This article has been
cited by other articles in ScienceCentral.
Abstract
Background
The pediatric field in South Korea is experiencing a significant workforce crisis due to a sharp decline in pediatricians, exacerbated by a decrease in pediatric residents and a series of distressing incidents in pediatric healthcare institutions. No prior studies have explored the waning interest in pediatrics among South Korea’s medical students and interns, which our research seeks to address during a pediatric workforce decline. This study aimed to investigate the declining interest in pediatrics among medical students and interns in South Korea amidst decreasing birth rates. We conducted a comprehensive survey to identify the factors deterring young medical professionals from pursuing a career in pediatrics.
Methods
In this cross-sectional study, in December 2023 we surveyed medical students and interns at Jeonbuk National University and Hospital using a 40-item electronically distributed questionnaire tailored to assess the factors influencing specialty choice, focusing on pediatrics. The participants were divided into the pre-clinical and clinical groups, allowing for analysis across educational stages. The survey covered demographics, perceptions of pediatrics, attitudes toward medical errors, and awareness of critical issues; it included a range of question types to ensure detailed and nuanced data collection.
Results
Our findings revealed a clear decrease in interest in pediatrics as medical students progressed through their education, with 86.69% displaying negative views. Although a sense of mission and emotional satisfaction from patient interactions were highlighted as positive influences, they were significantly countered by worries related to declining pediatric populations, legal challenges, and interactions with patient guardians. Additionally, 95.84% of the participants recognized the critical role of vital pediatric departments; however, litigation risks and psychological burdens substantially affected their willingness to specialize in these areas. The analysis also showed an increasing awareness of pediatric incidents as students advanced through their education; however, this did not directly correlate with their choice of specialty (P = 0.090).
Conclusion
The results emphasize the necessity for targeted interventions to alleviate concerns and improve the attractiveness of pediatrics. These efforts are essential to counteract the declining interest and ensure a sustainable pediatric workforce for the future.
Keywords: Pediatrics, Specialty Choice, Medical Students, Interns
INTRODUCTION
The pediatric field in South Korea is facing a severe problem as the number of pediatricians is sharply declining, leading to a significant workforce crisis.
1 In addition to the ongoing drop in birth rates, the situation has become unexpectedly disastrous as the number of pediatric residents plummets.
1 In 2023, only approximately 16% of residency positions were filled, highlighting the severity of the shortage, which is now becoming a major national issue.
A critical point in this downward trend was the distressing incident at Ewha Womans University Mokdong Hospital, where four newborns died in 2017 due to bacterial infection. This incident was a possible key factor in the rapid decline in the number of pediatricians.
12 The possibility that these deaths were linked to sepsis due to contamination with intravenous fluids was raised. Consequently, several members of the medical team, including a professor in the pediatric department specializing in neonatology, were arrested and faced criminal charges related to medical negligence. Although the medical team was eventually found not guilty, the repercussions of this incident were substantial.
3 In 2023, the situation reached a critical point where only 53 out of 208 national residency positions were filled, resulting in a residency application rate of 25.4%. This marks a marked decline from previous years in which application rates were 80% in 2019, 74% in 2020, 38% in 2021, and 27.5% in 2022.
4
The situation worsened with the death of a pediatric patient with croup in 2023, drawing significant public attention,
5 although this was not directly linked to a pediatrician shortage. Prior to this tragic event, the child exhibited symptoms of high fever, prompting the family to seek medical intervention from a pediatric specialist. After contacting five different emergency rooms, the patient was able to receive treatment only at the one that allowed admission under their specific conditions. Following discharge on the day after visiting the emergency room, the child experienced an abrupt and severe onset of respiratory distress. Notably, no direct causal nexus could be established between the actions taken by the medical facility and the patient's unfortunate outcomes. Nevertheless, this case reflects the broader implications of pediatrician shortages, as the child's access to appropriate emergency care was restricted to just one of the five hospitals contacted due to specific admission conditions linked to staffing levels, underscoring the urgent need for comprehensive studies and policy reform in pediatric healthcare staffing.
67
The Declaration of Closure for a Primary Care Pediatric Society was another disturbing incident in Korea.
