1. Thayabaranathan T, Kim J, Cadilhac DA, Thrift AG, Donnan GA, Howard G, et al. Global stroke statistics 2022. Int J Stroke. 2022; 17(9):946–956. PMID:
35975986.
2. Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, et al. Heart disease and stroke statistics-2022 update: a report from the American Heart Association. Circulation. 2022; 145(8):e153–e639. PMID:
35078371.
3. Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, Lombardi-Hill D, et al. 2021 Guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021; 52(7):e364–e467. PMID:
34024117.
4. Ko SB, Park HK, Kim BM, Heo JH, Rha JH, Kwon SU, et al. 2019 Update of the Korean clinical practice guidelines of stroke for endovascular recanalization therapy in patients with acute ischemic stroke. J Stroke. 2019; 21(2):231–240. PMID:
30991800.
5. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; 50(12):e344–e418. PMID:
31662037.
6. Katsanos AH, Palaiodimou L, Zand R, Yaghi S, Kamel H, Navi BB, et al. Changes in stroke hospital care during the COVID-19 pandemic: a systematic review and meta-analysis. Stroke. 2021; 52(11):3651–3660. PMID:
34344166.
7. Bae HJ. CRCS-K Investigators. David G. Sherman Lecture Award: 15-year experience of the nationwide multicenter stroke registry in Korea. Stroke. 2022; 53(9):2976–2987. PMID:
35899613.
8. Kim BJ, Park JM, Kang K, Lee SJ, Ko Y, Kim JG, et al. Case characteristics, hyperacute treatment, and outcome information from the clinical research center for stroke-fifth division registry in South Korea. J Stroke. 2015; 17(1):38–53. PMID:
25692106.
9. Park JH, Kim BJ, Yoon CW, Rha JH, Heo JH, Kwon SU. Current status and issues of acute stroke management in Korea: results of a nationwide acute stroke care hospital survey. J Korean Neurol Assoc. 2019; 37(1):38–46.
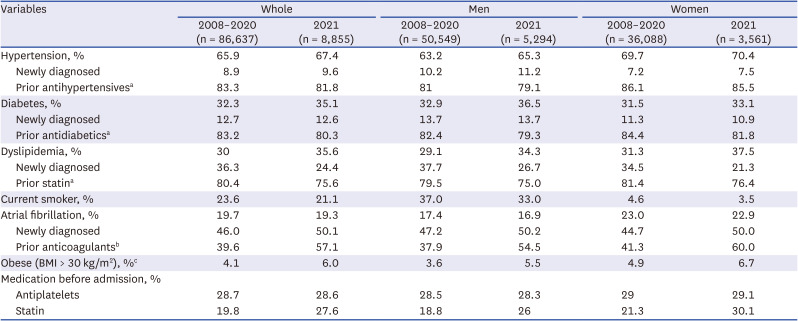
10. Park TH, Ko Y, Lee SJ, Lee KB, Lee J, Han MK, et al. Gender differences in the age-stratified prevalence of risk factors in Korean ischemic stroke patients: a nationwide stroke registry-based cross-sectional study. Int J Stroke. 2014; 9(6):759–765. PMID:
24148312.
11. Hajdu SD, Pittet V, Puccinelli F, Ben Hassen W, Ben Maacha M, Blanc R, et al. Acute stroke management during the COVID-19 pandemic: does confinement impact eligibility for endovascular therapy? Stroke. 2020; 51(8):2593–2596. PMID:
32716828.
12. Richter D, Eyding J, Weber R, Bartig D, Grau A, Hacke W, et al. A full year of the COVID-19 pandemic with two infection waves and its impact on ischemic stroke patient care in Germany. Eur J Neurol. 2022; 29(1):105–113. PMID:
34370900.
13. Siegler JE, Zha AM, Czap AL, Ortega-Gutierrez S, Farooqui M, Liebeskind DS, et al. Influence of the COVID-19 pandemic on treatment times for acute ischemic stroke: the Society of Vascular and Interventional Neurology Multicenter Collaboration. Stroke. 2021; 52(1):40–47. PMID:
33250041.
14. Xu X, Xiao Y, Li J, Chen L, Lin G, Dong L, et al. Decrease in intravenous thrombolysis and poor short-term functional prognosis for acute ischemic stroke during the COVID-19 pandemic. J Neurol. 2022; 269(2):597–602. PMID:
34379199.
