INTRODUCTION
Knee osteoarthritis (OA) is the most common form of arthritis affecting the elderly, and its implications in terms of health expenditure and quality of life are growing rapidly. OA is accompanied by diverse pathological changes in the whole joint including peri-articular muscle and menisci. Especially, meniscal degeneration is very common and is found on MRI scans of more than 60% of middle-aged and elderly individuals with radiographic evidence of OA.
1 However, whether meniscal degeneration causes knee symptoms is debatable. Studies have shown that the majority of meniscal damage is found in individuals without knee symptoms, and meniscal damage is not significantly associated with the presence of knee pain or its severity among individuals with radiographic knee OA.
123 These findings suggest that meniscal damage in elderly or OA patients should be dealt with differently from traumatic meniscal tears, where the arthroscopic repair has been reported to improve functional outcomes significantly. In line with these findings, rigorous outcome studies employing a randomized controlled trial design for arthroscopic management of degenerative meniscal tear showed that surgery was no better than physical therapy (PT) or even sham surgery in improving pain or functional status.
4567 Despite these findings, arthroscopic knee surgery remains the most common type of knee surgery, the number of arthroscopic meniscectomies increased by 12.67% in 8 years in Korea.
8 The incidence of the meniscus surgeries per 100,000 population-year in Korea was almost 10 fold higher compared to the United States.
9
In addition to the lack of clinical efficacy, some recent studies raise additional concerns that arthroscopic meniscectomy (AM) itself may be detrimental to the maintenance of the joint structure. A 14-year follow-up study of 205 patients who had undergone isolated unilateral meniscectomy showed that patients who underwent subtotal meniscectomy scored significantly worse on the knee-specific outcome than individuals who had had a partial meniscectomy for the same type of tear.
10 In a 5-year follow-up study from the Meniscal Tear in Osteoarthritis Research (MeTeOR) trial comparing PT vs. AM, 7.1% of individuals randomized to AM underwent total knee replacement (TKR) over five years with a hazard ratio (HR) for TKR of 2.0 (95% confidence intervals [CIs], 0.8–4.9) compared to those randomized to PT in the intention-to-treat (ITT) analysis.
11 The as-treated HR for TKR was even higher at 4.9 (95% CI, 1.1–20.9) for individuals treated with AM. Higher TKR rates in those undergoing AM remain a cause for concern and merit further investigation in a long-term study.
The objective of this study was to examine the rate of TKR among patients with OA who underwent AM for meniscal tears and compare this rate with those who did not by using the National Health Information Database (NHID) of South Korea.
METHODS
Dataset
Korean healthcare system covers the country’s entire population as a single national insurer in two tiers: the National Health Insurance (NHI) program, a wage-based, contributory insurance program covering around 96% of the population, and the Medical Aid program, a government-subsidized public assistance program for medically indigent individuals with a low income. In this study, we used data from NHID, which is a public database containing details such as health care utilization, health screening, sociodemographic variables, and mortality for the entire population of South Korea covered by NHI and Medical Aid since 2002.
12 It contains information on inpatient and outpatient medical care (diagnosis, length of hospital stay, and treatment received) and prescription records (drug code, duration of prescription, and daily dosage).
