INTRODUCTION
A previous meta-analysis, which included articles across all World Health Organization (WHO) regions, reported that the overall global incidence of traumatic spinal cord injury (TSCI) was 10.5 cases per 100,000 persons, which is equivalent to 768,473 new cases of TSCI annually.
1 From East Asian countries, a previous nationwide survey in Japan suggested that the annual incidence of TSCI in 2018 was 49 per million.
2 In a population-based study in Taiwan, the average incidence of TSCI from 2000 to 2003 was 61.61 cases per 100,000 persons.
3 In mainland China, the number of patients with spinal trauma from 2001 to 2007 was 82,720 cases per million according to the Chinese Database of Trauma.
4 However, each of these previous studies had limitations, such as using a survey rather than medical records,
2 having a short follow-up period,
3 or using data collected only from military hospitals rather than all hospitals nationwide.
4 These limitations make it unclear whether the statistical data of incidence includes all patients with TSCI without omission.
Globally, only few countries have national health insurance and provide universal health coverage. However, even in countries with national health insurance, the medical systems and coverage for trauma patients is different from country to country, for instance, the German Statutory Accident Insurance,
5 Swiss Accident Insurance,
6 and State Insurance Regulatory Agency in the Australian state of New South Wales.
7 In this regard, South Korea has one of the best national health insurance systems in the world. South Korea provides universal medical coverage to all citizens without omission, from birth to death, through the national health insurance system.
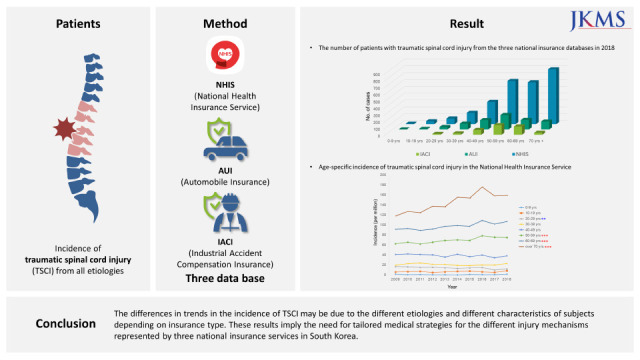
South Korea has three national or quasi-national insurance systems for trauma patients according to the cause of injuries. The National Health Insurance Service (NHIS) is the main national health insurance. The NHIS is a mandatory social insurance benefit scheme that covers the entire South Korean population, consisting of over 50 million individuals.
8 The NHIS provides lifelong coverage to trauma patients who were injured in daily life.
9 On the contrary, trauma patients who were injured in the workplace are covered by the Industrial Accident Compensation Insurance (IACI; the official name of the “Korea Workers’ Compensation & Welfare Service”). The IACI is also a mandatory national insurance system applied to all companies in South Korea, where one or more workers are employed
10; approximately 98% of the workers are covered by the IACI.
11 Finally, trauma patients who were injured by traffic accidents are covered by automobile insurances (AUI). Although all AUIs in South Korea are private insurance, they each share common characteristics with the national insurance system, since they are compulsory for all car owners. Considering that TSCI has various etiologies and mechanisms such as traffic and industrial accidents, AUI and IACI databases are essentially needed in addition to the NHIS database to investigate the incidence of TSCI in South Korea. However, the incidence of TSCI from various national insurance databases has not been explored yet, not only in South Korea, but also worldwide. Therefore, this study provides significant implications as we examined the incidences of TSCI, according to the cause of injuries, based on the three nationwide insurance databases in South Korea. This study aimed to report the incidences of TSCI and compare the trends in the incidence of TSCI across the NHIS, AUI, and IACI insurance databases.
METHODS
Data sources
We analyzed three nationwide insurance databases in South Korea, namely, NHIS, IACI, and AUI. Trauma patients can receive general medical coverage, such as inpatient or outpatient care, from NHIS, IACI, or AUI according to their cause of injuries. Because these three insurances are mutually exclusive, patients cannot be covered by more than one insurance simultaneously for the same diagnosis. For example, a patient with TSCI due to a traffic accident can only be covered by AUI, but not by the national health insurance simultaneously. All these three databases contain common information on the date of discharge and discharge diagnoses (both principal and additional diagnoses) assigned by a clinician at discharge according to the International Classification of Diseases, 10th revision (ICD-10).