8 The Korean Pediatric Association issued a statement expressing its lament over the challenges faced by primary care practitioners who have chosen to forsake a lifelong commitment to pediatric and adolescent specialized care in favor of pursuing a path in general medicine. This gesture was intended to highlight the challenges encountered by pediatric practitioners, as conveyed by the Korean Society of Pediatrics.
Amidst these troubling times, the importance of conducting a comprehensive survey of interns and medical students before their specialty selection became even more pronounced. Despite this critical situation, to the best of our knowledge, there has been no prior research on the declining interest in pediatrics among medical students and interns in South Korea. This survey aimed to probe the reasons behind the waning interest in pediatrics and understand what discourages young medical professionals from pursuing this field. The insights gleaned from this survey are crucial for crafting targeted strategies and interventions, confronting the immediate crisis, and ensuring the long-term sustainability and fortitude of pediatric healthcare in South Korea.
METHODS
Study design
In December 2023, a cross-sectional study was conducted among medical students and interns at Jeonbuk National University and Jeonbuk National University Hospital to explore the factors influencing their choice of a medical specialty, focusing on pediatrics. An electronic self-administered questionnaire was developed and distributed to both groups via Google Forms. In this study, “1st premed” denotes the first year of pre-medical undergraduate studies, whereas “1st med” refers to the first year of the medical school curriculum. Data collected from this survey were analyzed to compare the influences on specialty choice between students at different stages of their medical education.
Questionnaire
In designing our study, we developed a 40-item questionnaire that was meticulously tailored to meet our research objectives. We collected data on demographic characteristics, including sex, academic year, and marital status. The survey consisted of seven sections. The first section sought consent for study enrollment. The second section gathered demographic data. The third section surveyed perceptions of pediatrics. The fourth section focused on perceptions and attitudes toward medical errors. The fifth section explored awareness of vital aspects of pediatrics. The sixth section addressed issues related to low birth rates. Finally, the seventh section allowed for open-ended responses. The questionnaire format was diverse, including questions that required a simple “yes” or “no” response and others where participants could select two to three reasons they deemed most significant. To avoid potential bias toward neutral responses, we incorporated a rating scale ranging from 1 (strongly disagree) to 6 (strongly agree), enabling a nuanced assessment of each item. This comprehensive approach ensured that detailed and relevant data were gathered to meet the study objectives.
Statistical analysis
For data analysis, we used ChatGPT to create and interpret graphs, which facilitated a comprehensive examination of our data. This method enabled effective analysis of trends within our dataset, offering insights into the medical students' specialty preferences. ChatGPT’s data processing and graphical capabilities were instrumental in our analysis. We performed correlation analysis and linear regression to explore the relationship between medical educational stages and attitudes toward pediatrics. Pearson’s correlation coefficient assessed the relationship's strength and direction. Linear regression, with the educational stage as the independent variable and attitude toward pediatrics as the dependent variable, quantified attitude changes across stages. The regression model’s slope and R-squared value interpreted the relationship and variance in attitudes explained by the educational stage. Spearman's rank correlation assessed the association between educational stages and pediatric specialty interest, which is suitable for our ordinal data. This test’s significant correlation coefficient highlighted a consistent pediatric preference trend. An unpaired t-test evaluated sex-based differences in the desired number of children, comparing mean values between sexes.
A heatmap visualized average responses to participant-rated statements. Data were aggregated by calculating mean responses for each item. These means were plotted in a matrix, with cell color intensity reflecting response magnitude, offering a quick data distribution view. The dataset was segmented by stage for analysis, with means calculated within each subgroup to show stage-specific trends. The heatmap used a sequential color scheme for response ranges, with cell annotations providing exact values for clearer study context interpretation.
Ethics statement
The research protocol was reviewed and approved by Jeonbuk National University Hospital’s Institutional Review Board (2023-11-025-002). To ensure ethical rigor, we structured the study to uphold participants’ autonomy and confidentiality. Comprehensive information about the study’s intent was shared upfront, empowering the participants to disengage at any stage. To further solidify ethical compliance, participants’ entry into the study was marked by providing digitally documented consent.