15. Teo KC, Leung WC, Wong YK, Liu RK, Chan AH, Choi OM, et al. Delays in stroke onset to hospital arrival time during COVID-19. Stroke. 2020; 51(7):2228–2231. PMID:
32432998.
16. Cho Y, Yeo IH, Lee DE, Kim JK. Coronavirus disease pandemic impact on emergency department visits for cardiovascular disease in Korea: a review. Medicine (Baltimore). 2023; 102(47):e35992. PMID:
38013376.
17. Na SK, Kim JH, Lee WY, Oh MR. Impact of the COVID-19 pandemic on admission and mortality among patients with severe emergency diseases at emergency departments in Korea in 2020: registry data from the National Emergency Department Information System. J Korean Med Sci. 2023; 38(30):e243. PMID:
37527913.
18. Seo AR, Lee WJ, Woo SH, Moon J, Kim D. Pre-hospital delay in patients with acute stroke during the initial phase of the coronavirus disease 2019 outbreak. J Korean Med Sci. 2022; 37(6):e47. PMID:
35166083.
19. Liu J, Zheng L, Cheng Y, Zhang S, Wu B, Wang D, et al. Trends in outcomes of patients with ischemic stroke treated between 2002 and 2016: insights from a Chinese cohort. Circ Cardiovasc Qual Outcomes. 2019; 12(12):e005610. PMID:
31830825.
20. Toyoda K, Yoshimura S, Nakai M, Koga M, Sasahara Y, Sonoda K, et al. Twenty-year change in severity and outcome of ischemic and hemorrhagic strokes. JAMA Neurol. 2022; 79(1):61–69. PMID:
34870689.
21. Hsieh CY, Wu DP, Sung SF. Trends in vascular risk factors, stroke performance measures, and outcomes in patients with first-ever ischemic stroke in Taiwan between 2000 and 2012. J Neurol Sci. 2017; 378:80–84. PMID:
28566185.
22. Japan Stroke Data Bank. Japan Stroke Data Bank Report 2023. Osaka, Japan: National Cerebral and Cardiovascular Center;2023.
23. Ziaeian B, Xu H, Matsouaka RA, Xian Y, Khan Y, Schwamm LS, et al. US surveillance of acute ischemic stroke patient characteristics, care quality, and outcomes for 2019. Stroke. 2022; 53(11):3386–3393. PMID:
35862201.
24. RiksStroke Steering Group. RIKSSTROKE Annual Report 2022. Umeå, Sweden: RiksStroke Steering Group;2023.
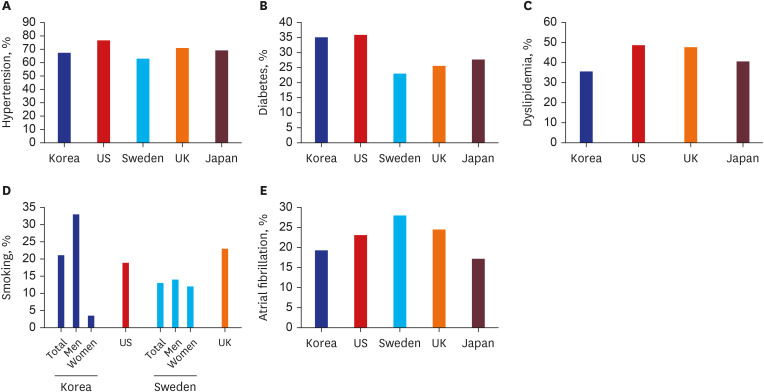
25. Cornelius ME, Loretan CG, Jamal A, Davis Lynn BC, Mayer M, Alcantara IC, et al. Tobacco product use among adults - United States, 2021. MMWR Morb Mortal Wkly Rep. 2023; 72(18):475–483. PMID:
37141154.
26. National Center for Health Statistics. NCHS Fact Sheet. Hyattsville, MD, USA: National Center for Health Statistics;2020.
27. Kim S, Choi S, Kim J, Park S, Kim YT, Park O, et al. Trends in health behaviors over 20 years: findings from the 1998-2018 Korea National Health and Nutrition Examination Survey. Epidemiol Health. 2021; 43:e2021026. PMID:
33872483.