Definition of TSCI and study population
We defined patients with TSCI as those admitted to the hospital with a diagnosis of TSCI according to the ICD-10 criteria. In the NHIS and AUI data, 1) patients diagnosed with TSCI (S14.0, S14.1, S14.6, S24.0, S24.1, S24.6, S34.0, S34.1, S34.6, T06.0, T06.1, T09.3, and T91.3) as a principal diagnosis or 2) patients diagnosed with vertebral fractures (S22.0, S22.1, S32.0, M48.4, and M48.5) as a principal diagnosis, and additional TSCI diagnosis within the top four minor diagnoses were included as the study population. In the IACI data, all patients diagnosed with TSCI were included as the study population since the principal and additional diagnoses are not distinctly defined. The NHIS data were reviewed between 2009 and 2018 as a main insurance database, and the AUI and IACI data were reviewed between 2014 and 2018 as additional insurance databases. Only patients who were newly diagnosed with TSCI on first admission during the study period were included to avoid duplicate counting of one person in each year.
The injured body regions of TSCI patients were classified according to the ICD-10 codes: cervical spinal cord injury (S14.0, S14.1, S14.6, and T06.0), thoracic spinal cord injury (S24.0, S24.1, and S24.6), lumbar spinal cord injury (S34.0, S34.1, and S34.6), multiple spinal cord injury (T06.1), and unspecified spinal cord injury (T09.3 and T91.3).
Statistical analysis
The crude incidence in the NHIS and AUI data was calculated using the annual number of TSCI cases divided by the mid-year population estimates. The mid-year population estimates were obtained from the annual resident population data from the Korea National Statistical Office (
http://www.kosis.kr). On the other hand, the crude incidence in the IACI data was calculated by dividing the annual number of TSCI cases by the number of workers insured by IACI in the same year. The number of workers insured by IACI was obtained from the public data provided by the Korea Worker’s Compensation and Welfare Service (
http://www.data.go.kr). The age-specific incidence was calculated by dividing the number of cases in each 10-year age group by the total number of subjects in that age group. Age-adjusted incidence was calculated using direct standardization by applying the 2005 South Korean population or using the 2000 US population as a standard population. The annual percentage changes (APC) of TSCI incidence were calculated using Joinpoint regression analysis.
12 Cochrane-Armitage trend test was performed to test the trends of TSCI incidence according to injured body regions.
SAS version 9.4 statistical software (SAS Institute, Cary, NC, USA) was used for statistical analysis. The Cochrane-Armitage trend test was conducted using R version 4.0.1 (R Development Core Team, Vienna, Austria). APCs were calculated using Joinpoint Regression Program version 4.9.0.0 (National Cancer Institute, Bethesda, MD, USA). All reported P values are two-sided. Statistical significance was set at P < 0.05.
Ethics statement
The requirement for ethical approval for this study was waived by the Institutional Review Board (IRB) of Seoul National University Hospital, Seoul, South Korea (IRB No. E-2011-004-1168). The requirement for informed consent was also waived because all data in the NHIS, IACI, and AUI were anonymized and de-identified.
RESULTS
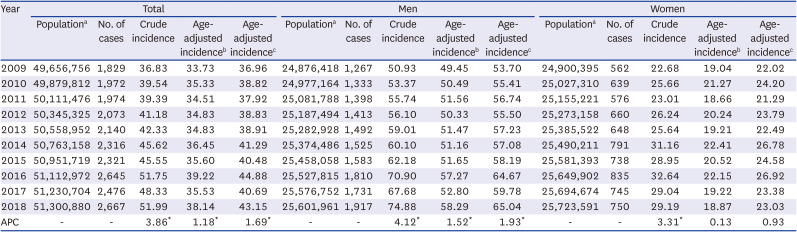
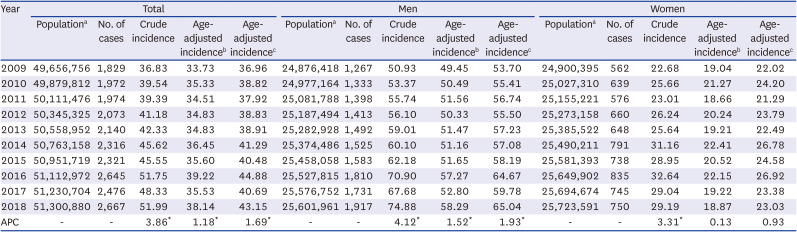
Table 1 presents the annual incidence of TSCI in the NHIS data of South Korea between 2009 and 2018. The crude incidence of TSCI in the overall population increased continuously during the study period (from 36.83 per million in 2009 to 51.99 per million in 2018). The APC was 3.9%, which was significant (
P < 0.001). The age-adjusted incidence with the standard population of South Korea also increased (from 33.73 per million in 2009 to 38.14 per million in 2018) with significant APC (APC = 1.2%,
P = 0.014). The age-adjusted incidence with the standard population of the US also showed similar results. After stratification by sex, crude incidence and age-adjusted incidence were higher in men than in women throughout the study period. In men, crude incidence and age-adjusted incidence increased significantly (APC of crude incidence = 4.1%,
P < 0.001; APC of age-adjusted incidence = 1.5%,
P = 0.005). In women, only crude incidence increased with significance (APC = 3.3%,
P = 0.005). The age-adjusted incidence using the US standard population also presented similar results.