RESULTS
Demographic characteristics and response rate
Out of a total of 865 participants, consisting of 51 interns from Jeonbuk National University Hospital and 814 medical students, 729 (84.28%) responded. Of these, seven individuals opted out of having their answers used in the study. Additionally, one participant whose age was recorded as 99 years was excluded from the analysis because of data inaccuracy. Sex distribution among the study participants was 37.45% females and 62.55% males. The breakdown of the survey respondents is as follows: 118 were in their first year of premedical school, 132 in their second year, 122 in their first year of medical school, 131 in their second, 114 in their third, 77 in their fourth, and 27 were interns.
Perception of pediatrics
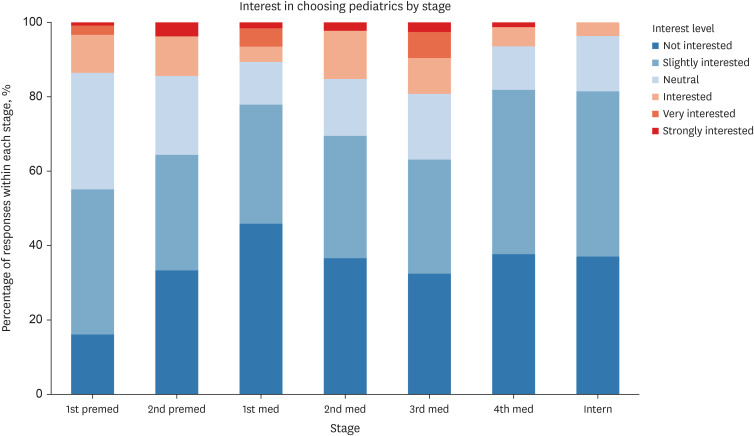
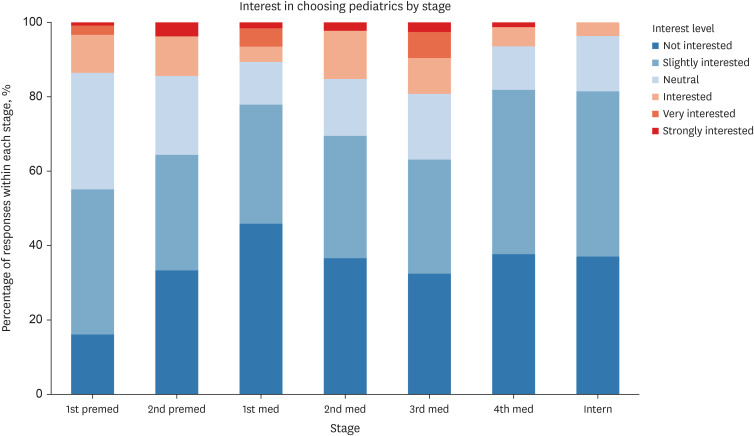
Fig. 1 illustrates varied levels of interest in choosing pediatrics as a future specialty across different educational stages. Of the 721 survey participants, 625 (86.69%) students responded negatively (scoring 1–3) to the question, “Do you want to choose pediatrics as your future specialty?” Linear regression and correlation analyses showed a moderate positive correlation (coefficient: 0.53) for negative responses, indicating that as students progress through their stages of education, from 1st premed to internship year, the tendency to respond negatively increases. Spearman's rank correlation was used to assess the relationship between the stage of medical education and students' desire to choose pediatrics as a future specialty (
r= −0.114,
P = 0.002). The demographic characteristics of the group interested in pediatrics comprised 43.75% males and 4.17% married individuals, with a mean age of 22.94 years. Contrastingly, the group not interested in pediatrics consisted of 34.56% males (
P < 0.001), 0.96% married individuals (
P = 0.042), and a mean age of 23.05 years (
P = 0.717).
Fig. 1
Distribution of medical students’ interest in pediatrics based on academic year and internship stage. 1 = strongly disagree; 2 = disagree; 3 = somewhat disagree; 4 = somewhat agree; 5 = agree; 6 = strongly agree.