Study population
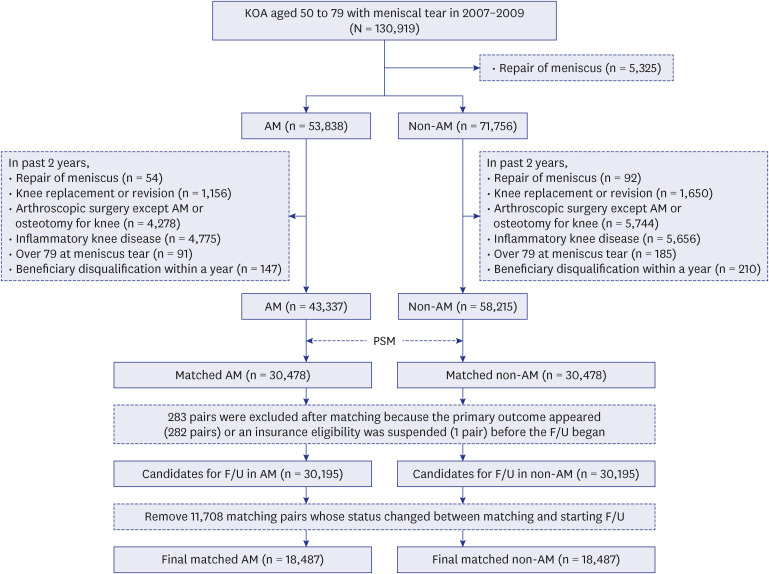
We retrospectively identified a cohort of knee OA patients with meniscal tears aged ≥ 50 years who received medical treatment using NHID for 2006 and 2019. Patients who underwent knee surgery, including joint replacement, AM, osteotomy, or other arthroscopic surgery, less than 2 years prior to study inclusion, who were diagnosed with inflammatory arthritis, and who died less than 1 year after study inclusion were excluded. Operational definitions were first examined to improve the precision of identifying patients with OA in the claims database. Patients with knee OA were identified using a combination of diagnostic, medication prescription, and procedure codes (
Supplementary Table 1). We constructed seven operational definitions by combining three conditions that were employed in a previous report using Korean claims data with a few modifications as follows
13: 1) M15, M17, or M19 and knee X-ray; 2) M17 and a prescription medication approved for only OA (
Supplementary Table 1); and 3) M17 and knee surgery (
Supplementary Table 2). The sensitivity, specificity, accuracy, positive predictive value (PPV), and negative predictive value (NPV) of each definition were determined by reviewing the medical records and knee radiographs of patients from two academy-affiliated tertiary hospitals. Kellgren and Lawrence (KL) ≥ 2 was considered definite radiographic knee OA. Patients with knee OA were defined as those with one or more claims with M15, M17, M19, and knee X-rays, or those with one or more claims with M17 and drug prescriptions approved only for OA. This definition has accuracy, sensitivity, specificity, PPV, and NPV of 75%, 81%, 48%, 87%, and 36%, respectively.
Meniscal damage in OA patients was defined as one or more claims with a meniscectomy or a repair of meniscus, or one or more claims with M23.2, M23.3, or S83.2 (derangement of meniscus due to old tear or injury; other meniscus derangements; tear of the meniscus, current injury, respectively) after study inclusion. Procedure codes for defining AM and TKR are shown in
Supplementary Table 1.
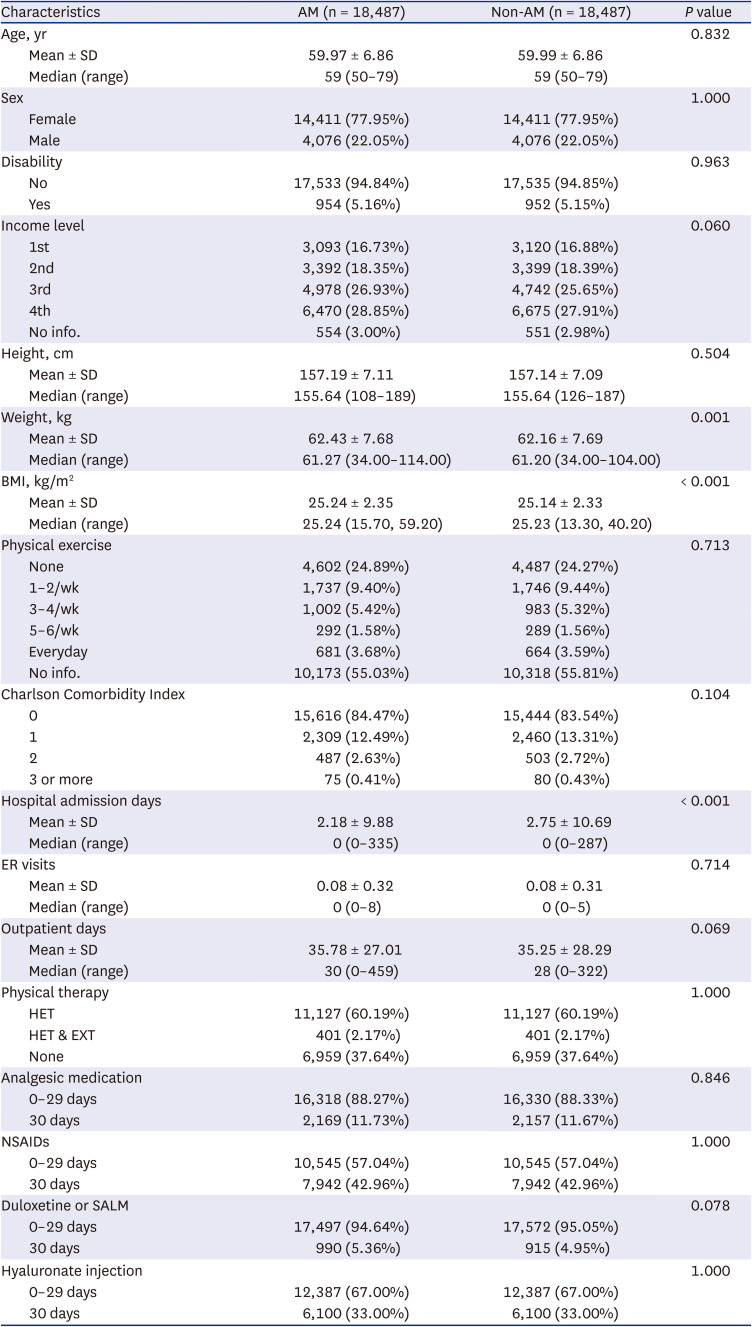
Propensity score matching (PSM)
Among patients with OA and meniscal damage, those who were treated with AM from January 1, 2007, to December 31, 2009, were selected as the AM group, while those not treated with AM were selected as the control group. PSM was performed to minimize the probability of confounding by indication by pairing the AM and non-AM groups based on propensity scores. Clinical and sociodemographic variables included in the PSM model are shown in