Supplementary Table 1 displays the annual incidence of TSCI in the AUI database between 2014 and 2018. The age-adjusted incidence decreased from 13.88 per million in 2014 to 11.57 per million in 2018, and the APC was also significant (APC = −5.1%,
P = 0.009). The age-adjusted incidence of TSCI was higher in men, and significantly decreased only in men. In the IACI database, the age-adjusted incidence showed no significant trend, while the crude incidence showed a significant increase (from 22.02 per million in 2014 to 28.92 per million in 2018, APC = 6.1%,
P = 0.038) (
Supplementary Table 2). After stratification by sex, the crude incidence was higher in men, and significant increases were found in both men and women.
Table 1
Annual incidence of traumatic spinal cord injury in patients (per million) in South Korea’s National Health Insurance Service database
|
Year |
Total |
Men |
Women |
|
Populationa
|
No. of cases |
Crude incidence |
Age-adjusted incidenceb
|
Age-adjusted incidencec
|
Populationa
|
No. of cases |
Crude incidence |
Age-adjusted incidenceb
|
Age-adjusted incidencec
|
Populationa
|
No. of cases |
Crude incidence |
Age-adjusted incidenceb
|
Age-adjusted incidencec
|
|
2009 |
49,656,756 |
1,829 |
36.83 |
33.73 |
36.96 |
24,876,418 |
1,267 |
50.93 |
49.45 |
53.70 |
24,900,395 |
562 |
22.68 |
19.04 |
22.02 |
|
2010 |
49,879,812 |
1,972 |
39.54 |
35.33 |
38.82 |
24,977,164 |
1,333 |
53.37 |
50.49 |
55.41 |
25,027,310 |
639 |
25.66 |
21.27 |
24.20 |
|
2011 |
50,111,476 |
1,974 |
39.39 |
34.51 |
37.92 |
25,081,788 |
1,398 |
55.74 |
51.56 |
56.74 |
25,155,221 |
576 |
23.01 |
18.66 |
21.29 |
|
2012 |
50,345,325 |
2,073 |
41.18 |
34.83 |
38.83 |
25,187,494 |
1,413 |
56.10 |
50.33 |
55.50 |
25,273,158 |
660 |
26.24 |
20.24 |
23.79 |
|
2013 |
50,558,952 |
2,140 |
42.33 |
34.83 |
38.91 |
25,282,928 |
1,492 |
59.01 |
51.47 |
57.23 |
25,385,522 |
648 |
25.64 |
19.21 |
22.49 |
|
2014 |
50,763,158 |
2,316 |
45.62 |
36.45 |
41.29 |
25,374,486 |
1,525 |
60.10 |
51.16 |
57.08 |
25,490,211 |
791 |
31.16 |
22.41 |
26.78 |
|
2015 |
50,951,719 |
2,321 |
45.55 |
35.60 |
40.48 |
25,458,058 |
1,583 |
62.18 |
51.65 |
58.19 |
25,581,393 |
738 |
28.95 |
20.52 |
24.58 |
|
2016 |
51,112,972 |