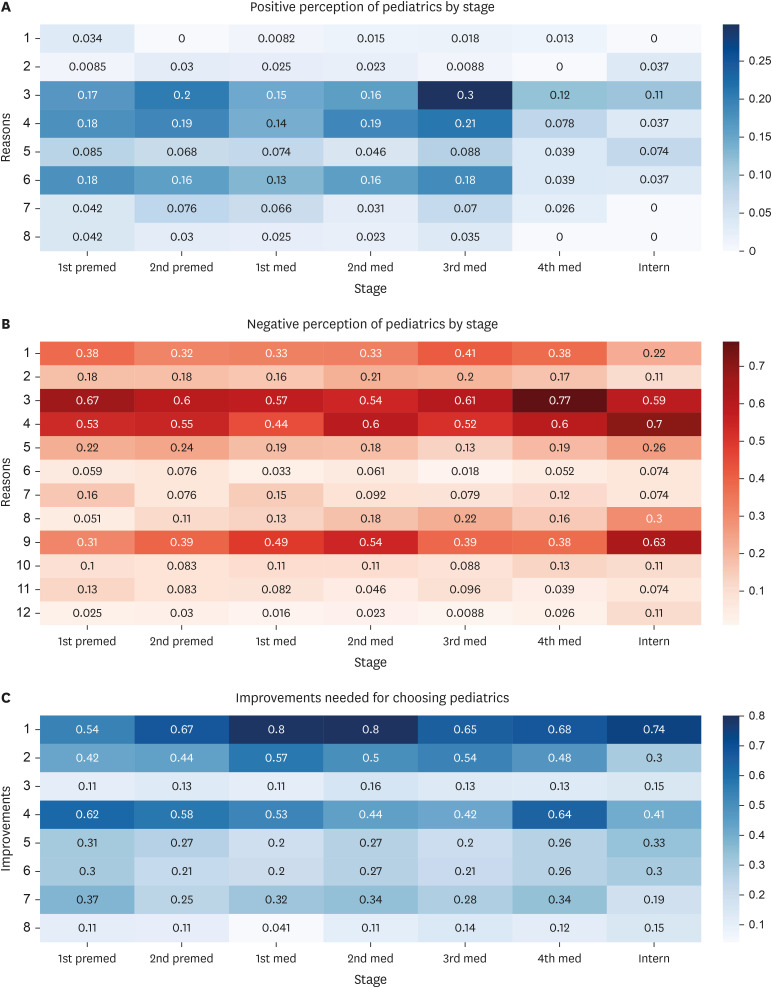
In the survey, students who had a positive view of pursuing a career in pediatrics were invited to select up to three reasons that influenced their perspectives. Heatmap analysis (
Fig. 2A) revealed that the most cited factor influencing medical students’ positive perception of pediatrics was an altruistic mission to enhance pediatric patients’ health and welfare. This motivation dominated all educational stages and significantly influenced their specialty choice. Emotional satisfaction from interactions with pediatric patients also emerged as a significant factor. The survey findings indicated that income level, work-life balance, and academic exploration were identified as the least influential reasons for medical students’ positive perceptions of a career in pediatrics.
Fig. 2
Medical students’ perceptions and considerations for pediatrics across educational stages: a heatmap analysis. (A) Heatmap of medical students’ positive perceptions towards pediatrics based on educational stages: 1) Income level, 2) work hours and life balance, 3) emotional satisfaction from interacting with pediatric patients, 4) sense of mission in improving the health and welfare of pediatric patients, 5) optimism for future development due to current medical staff shortage, 6) professional achievement in restoring health and life of pediatric patients, 7) positivity of pediatric patients’ recovering ability and prognosis, and 8) academic exploration of pediatrics and pediatric patients. (B) Heatmap of medical students' negative perceptions towards pediatrics based on educational stages: 1) Income level, 2) work hours and life balance, 3) decrease in the pediatric population due to a very low birth rate, 4) difficulties in interacting with guardians, 5) complexity and difficulties in interacting with pediatric patients, 6) influence of mass media, 7) employment insecurity, 8) anxiety about frequent life-threatening situations in pediatrics, 9) anxiety about lawsuits, 10) uncertainty in duty and future career as a specialist, 11) decreased academic attraction to pediatrics and pediatric patients, and 12) professional stress and anxiety from competition with general practitioners. (C) Heatmap of medical students’ perceptions and required improvements for choosing pediatrics based on educational stages: 1) Legal security measures against lawsuits, 2) economic stability from increased compensation, 3) job opportunities and career growth due to job increase, 4) increased pediatric medical demand and job security from higher birth rates, 5) hiring of professional guardian consultants, 6) enhanced respect and job satisfaction from improved social perception, 7) improvement in workload distribution due to a shortage of pediatric staff, and 8) unique procedures or treatments exclusive to pediatric specialists.