28. Seo E, Jung S, Lee H, Kim HC. Sex-specific trends in the prevalence of hypertension and the number of people with hypertension: analysis of the Korea National Health and Nutrition Examination Survey (KNHANES) 1998-2018. Korean Circ J. 2022; 52(5):382–392. PMID:
35257521.
29. Chang Y, Kang HY, Lim D, Cho HJ, Khang YH. Long-term trends in smoking prevalence and its socioeconomic inequalities in Korea, 1992-2016. Int J Equity Health. 2019; 18(1):148. PMID:
31533732.
30. Rexrode KM, Madsen TE, Yu AY, Carcel C, Lichtman JH, Miller EC. The impact of sex and gender on stroke. Circ Res. 2022; 130(4):512–528. PMID:
35175851.
31. Madsen TE, Khoury JC, Leppert M, Alwell K, Moomaw CJ, Sucharew H, et al. Temporal trends in stroke incidence over time by sex and age in the GCNKSS. Stroke. 2020; 51(4):1070–1076. PMID:
32078459.
32. World Health Organization. Life Expectancy at Birth (years). Geneva, Switzerland: World Health Organization;2023.
33. Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Results. Seattle, WA, USA: Institute for Health Metrics and Evaluation (IHME);2020.
34. Omama S, Ogasawara K, Inoue Y, Ishibashi Y, Ohsawa M, Onoda T, et al. Ten-year cerebrovascular disease trend occurrence by population-based stroke registry in an aging Japan local prefecture. J Stroke Cerebrovasc Dis. 2020; 29(3):104580. PMID:
31879137.
35. Wafa HA, Wolfe CD, Bhalla A, Wang Y. Long-term trends in death and dependence after ischaemic strokes: a retrospective cohort study using the South London Stroke Register (SLSR). PLoS Med. 2020; 17(3):e1003048. PMID:
32163411.
36. Yafasova A, Fosbøl EL, Christiansen MN, Vinding NE, Andersson C, Kruuse C, et al. Time trends in incidence, comorbidity, and mortality of ischemic stroke in Denmark (1996-2016). Neurology. 2020; 95(17):e2343–e2353. PMID:
32817180.
37. Wangqin R, Laskowitz DT, Wang Y, Li Z, Wang Y, Liu L, et al. International comparison of patient characteristics and quality of care for ischemic stroke: analysis of the China National Stroke Registry and the American Heart Association Get With The Guidelines--Stroke Program. J Am Heart Assoc. 2018; 7(20):e010623. PMID:
30371291.
38. Cho SMJ, Lee H, Lee HH, Baek J, Heo JE, Joo HJ, et al. Dyslipidemia fact sheets in Korea 2020: an analysis of nationwide population-based data. J Lipid Atheroscler. 2021; 10(2):202–209. PMID:
34095012.
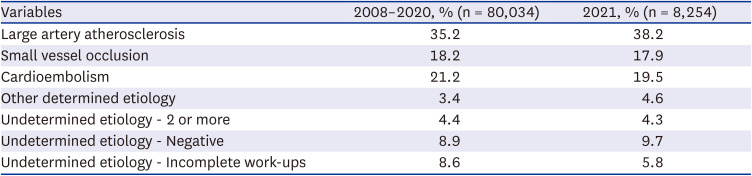
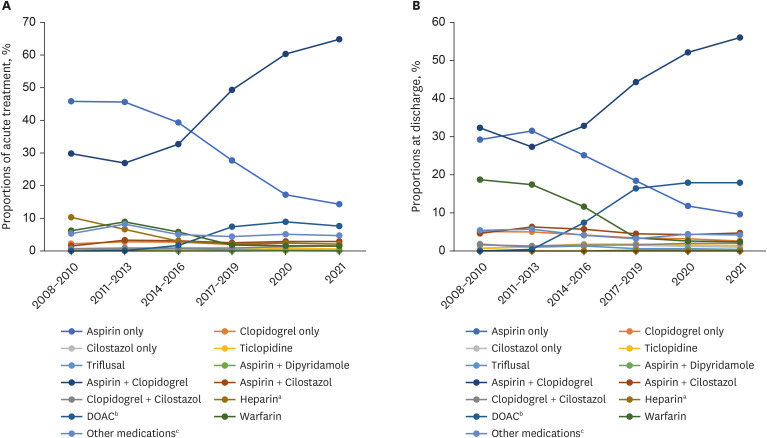
39. Lee SR, Choi EK, Han KD, Cha MJ, Oh S, Lip GY. Temporal trends of antithrombotic therapy for stroke prevention in Korean patients with non-valvular atrial fibrillation in the era of non-vitamin K antagonist oral anticoagulants: a nationwide population-based study. PLoS One. 2017; 12(12):e0189495. PMID:
29261716.