2,645 |
51.75 |
39.22 |
44.88 |
25,527,815 |
1,810 |
70.90 |
57.27 |
64.67 |
25,649,902 |
835 |
32.64 |
22.15 |
26.92 |
|
2017 |
51,230,704 |
2,476 |
48.33 |
35.53 |
40.69 |
25,576,752 |
1,731 |
67.68 |
52.80 |
59.78 |
25,694,674 |
745 |
29.04 |
19.22 |
23.38 |
|
2018 |
51,300,880 |
2,667 |
51.99 |
38.14 |
43.15 |
25,601,961 |
1,917 |
74.88 |
58.29 |
65.04 |
25,723,591 |
750 |
29.19 |
18.87 |
23.03 |
|
APC |
- |
- |
3.86*
|
1.18*
|
1.69*
|
- |
- |
4.12*
|
1.52*
|
1.93*
|
- |
- |
3.31*
|
0.13 |
0.93 |

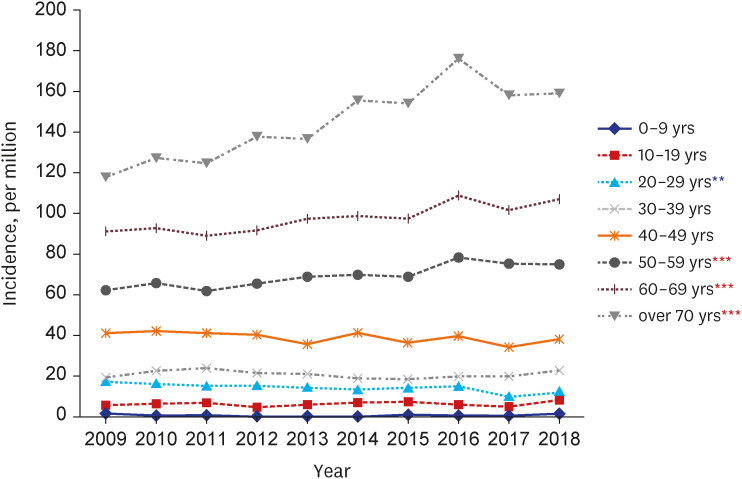
Fig. 1 shows the age-specific incidence of TSCI according to age groups in the NHIS database. Between 2009 and 2018, the age-specific incidence of TSCI was the highest for those in their 70s or older. The age-specific incidence significantly decreased for those in the 20s (APC = −4.2%,
P = 0.005), whereas it showed a significant increase for those in their 50s, 60s, and 70s or older (50s APC = 2.5%,
P < 0.001; 60s APC = 2.0%,
P = 0.001; 70s APC = 4.0%,
P < 0.001). In the AUI database, between 2014 and 2018, the age-specific incidence of TSCI was the highest for those in their 50s and 60s, and significantly decreased for those in their 10s and 40s (10s APC = – 22.3%,
P = 0.002; 40s APC = −8.0%,
P = 0.038) (
Supplementary Fig. 1). In the IACI database, the age-specific incidence of TSCI for those in their 60s was the highest during the study periods, and increased significantly for those in their 70s or older (APC = 40.4%,
P = 0.007) (
Supplementary Fig. 1).
Fig. 1
Age-specific incidence of traumatic spinal cord injury in the National Health Insurance Service database from 2009 to 2018.
*P < 0.05; **P < 0.01; ***P < 0.001.
Red asterisk indicates increased the annual percentage changes; Blue asterisk indicates decreased the annual percentage changes.
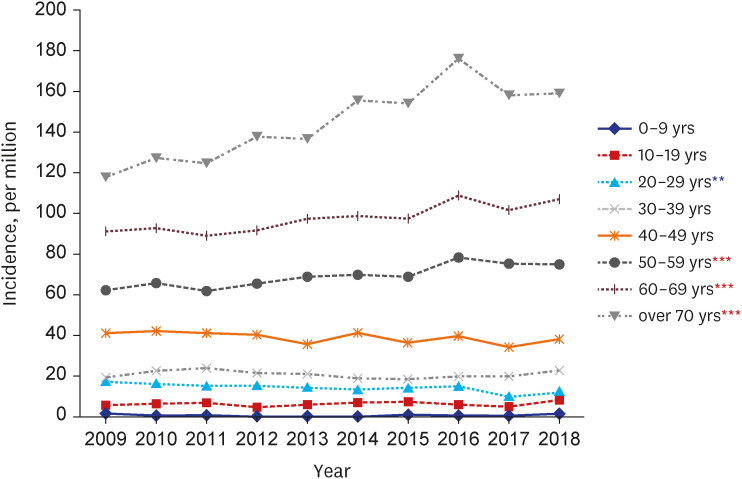

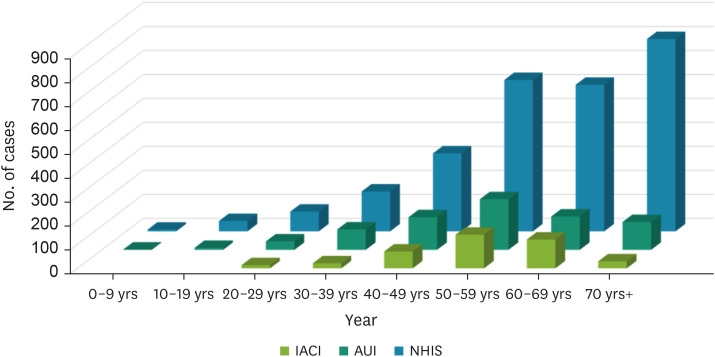
Fig. 2 presents the number of patients with TSCI according to age groups across the three insurance databases in South Korea in 2018. In the NHIS, the number of patients with TSCI was the highest among those over 70 years of age. In both AUI and IACI, the number of patients with TSCI was the highest in those in their 50s.