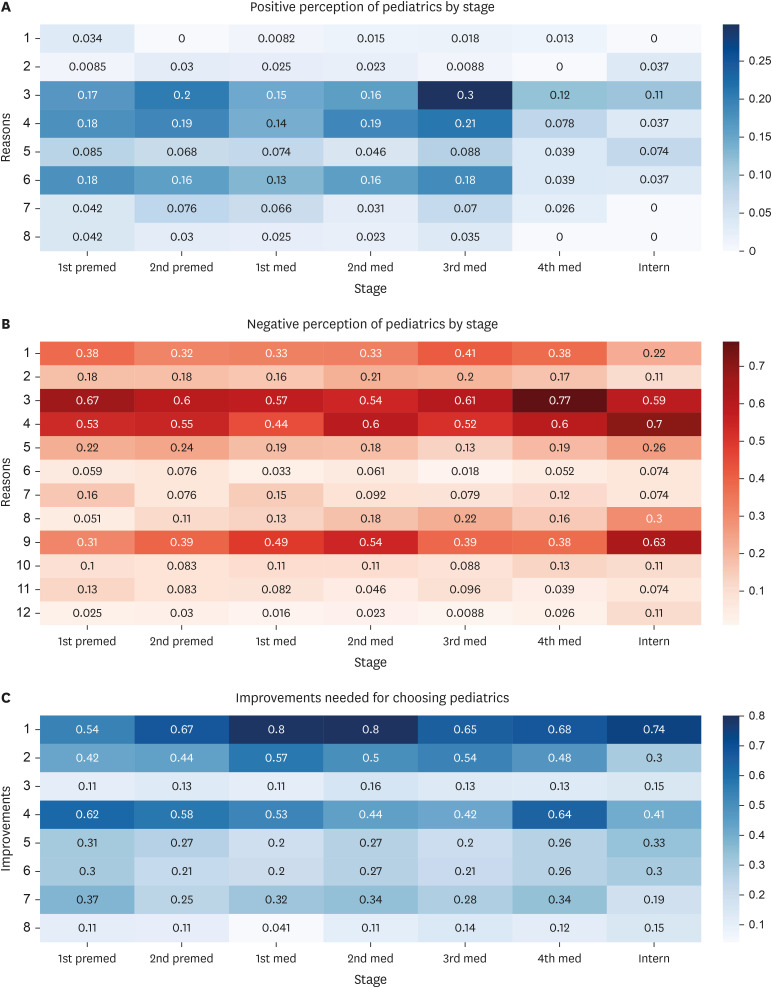
The heatmap in
Fig. 2B provides an insightful representation of the factors contributing to a negative perception of pediatrics, as conveyed by respondents who could select up to three reasons for their stance. Heatmap analysis indicated that the respondents’ negative perceptions of pediatrics were most strongly associated with concerns about the declining pediatric population, challenges interacting with patients’ guardians, and apprehensions regarding potential legal issues. Additionally, concerns regarding income levels emerged as a significant factor, with these issues becoming more pronounced as medical students advanced to the intern stage, reflecting a heightened awareness of practical and professional challenges in pediatrics. In contrast, the influence of mass media, decreased academic interest in pediatrics, and professional stress and anxiety were the least cited reasons, suggesting that these factors had a relatively minor impact on students' perceptions of the field. In addressing the specific query on the role of mass media and social perception, 67.55% of students recognized their negative influence on choosing pediatrics as a specialty; however, these concerns were not reflected as major deterrents in the practical decision-making process regarding specialty selection.
In the heat map showing the perspectives of students with a negative perception of pediatrics (
Fig. 2C), interns most prominently highlight the need for legal security measures against lawsuits as a critical area for improvement when considering pediatrics. The need for economic stability from increased compensation, increased pediatric medical demand, and job security from higher birth rates were also identified as important areas for enhancement.
Of the 721 respondents, 43.55% indicated a pronounced preference for pediatric training among medical students at large tertiary hospitals in the Seoul or Gyeonggi region across all educational stages.
