1. Kim I, Kim HA, Seo YI, Song YW, Jeong JY, Kim DH. The prevalence of knee osteoarthritis in elderly community residents in Korea. J Korean Med Sci. 2010; 25(2):293–298. PMID:
20119586.

2. Kim IJ, Kim HA, Seo YI, Jung YO, Song YW, Jeong JY, et al. Prevalence of knee pain and its influence on quality of life and physical function in the Korean elderly population: a community based cross-sectional study. J Korean Med Sci. 2011; 26(9):1140–1146. PMID:
21935267.

3. Nguyen JC, De Smet AA, Graf BK, Rosas HG. MR imaging-based diagnosis and classification of meniscal tears. Radiographics. 2014; 34(4):981–999. PMID:
25019436.

4. Englund M, Guermazi A, Gale D, Hunter DJ, Aliabadi P, Clancy M, et al. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med. 2008; 359(11):1108–1115. PMID:
18784100.

5. Kim HA, Kim I, Song YW, Kim DH, Niu J, Guermazi A, et al. The association between meniscal and cruciate ligament damage and knee pain in community residents. Osteoarthritis Cartilage. 2011; 19(12):1422–1428. PMID:
21959098.

6. Katz JN, Brownlee SA, Jones MH. The role of arthroscopy in the management of knee osteoarthritis. Best Pract Res Clin Rheumatol. 2014; 28(1):143–156. PMID:
24792949.

7. Persson F, Turkiewicz A, Bergkvist D, Neuman P, Englund M. The risk of symptomatic knee osteoarthritis after arthroscopic meniscus repair vs partial meniscectomy vs the general population. Osteoarthritis Cartilage. 2018; 26(2):195–201. PMID:
29146386.

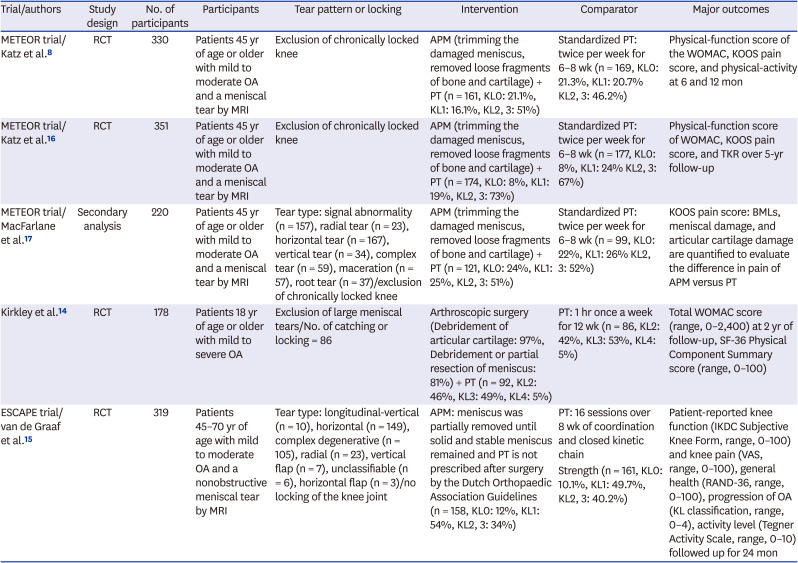
8. Katz JN, Brophy RH, Chaisson CE, de Chaves L, Cole BJ, Dahm DL, et al. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engl J Med. 2013; 368(18):1675–1684. PMID:
23506518.

9. Sihvonen R, Paavola M, Malmivaara A, Itälä A, Joukainen A, Nurmi H, et al. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013; 369(26):2515–2524. PMID:
24369076.

10. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions. 2nd ed. Chichester, UK: John Wiley & Sons;2019.
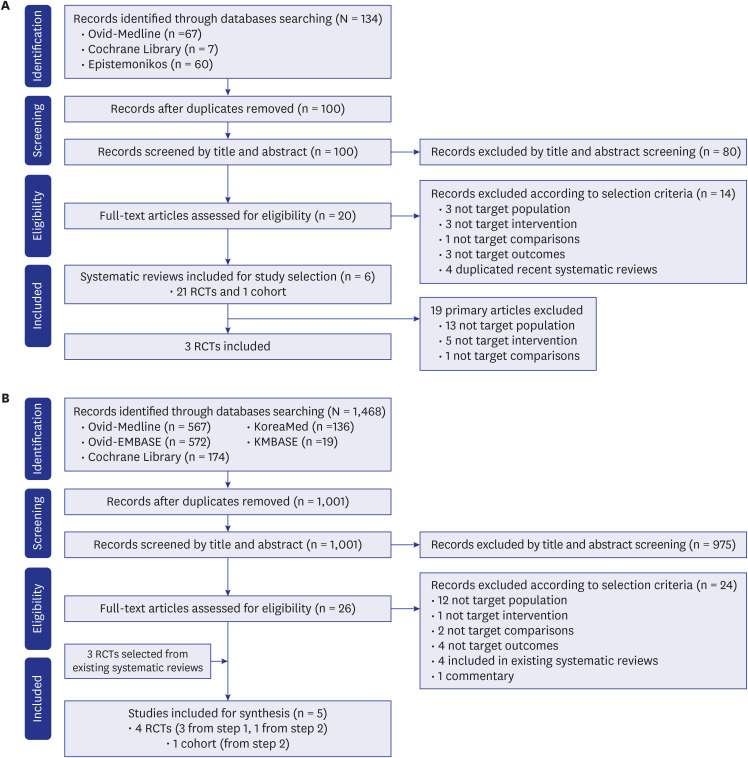
11. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009; 339:b2535. PMID:
19622551.

12. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011; 343:d5928. PMID:
22008217.

13. Kim SY, Park JE, Lee YJ, Seo HJ, Sheen SS, Hahn S, et al. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol. 2013; 66(4):408–414. PMID:
23337781.

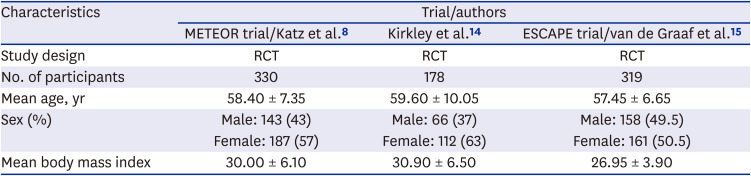
14. Kirkley A, Birmingham TB, Litchfield RB, Giffin JR, Willits KR, Wong CJ, et al. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2008; 359(11):1097–1107. PMID:
18784099.

15. van de Graaf VA, Noorduyn JC, Willigenburg NW, Butter IK, de Gast A, Mol BW, et al. Effect of early surgery vs physical therapy on knee function among patients with nonobstructive meniscal tears: the ESCAPE randomized clinical trial. JAMA. 2018; 320(13):1328–1337. PMID:
30285177.
16. Katz JN, Shrestha S, Losina E, Jones MH, Marx RG, Mandl LA, et al. Five-year outcome of operative and nonoperative management of meniscal tear in persons older than forty-five years. Arthritis Rheumatol. 2020; 72(2):273–281. PMID:
31429198.

17. MacFarlane LA, Yang H, Collins JE, Guermazi A, Jones MH, Spindler KP, et al. Influence of baseline magnetic resonance imaging features on outcome of arthroscopic meniscectomy and physical therapy treatment of meniscal tears in osteoarthritis. Am J Sports Med. 2019; 47(3):612–619. PMID:
30653921.
18. Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (Updated March 2011). London, UK: Cochrane Collaboration;2011.
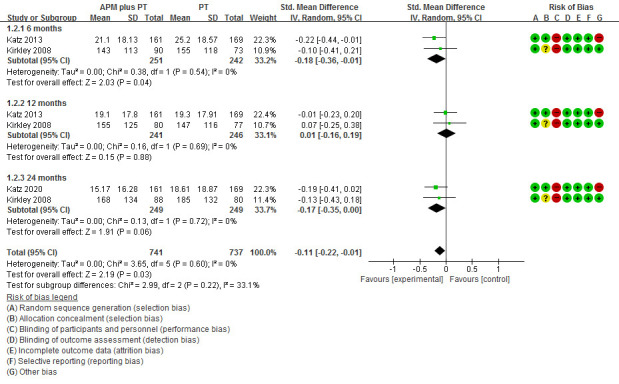
19. Olsen MF, Bjerre E, Hansen MD, Hilden J, Landler NE, Tendal B, et al. Pain relief that matters to patients: systematic review of empirical studies assessing the minimum clinically important difference in acute pain. BMC Med. 2017; 15(1):35. PMID:
28215182.

20. Tubach F, Ravaud P, Baron G, Falissard B, Logeart I, Bellamy N, et al. Evaluation of clinically relevant changes in patient reported outcomes in knee and hip osteoarthritis: the minimal clinically important improvement. Ann Rheum Dis. 2005; 64(1):29–33. PMID:
15208174.

21. Abram SG, Judge A, Beard DJ, Price AJ. Adverse outcomes after arthroscopic partial meniscectomy: a study of 700 000 procedures in the national Hospital Episode Statistics database for England. Lancet. 2018; 392(10160):2194–2202. PMID:
30262336.
22. Farina EM, Lowenstein NA, Chang Y, Arant KR, Katz JN, Matzkin EG. Meniscal and mechanical symptoms are associated with cartilage damage, not meniscal pathology. J Bone Joint Surg Am. 2021; 103(5):381–388. PMID:
33448713.

23. Petty CA, Lubowitz JH. Does arthroscopic partial meniscectomy result in knee osteoarthritis? A systematic review with a minimum of 8 years' follow-up. Arthroscopy. 2011; 27(3):419–424. PMID:
21126847.

24. Lee SM, Awal W, Vertullo C. Changing practice: incidence of non-reconstructive arthroscopic knee surgery in people over 50 years of age, Australia, 2008-2018. Med J Aust. 2020; 212(1):29–30. PMID:
31816091.

25. Blom AW, Donovan RL, Beswick AD, Whitehouse MR, Kunutsor SK. Common elective orthopaedic procedures and their clinical effectiveness: umbrella review of level 1 evidence. BMJ. 2021; 374:n1511. PMID:
34233885.





 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download