Fig. 2
Distribution of patients with traumatic spinal cord injury according to age groups across the three trauma-related insurance databases in 2018.
IACI = Industrial Accident Compensation Insurance, AUI = automobile insurance, NHIS = National Health Insurance Service.
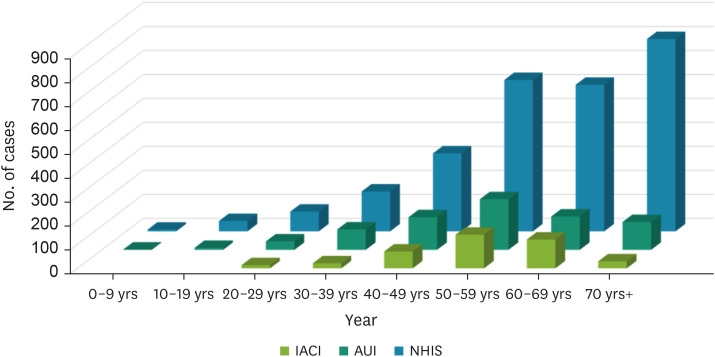

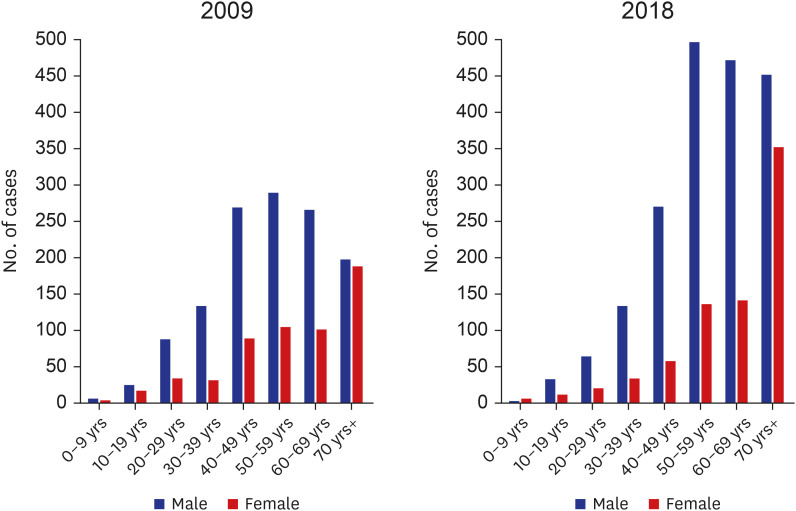
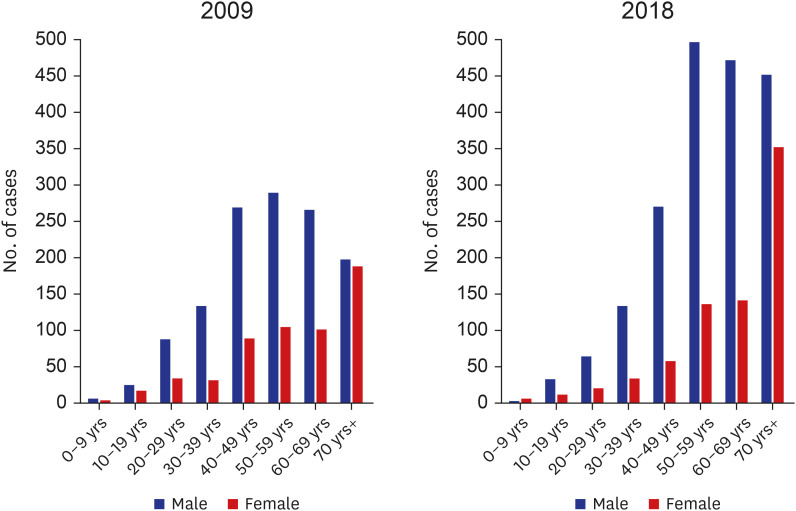
Fig. 3 displays the number of patients with TSCI according to sex and age groups in the NHIS data for 2009 and 2018, respectively. In men, the number of patients with TSCI was the highest in the 40−60 years old group in 2009; however, in 2018, the highest number of patients with TSCI was observed in the 50−70 years old group with double the number of patients than that 10 years ago. In women, the number of patients with TSCI over 70 years of age was the highest in both 2009 and 2018. In 2018, the number of patients with TSCI over 70 years of age was more than twice than that in 2009.