Supplementary Table 3. Comorbidities were assessed using read codes for medical conditions and by self-reported details of disease history obtained from questionnaires in the national health screening database. We used greedy nearest-neighbor matching without the replacement method to achieve adequate 1:1 matches. Mean ± standard deviation, number (%), and standardized differences were used to examine the covariate balance between groups. If the standardized difference was less than 0.10, the variable was included in the model as a covariate.
Exposure and outcome
The index date was defined as the date of AM in the exposed participants. Unexposed participants were assigned the index date of their matched exposed participants. The outcome was the time to TKR from the index date. TKR occurrence was defined as the appearance of the TKR procedure code between the index date and the last observation date. Because the administrative data did not specify the side of the knee on which the operation was performed, we conservatively defined the outcome as the second TKR. When AM was performed on both knees simultaneously, the time to the first TKR was defined as the outcome. Exposed and unexposed participants were followed up starting from the index date until the occurrence of TKR, death, or study end date (December 31, 2019), whichever is earlier. The follow-up period of the participants who did not experience an outcome was censored.
Statistical analysis
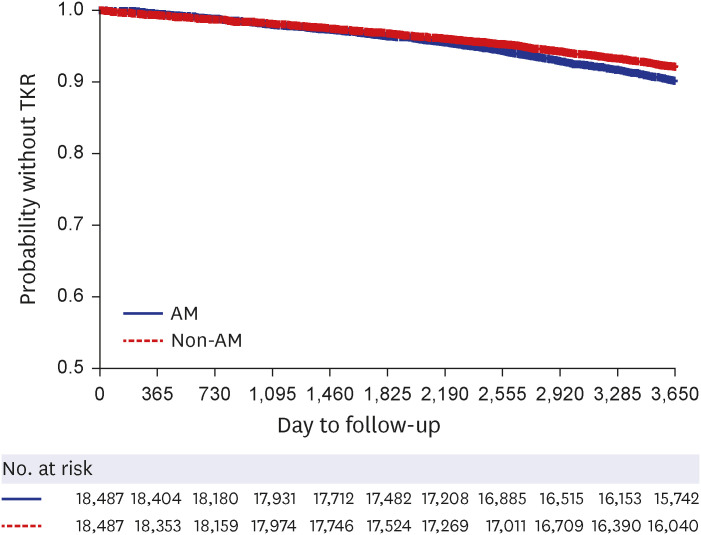
Missing values for continuous variables were imputed as the mean of the complete cases in the study sample of the same age and sex. For categorical variables, missing data were grouped into additional categories. The Kaplan–Meier method was used to analyze the time to TKR, and the log-rank test was used to test differences between the AM and non-AM groups. A model that regarded TKR as the major event and death as the competing risk was fitted to evaluate the differences between the two groups after adjusting for potential confounding factors using the Cox model. Covariates that were likely to influence outcomes (age, sex, income level, disability, comorbidities, medication, PT used, body mass index) or which reflect general health-seeking behavior and may influence consultation for musculoskeletal pain (place of residence, number of hospital admissions, or emergency room visits in the 12-month period preceding study inclusion) were included in the model. The subdistribution hazard ratios (sHRs) with 95% CI were calculated.