40. Park J, Jung JH, Choi EK, Lee SW, Kwon S, Lee SR, et al. Longitudinal patterns in antithrombotic therapy in patients with atrial fibrillation after percutaneous coronary intervention in the non-vitamin K oral anticoagulant era: a nationwide population-based study. J Clin Med. 2021; 10(7):1505. PMID:
33916604.
41. Lyrer F, Zietz A, Seiffge DJ, Koga M, Volbers B, Wilson D, et al. Atrial fibrillation detected before or after stroke: role of anticoagulation. Ann Neurol. 2023; 94(1):43–54. PMID:
36975022.
42. Howard VJ, Madsen TE, Kleindorfer DO, Judd SE, Rhodes JD, Soliman EZ, et al. Sex and race differences in the association of incident ischemic stroke with risk factors. JAMA Neurol. 2019; 76(2):179–186. PMID:
30535250.
43. Grau AJ, Weimar C, Buggle F, Heinrich A, Goertler M, Neumaier S, et al. Risk factors, outcome, and treatment in subtypes of ischemic stroke: the German Stroke Data Bank. Stroke. 2001; 32(11):2559–2566. PMID:
11692017.
44. An S, Ahn C, Jang J, Lee J, Kang D, Lee JK, et al. Comparison of the prevalence of cardiometabolic disorders and comorbidities in Korea and the United States: analysis of the National Health and Nutrition Examination Survey. J Korean Med Sci. 2022; 37(18):e149. PMID:
35535376.
45. Turin TC, Kita Y, Rumana N, Nakamura Y, Takashima N, Ichikawa M, et al. Ischemic stroke subtypes in a Japanese population: Takashima Stroke Registry, 1988-2004. Stroke. 2010; 41(9):1871–1876. PMID:
20689083.
46. Bogiatzi C, Hackam DG, McLeod AI, Spence JD. Secular trends in ischemic stroke subtypes and stroke risk factors. Stroke. 2014; 45(11):3208–3213. PMID:
25213343.
47. Sedova P, Brown RD, Zvolsky M, Belaskova S, Volna M, Baluchova J, et al. Incidence of stroke and ischemic stroke subtypes: a community-based study in Brno, Czech Republic. Cerebrovasc Dis. 2021; 50(1):54–61. PMID:
33302276.
48. Kim JS, Bonovich D. Research on intracranial atherosclerosis from the east and west: why are the results different? J Stroke. 2014; 16(3):105–113. PMID:
25328869.
49. Ko Y, Lee S, Chung JW, Han MK, Park JM, Kang K, et al. MRI-based algorithm for acute ischemic stroke subtype classification. J Stroke. 2014; 16(3):161–172. PMID:
25328874.
50. Hurford R, Wolters FJ, Li L, Lau KK, Küker W, Rothwell PM, et al. Prevalence, predictors, and prognosis of symptomatic intracranial stenosis in patients with transient ischaemic attack or minor stroke: a population-based cohort study. Lancet Neurol. 2020; 19(5):413–421. PMID:
32333899.
51. Richter D, Weber R, Eyding J, Bartig D, Misselwitz B, Grau A, et al. Acute ischemic stroke care in Germany - further progress from 2016 to 2019. Neurol Res Pract. 2021; 3(1):14. PMID:
33789773.
52. Committee CSBPSQA. Ontario Stroke Report FY 2019-20. 2021.
53. Camporesi J, Strumia S, Di Pilla A, Paolucci M, Orsini D, Assorgi C, et al. Stroke pathway performance assessment: a retrospective observational study. BMC Health Serv Res. 2023; 23(1):1391. PMID:
38082226.
54. Olavarría VV, Hoffmeister L, Vidal C, Brunser AM, Hoppe A, Lavados PM. Temporal trends of intravenous thrombolysis utilization in acute ischemic stroke in a prospective cohort from 1998 to 2019: modeling based on joinpoint regression. Front Neurol. 2022; 13:851498. PMID:
35463124.