Supplementary Fig. 2 presents the number of patients with TSCI according to sex and age groups in the AUI and IACI data in 2014 and 2018, respectively. In men, the number of patients with TSCI in their 40s and 50s was similarly high in 2014, but in 2018, the number of patients with TSCI in their 50s was the highest. Among women, similar patterns and numbers were observed between 2014 and 2018. In the IACI data, the number of patients in their 50s was the highest in 2014, followed by the number of patients in their 40s, while the number of patients in their 60s exceeded the number of patients in their 40s in 2018 (
Supplementary Fig. 2).
Fig. 3
Number of patients with traumatic spinal cord injury according to sex and age groups in the National Health Insurance Service databases in 2009 and 2018.

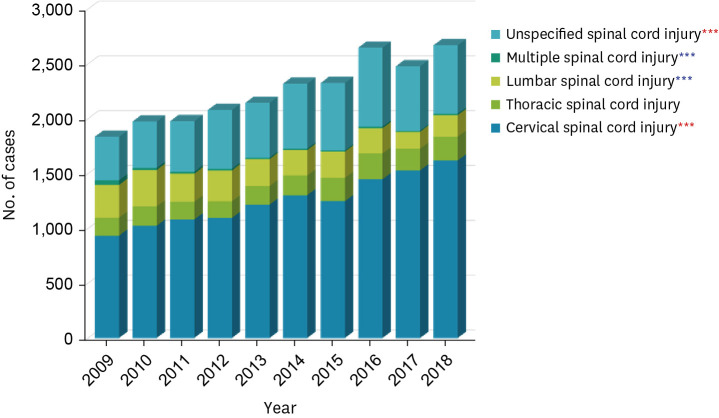
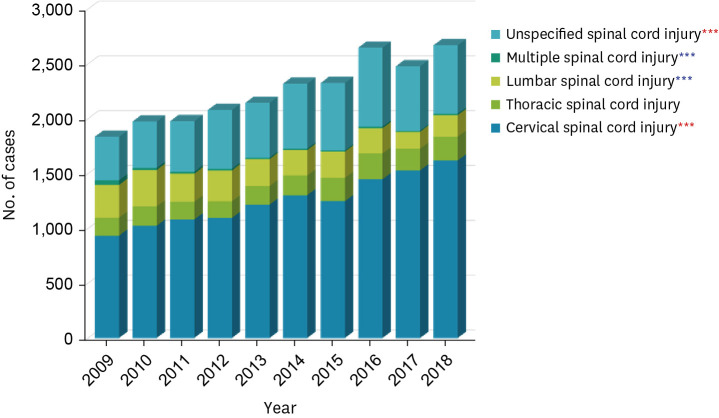
In
Fig. 4, we examined the distribution of injured body regions in patients with TSCI using the NHIS data. The proportion of patients with cervical spinal cord injury was the most common in all the three databases. Between 2009 and 2018, the number of patients with cervical spinal cord injury and those with unspecified spinal cord injury showed a significantly increasing trend, whereas the number of patients with lumbar spinal cord injury and multiple spinal cord injuries showed a significantly decreasing trend. In the AUI data from 2014 to 2018, the number of patients with thoracic spinal cord injury and lumbar spinal cord injury showed a significantly decreasing trend (
Supplementary Fig. 3). In the IACI data, the number of patients with unspecified spinal cord injury showed a significantly increasing trend (
Supplementary Fig. 3).