Sensitivity analysis
The robustness of the results was additionally assessed using an as- treated analysis, the first TKR as an outcome, or using different operational definitions for OA. All statistical analyses were conducted using SAS version 9.4 (SAS Institute, Inc., Cary, NC, USA). Statistical significance was set at P < 0.050.
Ethics statement
This study used de-identified data and was conducted without patient and public involvement. The Institutional Review Board of NECA approved the use of NHID data as well as the study protocol (NECA IRB20-019, NHIS-2021-1-054).
DISCUSSION
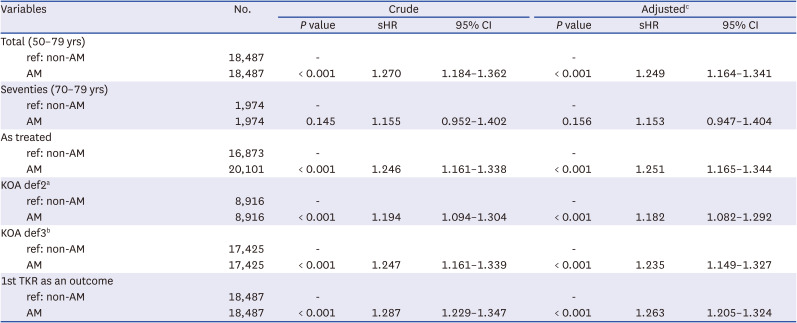
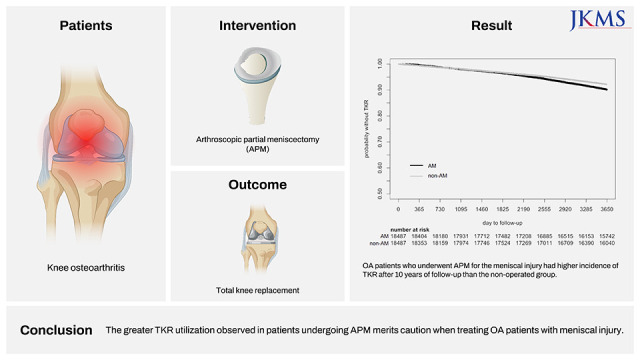
In this study, using the administrative database of the NHIS in South Korea, the rate of TKR among patients with OA who underwent AM due to meniscal tear was compared with those who did not, with the help of PSM. The results showed that the AM group had a 25% increase in TKR after 10 years.
Recent randomized controlled trials comparing arthroscopic surgery with sham surgery or PT in patients with degenerative meniscal tears showed that surgery was no better than PT or even sham surgery in improving outcomes, raising concerns about the value of surgical treatment.
67 Meniscal damage of the knee is commonly observed among elderly individuals without knee symptoms, corroborating the lack of effectiveness of AM in degenerative meniscal tears.
13 A recent study revealed no significant association between the presence and pattern of meniscal tears observed on arthroscopy and symptom scores, including grinding/clicking/popping, pain when pivoting, or catching/locking, defying the common belief that “mechanical” symptoms arise from meniscal tears.
14 Furthermore, the influence of meniscus resection or arthroscopy itself on cartilage damage is an unsettled topic, with some indicative evidence. A study reporting a statistically significant increase of radiographic signs of OA at 8–16 years of follow-up after knee AM compared with control non-operated knees reported a protective effect of the meniscus on cartilage, raising further concern that AM may have negative consequences in the maintenance of joint integrity.
15 A case-control study that enrolled patients from the OA Initiative reported that in the group with incident radiographic osteoarthritis (ROA), 4.4% underwent partial meniscectomy during the year prior to the case-defining visit compared with none of the knees that did not develop ROA.