The current evaluation pertains to policies implemented by the government and pediatric associations to augment the pediatric workforce. First, of the 721 respondents, 42.30% agreed that a salary increase for residents has a positive impact on choosing pediatrics as a specialty, 35.37% disagreed, and 22.33% were neutral. The trend analysis of the mean responses per stage suggests that opinions vary across stages. Second, we examined the influence of transitioning from a 4-year to a 3-year pediatric residency program on pursuing pediatrics as a specialty. In total, 45.35% believed that a shorter residency would positively influence their decision to specialize in pediatrics. This sentiment was particularly strong among interns, with 81.48% in agreement. Third, the students were asked whether an increase in medical school quotas would influence their decision to choose a specialty, and 62.55% indicated that increased medical school quotas would significantly impact their career planning. Moreover, they were asked whether they believed this increase would aid in resolving the pediatric workforce shortage. Only 4.58% believed that increasing medical school quotas would help solve the pediatric workforce problem.
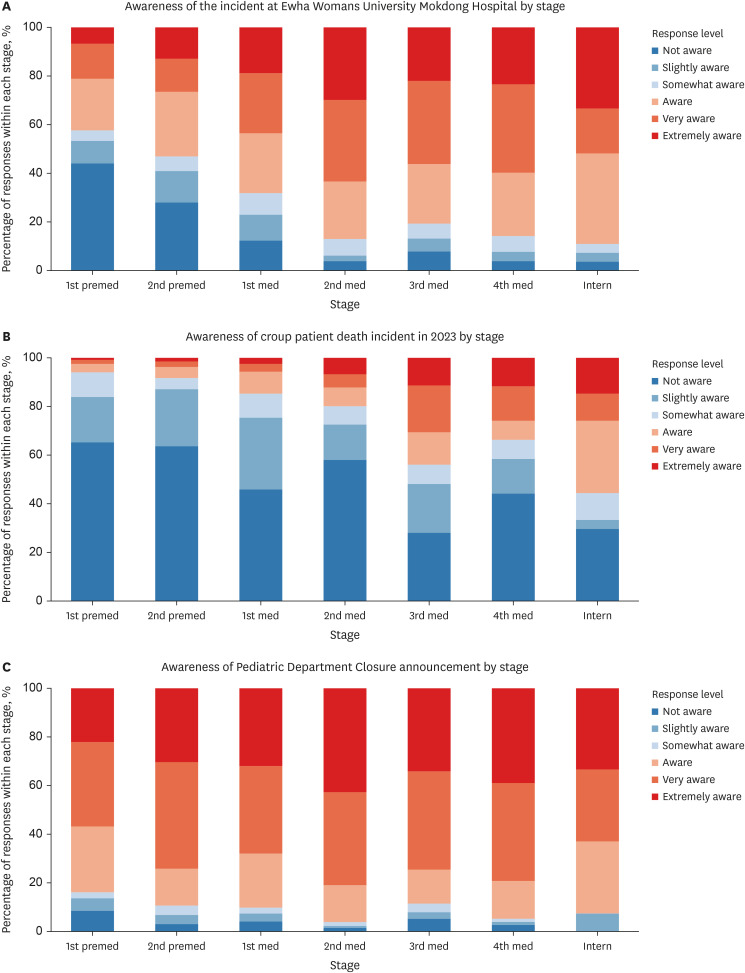
Perceptions and attitudes toward medical issues
Fig. 3A presents the students’ responses on their awareness of the Ewha Womans University Mokdong Hospital neonatal incident, revealing increased awareness with academic progression. Spearman’s rank correlation was used to analyze the relationship between medical educational stages and incident awareness, showing a significant correlation coefficient of 0.363 (
P < 0.001).
Fig. 3B summarizes the responses about awareness of the pediatric patient death due to croup in 2023, where Spearman's correlation indicated a correlation coefficient of 0.291 (
P < 0.001), showing awareness differences across educational stages.
Fig. 3C illustrates awareness distribution among students about pediatric department closures by stage, with 90.43% showing high awareness (scores 4–6) of the “Pediatric Department Closure Declaration.” Spearman’s correlation for educational stage versus closure awareness yielded a coefficient of 0.131, indicating a significant, though modest, positive correlation (
P < 0.001). This suggests high general awareness, with variations in awareness levels at different educational stages.