Fig. 4
Distribution of injured body regions in patients with traumatic spinal cord injury in the National Health Insurance Service databases from 2009 to 2018.
*P for trend < 0.05; **P for trend < 0.01; ***P for trend < 0.001.
Red asterisk indicates increased trend; Blue asterisk indicates decreased trend.

DISCUSSION
In this study, the age-adjusted incidence of TSCI in 2018 was 38.14, 11.57, and 26.87 cases per million in the NHIS, AUI, and IACI databases, respectively. We also found that the incidence of TSCI significantly increased in the NHIS and IACI databases, whereas it significantly decreased in the AUI database. Older patients in their 60s and 70s or older showed a high incidence of TSCI in all the three insurance databases compared to other age groups. In particular, the incidence of TSCI in those in their 70s or older dramatically increased in both the NHIS and IACI databases. In 2018, the number of patients with TSCI was the highest among those over 70 years of age in the NHIS database, whereas the number of patients with TSCI in their 50s was the highest in the AUI and IACI databases. The proportion of patients with cervical spinal cord injury was the most common in all the three databases.
Our results revealed that in the NHIS database, which covers the entire Korean population, the incidence of TSCI in those in their 70s or older significantly increased, and proportion of older patients was the most prevalent regardless of sex. A previous hospital-based study from the last three decades (1990–1999, 2000–2009, and 2010–2019) showed comparable results. Lee et al.
13 found that the mean age of patients with TSCI increased from 32.4 years in 1990s to 47.1 years in 2010s. During the three decades, the number of patients in the 46–60, 61–75, and 76 years or older age groups increased, whereas that in the under 15 and 16–30 years age groups decreased.
13 Another hospital-based study by Shin et al.
14 also reported that the mean age of patients with spinal cord injury, mainly TSCI, increased from 32.3 years to 43.6 years during the period from 1987–1996 to 2004–2008. The number of patients in the over 50 years age group increased significantly. Previous studies in other countries also have reported results that are consistent with our study findings. A population-based study using the Nationwide Inpatient Sample databases in the United States has presented that the highest increase in the incidence of acute TSCI was observed in older patients, significantly associated with an increase in falls.
15 A retrospective cohort study of the Victorian State Trauma Registry in Australia suggested that the increasing number of TSCI cases were noted in older adults.
16 Moreover, a population-based study from 11 Italian regions revealed an increase in the incidence among older individuals, with falls as the leading cause of TSCI.
17 Most previous studies have pointed out that the main traumatic cause of TSCI among older individuals was falls.
13151617 Etiologically, cervical ossification of the ligamentum flavum (COLF) also can be considered as a cause of TSCI among older individuals. A previous meta-analysis reported that COLF predominantly appeared in older populations, especially in East Asian countries.
6 Therefore, the underlying COLF in older patients may cause canal stenosis,
18 resulting in spinal cord injury after a traumatic accident.
Another noteworthy result in our study is that the proportion of cervical spinal cord injury was the highest and displayed increasing trend from the NHIS data (50.8% in 2009 to 60.6% in 2018). Similarly, previous studies by Lee et al.
13 and Shin et al.
14 also reported high proportions of tetraplegia (74.3% in 2010–2019 and 60.3% in 2004–2008, respectively), which is the equivalent anatomical injury level to cervical spinal cord injury. However, in our study and in Shin’s study, the proportions of cervical spinal cord injury or tetraplegia increased rapidly, whereas in Lee’s study, it increased slightly. This may be due to the different characteristics of each data. Since we used health insurance data, we were able to define the TSCI patients during initial diagnosis. However, unlike Shin's study, which used data from a tertiary general hospital, Lee’s study used data from a specialized rehabilitation hospital. In other words, there is a possibility that patients who died before being transferred to a specialized rehabilitation hospital or who were inactive during rehabilitation treatment were not included in the data. Therefore, it is presumed that the difference in the increase of cervical spinal cord injury was due to the different characteristics of the participants of each study.
According to a previous meta-analysis, the overall global incidence of TSCI across all WHO regions was 10.5 per 100,000 persons, which is equivalent to 768,473 new cases of TSCI annually.
1 When classified by WHO region, the incidence of TSCI ranged from 3.4 per 100,000 (95% confidence interval [CI], 1.8 to 6.6 cases/100,000) in Europe to 5.1 per 100,000 (95% CI, 1.4 to 19.0 cases/100,000) in the Americas (United States and Canada).