16 Particularly, when looking only at knees that developed ROA, partial meniscectomy was associated with a greater risk of worsening cartilage damage, as assessed using MRI, with an odds ratio (OR) of 4.51. In a systematic review of published reports, the annual incidence of TKR after arthroscopic surgery for OA was found to be 2.62%, with a median duration of 2.0 years between arthroscopy and TKR.
17 Patients who were older or had more advanced ROA at the time of arthroscopy had higher risk of TKR. However, it is not clear whether the increase in OA or TKR results from meniscal damage leading to arthroscopic surgery or arthroscopic surgery per se. This issue was examined by posthoc analysis of the MeTeOR trial, which compared AM and PT. Despite the problem of crossover during follow-up with as many as 30.2% of patients in the PT group receiving AM treatment, the result showing that the AM group had a greater, albeit not significant, frequency of TKR over 5 years, indicates the need for exercising additional caution when using arthroscopic surgery in OA. Compared to the MeTeOR subjects, our study population in the AM group had a lower HR for TKR despite a longer follow-up time. Both study subjects had similar mean ages; thus, this discrepancy in the TKR rate may stem from ethnic disparity in the study population or from differences in healthcare utilization. An Italian study reported a 15.7% conversion rate from AM to TKR at 20 years with a mean time between surgeries of 7 years; this finding was consistent with our results.
18 Subsequent TKR after AM for degenerative meniscal tears was significantly associated with the severity of preoperative OA and chondral lesions (Kellgren Lawrence 2; Outerbridge > 2), lateral meniscectomy, age at surgery, female sex, and malalignment.
18 A Swedish study involving patients aged 16–45 years who underwent surgery due to traumatic meniscal tears reported that the absolute risk of requiring consultation for knee OA after a median follow-up of 10.3 years was about 25–50% lower after meniscus repair than AM. This suggests that preservation of the meniscus may be a better option than AM for maintaining joint structure.
19 However, the consultation rate for knee OA standardized to the general population was twice as high after meniscus repair as that of the general population, suggesting that meniscal damage itself is also responsible for the development of OA.
This study has several limitations. Although this study applied various algorithms to identify OA cases from the administrative database, it was impossible to confirm the diagnosis individually. The choice of the operational definition for the study subject as ‘those with one or more claims with OA diagnostic codes and knee X-rays, or approved drug prescriptions only for OA’ was arbitrary, although it had high accuracy, sensitivity, and PPV. Sensitivity analysis using different operational definitions as cases led to the same result; however, misclassification of healthy individuals as having OA would have biased the study results toward the null. Second, rigorous PSM would not resolve the issue of confounding by indication, which might have acted in either way. If patients with more severe OA and symptoms had a higher tendency to undergo AM, this would have resulted in a higher TKR rate in the AM group. Although the rate of PT or analgesic medication prescriptions before AM did not differ between the two groups, this possibility cannot be completely ruled out without considering information on radiographic findings or symptom severity. In contrast, the AM group might have had better physical function than the non-AM group and thus would have been more willing to undergo surgery, such as AM or TKR. This remains a lingering concern despite the similar Charlson Comorbidity Index and disability rate. Third, because the administrative database does not contain which side of the knee was operated on, it was unknown whether TKR was performed on the same side as the AM knee. We defined second TKR as the outcome to address this limitation, which probably led to a conservative outcome. Sensitivity analysis using the first TKR did not result in a notably higher OR, however, and this finding supports our conservative approach. Inability to distinguish the extent of meniscectomy (partial or total) is also a limitation because it may affect the speed of joint degeneration. Lastly, because of the lack of information on the severity of OA or the extent of meniscal injury, direct harm of arthroscopic partial meniscectomy in OA joint damage cannot be ascertained.
A key strength of this study was the use of a large database representing the entire Korean population and reflecting real-world situations. The extensive adjustment for confounders minimized confounding by indication in our study, which is otherwise a major issue in these types of studies. Lastly, the sensitivity analyses agreed with the primary findings of increased risk with AM with largely similar HRs, suggesting that these results are robust given the assumptions in our analytical approach.
In conclusion, our study showed that OA patients who underwent AM for the meniscal injury had a 9.62% cumulative incidence of TKR after up to 10 years of follow-up, which was 25% higher than the non-operated group.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download