Fig. 3
Medical students’ awareness of significant pediatric incidents based on educational stages. (A) Awareness levels of medical students regarding the Ewha Womans University Mokdong Hospital neonatal incident. 1 = first time hearing; 2 = informed; 3 = moderately informed; 4 = well informed; 5 = very informed; 6 = very well informed. (B) Medical students’ awareness of the croup pediatric death incident. 1 = first time hearing; 2 = informed; 3 = moderately informed; 4 = well informed; 5 = very informed; 6 = very well informed. (C) Medical students’ awareness of the Declaration of Pediatrics Department Closures. 1 = first time hearing; 2 = informed; 3 = moderately informed; 4 = well informed; 5 = very informed; 6 = very well informed.
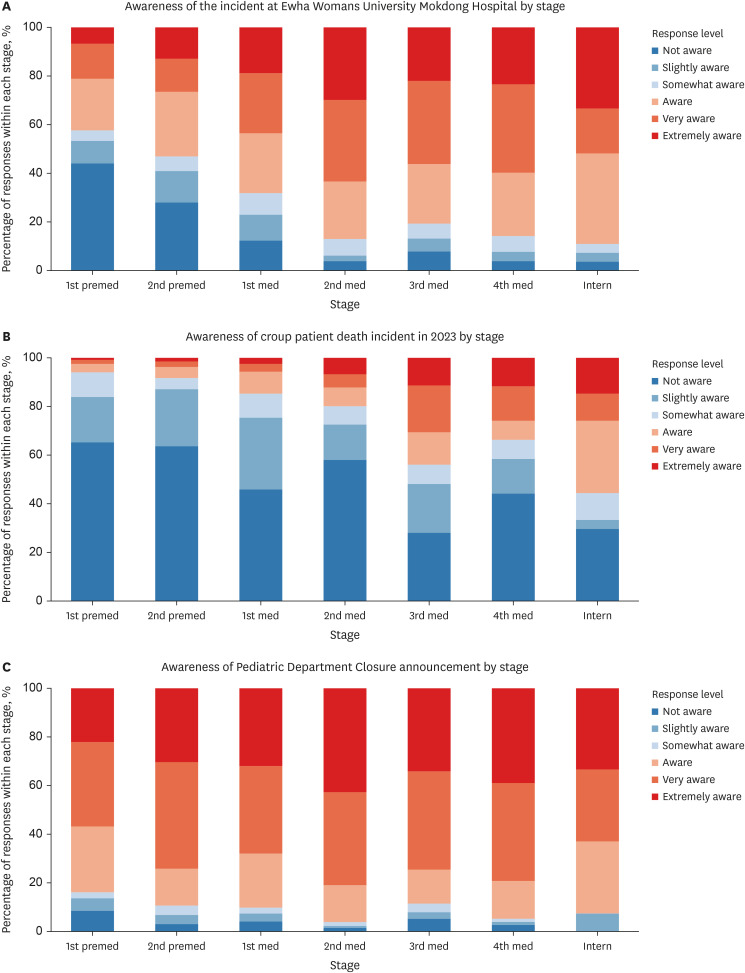
Furthermore, 80.1% of medical students across various stages of their education perceived recent pediatric incidents to influence their perspectives on the specialty significantly. Spearman's rank correlation was used to assess the correlation between the level of medical education and the impact of these incidents on students' perceptions, resulting in a P value of 0.090, which was not significant. Regarding concerns over litigation risks stemming from medical accidents, 98.89% of respondents expressed concern. Spearman’s rank correlation analysis indicated a significant, slightly upward trend in these concerns with advancing medical education (r = 0.160, P < 0.001).