1 In the present study, the age-adjusted incidence of TSCI in South Korea was 4.3 per 100,000 in 2018, which is comparable with those in Europe and the Americas (United States and Canada). When the WHO regions were classified by income levels,
19 the incidence of TSCI and the pattern of injured body region in South Korea were close to those of high-income countries. The incidence of TSCI in low- to middle-income countries was 13.69 per 100,000 (95% CI, 6.39 to 20.98 cases/100,000) and that in high-income countries was 8.72 per 100,000 (95% CI, 6.56 to 10.88). Regarding the distribution of injured body regions, the proportion of patients with cervical spinal cord injury in high-income countries was 51.4%, and those in low- to middle- income countries were 41.9% and 37.3%, respectively. In the present study, the proportions of patients with cervical spinal cord injury in 2018 were 60.6%, 73.7%, and 60.1% in the NHIS, AUI, and IACI databases, respectively, which were even higher than those of other high-income countries.
The most notable strength of this study is that we examined the incidences of TSCI based on three nationwide insurance databases, namely, NHIS, AUI, and IACI. To date, several previous studies have reported the epidemiology of TSCI in South Korea. However, the previous studies were single hospital-based studies
1314 or studies using only health insurance data.
20 No previous studies have suggested the incidence of TSCI including all etiologies, on a nationwide scale, as this present study. The main etiology of TSCI can be classified by five categories, including land transport, work, falls, sports/recreations, and violence/self-harm.
19212223 The three insurance databases in this study can cover all these main etiologies of TSCI; the TSCI caused by land transport can be covered by AUI, work-related TSCI can be covered by IACI, and the rest, including falls, sports/recreations, and violence/self-harm, can be covered by the NHIS. As such, each of the databases has a different etiology as well as different insured subjects, which may result in different trends in the incidence of TSCI. In this study, we revealed that all the three databases had a high incidence of TSCI in those in their 60s and 70s or older. However, among those in their 70s or older, the incidence of TSCI sharply increased in the NHIS and IACI databases, while no significant increase was shown in AUI database. Therefore, in the NHIS and IACI, it is necessary to focus on early rehabilitation to reduce permanent disability for older TSCI patients who have a greatly increased number in this age group. On the other hand, in AUI, accidents can be prevented effectively by traffic policies; thus, improving the driving system should be a focus in order to decrease the incidence of TSCI in the older population.
This study has several limitations. First, although we compared the incidence of TSCI from each of the three insurance databases, the overall incidence of TSCI in South Korea could not be determined. We were not able to combine the three insurance databases into one database since each insurance database was owned by different institutions. Even though the three insurances are mutually exclusive, in the real world, it is impossible to identify patients who are illegally receiving two or more overlapping insurance coverage. For example, patients injured in an automobile accident or industrial accident may be illegally covered by the NHIS after the AUI or IACI coverage ends. In this case, the patient might be counted as duplicates in both insurance databases. Therefore, further research is needed to measure the overall incidence of TSCI in South Korea using a complete dataset that merges the data of all these three insurance databases. Second, the incidence based on the ICD-10 codes may have included some errors due to misclassification. Indeed, we found that the proportion of unspecified SCI for which the level of injury was not known accounted for almost 20% of cases in our study. According to the disease statistics provided by the Health Insurance Review & Assessment Service (HIRA), more than half of the hospitals that entered unspecified SCI codes were clinic level hospitals. Nevertheless, our results are still meaningful in that we reported overall TSCI occurrence in the real world. Third, since AUI data have been collected by the HIRA since 2014, it could only be followed up for five years. IACI data were followed up in the same year for comparison with AUI. Therefore, additional data from the AUI and IACI databases with a longer follow-up period are needed for further research.
This study reported the incidence of TSCI across three national or quasi-national insurance databases in South Korea. In the NHIS, AUI, and IACI, the incidence of TSCI was higher among the older population those in their 60s and 70s or older, across all three insurance systems. The changing trends showed that the incidence of TSCI in older patients over 70 years of age increased significantly in the NHIS and IACI, but no significant trend was seen among the older population in AUI. These results may be due to the different etiologies and characteristics of subjects in each insurance system, implying the need for tailored medical strategies for each injury type represented by the three national insurance systems in South Korea.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download