55. Japan Stroke Data Bank. Japan Stroke Data Bank Report 2021. Osaka, Japan: National Cerebral and Cardiovascular Center;2021.
56. American Stroke Association. Target: Stroke Phase III Campaign Manual. Columbus, OH, USA: American Stroke Association;2019.
57. Rohde S, Weber W, Berlis A, Urbach H, Reimer P, Schramm P, et al. Acute endovascular stroke treatment in Germany in 2019 : results from a nationwide database. Clin Neuroradiol. 2021; 31(1):11–19. PMID:
33481050.
58. Kim Y, Lee S, Abdelkhaleq R, Lopez-Rivera V, Navi B, Kamel H, et al. Utilization and availability of advanced imaging in patients with acute ischemic stroke. Circ Cardiovasc Qual Outcomes. 2021; 14(4):e006989. PMID:
33757311.
59. Kim HC, Lee H, Lee HH, Lee G, Kim E, Song M, et al. Korea hypertension fact sheet 2022: analysis of nationwide population-based data with a special focus on hypertension in the elderly. Clin Hypertens. 2023; 29(1):22. PMID:
37580841.
60. Rizos T, Jenetzky E, Nabavi DG, Haeusler KG, Wachter R, Ossenbrink M, et al. Echocardiography in acute stroke patients: a nationwide analysis in departments with certified stroke units in Germany. Neurol Res Pract. 2023; 5(1):3. PMID:
36653887.
61. Edwards JD, Kapral MK, Fang J, Saposnik G, Gladstone DJ. Investigators of the Registry of the Canadian Stroke Network. Underutilization of ambulatory ECG monitoring after stroke and transient ischemic attack: missed opportunities for atrial fibrillation detection. Stroke. 2016; 47(8):1982–1989. PMID:
27406109.
62. Xian Y, Xu H, Matsouaka R, Laskowitz DT, Maisch L, Hannah D, et al. Analysis of prescriptions for dual antiplatelet therapy after acute ischemic stroke. JAMA Netw Open. 2022; 5(7):e2224157. PMID:
35900761.
63. Fischer U, Koga M, Strbian D, Branca M, Abend S, Trelle S, et al. Early versus later anticoagulation for stroke with atrial fibrillation. N Engl J Med. 2023; 388(26):2411–2421. PMID:
37222476.
64. Ovbiagele B, Schwamm LH, Smith EE, Hernandez AF, Olson DM, Pan W, et al. Recent nationwide trends in discharge statin treatment of hospitalized patients with stroke. Stroke. 2010; 41(7):1508–1513. PMID:
20508182.
65. Heo JH, Song D, Nam HS, Kim EY, Kim YD, Lee KY, et al. Effect and safety of rosuvastatin in acute ischemic stroke. J Stroke. 2016; 18(1):87–95. PMID:
26846760.
66. Amarenco P, Kim JS, Labreuche J, Charles H, Abtan J, Béjot Y, et al. A comparison of two LDL cholesterol targets after ischemic stroke. N Engl J Med. 2020; 382(1):9–19. PMID:
31738483.
67. Park HK, Lee JS, Hong KS, Cho YJ, Park JM, Kang K, et al. Statin therapy in acute cardioembolic stroke with no guidance-based indication. Neurology. 2020; 94(19):e1984–e1995. PMID:
32273430.
68. Oravec CS, Tschoe C, Fargen KM, Kittel CA, Spiotta A, Almallouhi E, et al. Trends in mechanical thrombectomy and decompressive hemicraniectomy for stroke: a multicenter study. Neuroradiol J. 2022; 35(2):170–176. PMID:
34269121.
69. Göttsche J, Flottmann F, Jank L, Thomalla G, Rimmele DL, Czorlich P, et al. Decompressive craniectomy in malignant MCA infarction in times of mechanical thrombectomy. Acta Neurochir (Wien). 2020; 162(12):3147–3152. PMID:
31879817.
70. Seners P, Turc G, Oppenheim C, Baron JC. Incidence, causes and predictors of neurological deterioration occurring within 24 h following acute ischaemic stroke: a systematic review with pathophysiological implications. J Neurol Neurosurg Psychiatry. 2015; 86(1):87–94. PMID:
24970907.
71. Liu H, Liu K, Zhang K, Zong C, Yang H, Li Y, et al. Early neurological deterioration in patients with acute ischemic stroke: a prospective multicenter cohort study. Ther Adv Neurol Disorder. 2023; 16:17562864221147743.
72. Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014; 384(9958):1929–1935. PMID:
25106063.
73. Seet RC, Rabinstein AA. Symptomatic intracranial hemorrhage following intravenous thrombolysis for acute ischemic stroke: a critical review of case definitions. Cerebrovasc Dis. 2012; 34(2):106–114. PMID:
22868870.
74. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372(1):11–20. PMID:
25517348.
75. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; 372(24):2296–2306. PMID:
25882510.
76. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018; 378(1):11–21. PMID:
29129157.
77. Yoshimura S, Sakai N, Yamagami H, Uchida K, Beppu M, Toyoda K, et al. Endovascular therapy for acute stroke with a large ischemic region. N Engl J Med. 2022; 386(14):1303–1313. PMID:
35138767.
78. van der Steen W, van der Ende NAM, van Kranendonk KR, Chalos V, van Oostenbrugge RJ, van Zwam WH, et al. Determinants of symptomatic intracranial hemorrhage after endovascular stroke treatment: a retrospective cohort study. Stroke. 2022; 53(9):2818–2827. PMID:
35674042.
79. Rücker V, Heuschmann PU, O’Flaherty M, Weingärtner M, Hess M, Sedlak C, et al. Twenty-year time trends in long-term case-fatality and recurrence rates after ischemic stroke stratified by etiology. Stroke. 2020; 51(9):2778–2785. PMID:
32811383.
80. Skajaa N, Adelborg K, Horváth-Puhó E, Rothman KJ, Henderson VW, Thygesen LC, et al. Risks of stroke recurrence and mortality after first and recurrent strokes in Denmark: a nationwide registry study. Neurology. 2022; 98(4):e329–e342. PMID:
34845054.
81. Leifheit EC, Wang Y, Goldstein LB, Lichtman JH. Trends in 1-year recurrent ischemic stroke in the US Medicare fee-for-service population. Stroke. 2022; 53(11):3338–3347. PMID:
36214126.
82. Sennfält S, Norrving B, Petersson J, Ullberg T. Long-term survival and function after stroke: a longitudinal observational study from the Swedish Stroke Register. Stroke. 2019; 50(1):53–61. PMID:
30580719.
83. Bettger JP, Thomas L, Liang L, Xian Y, Bushnell CD, Saver JL, et al. Hospital variation in functional recovery after stroke. Circ Cardiovasc Qual Outcomes. 2017; 10(1):e002391. PMID:
28096203.
84. Ganesh A, Luengo-Fernandez R, Wharton RM, Rothwell PM. Oxford Vascular Study. Ordinal vs dichotomous analyses of modified Rankin Scale, 5-year outcome, and cost of stroke. Neurology. 2018; 91(21):e1951–e1960. PMID:
30341155.
85. Marko M, Miksova D, Ebner J, Lang M, Serles W, Sommer P, et al. Temporal trends of functional outcome in patients with acute ischemic stroke treated with intravenous thrombolysis. Stroke. 2022; 53(11):3329–3337. PMID:
36000395.
86. Rodrigues FB, Neves JB, Caldeira D, Ferro JM, Ferreira JJ, Costa J. Endovascular treatment versus medical care alone for ischaemic stroke: systematic review and meta-analysis. BMJ. 2016; 353:i1754. PMID:
27091337.
87. RiksStroke Steering Group. RIKSSTROKE Annual Report 2011. Umeå, Sweden: RiksStroke Steering Group;2012.
88. Bushnell CD, Chaturvedi S, Gage KR, Herson PS, Hurn PD, Jiménez MC, et al. Sex differences in stroke: challenges and opportunities. J Cereb Blood Flow Metab. 2018; 38(12):2179–2191. PMID:
30114967.
89. Petty GW, Brown RD Jr, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO. Ischemic stroke subtypes : a population-based study of functional outcome, survival, and recurrence. Stroke. 2000; 31(5):1062–1068. PMID:
10797166.
90. Caso V, Paciaroni M, Agnelli G, Corea F, Ageno W, Alberti A, et al. Gender differences in patients with acute ischemic stroke. Womens Health (Lond Engl). 2010; 6(1):51–57. PMID:
20088729.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download