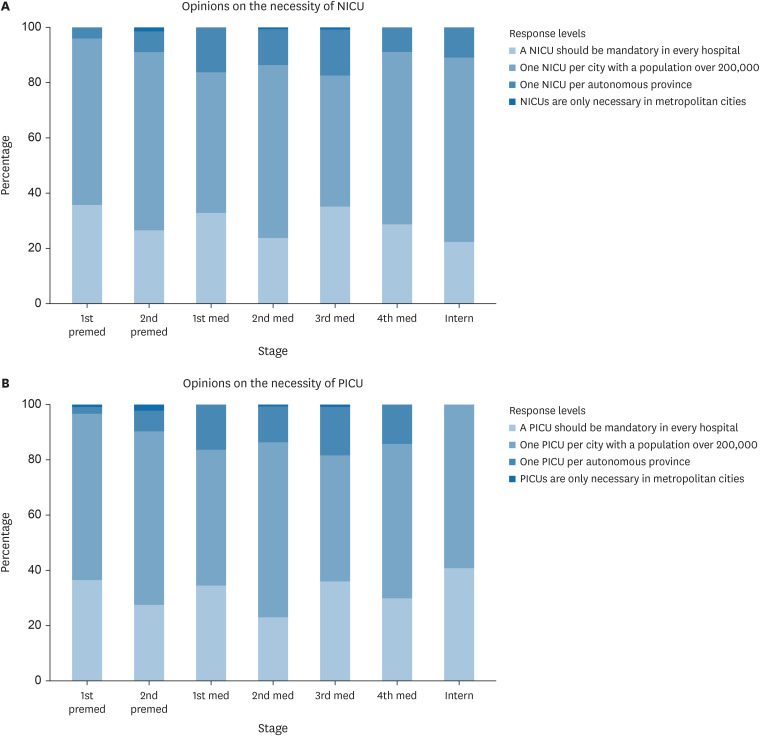
Awareness of vital aspects in pediatrics
Approximately 95.84% of students considered the vital department of pediatrics important. Spearman's rank correlation for the importance of the vital department within pediatrics in relation to the stage of medical education yielded a correlation coefficient of 0.074 (
P = 0.048).
Fig. 4 depicts the students’ perspectives on establishing neonatal intensive care units (NICUs) and pediatric intensive care units (PICUs) regarding required area coverage. This figure consolidates the students’ views on how essential it is to have these units accessible within a certain area, reflecting their understanding of these units' critical role in pediatric care. Overall, a consensus was observed among medical students that both NICUs and PICUs are critical resources, suggesting widespread recognition of their necessity in the healthcare infrastructure.
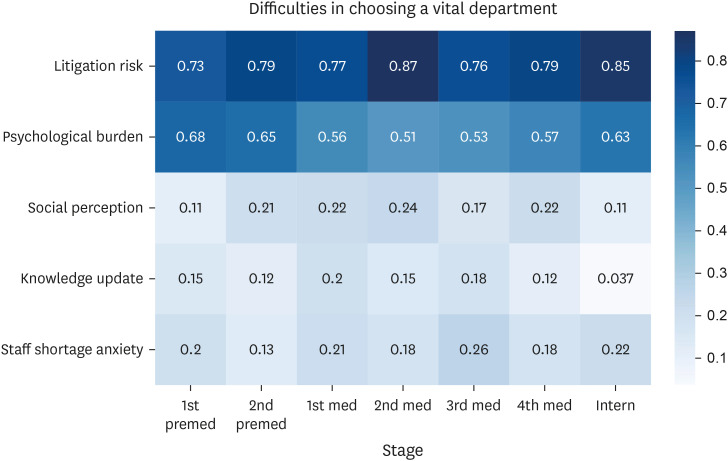
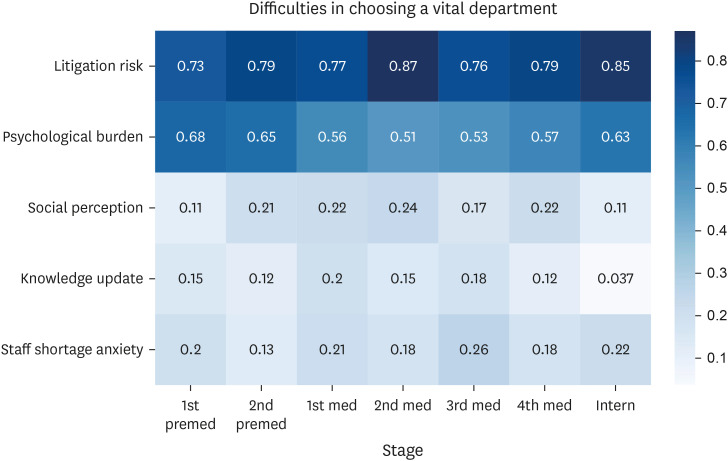
Fig. 5 illustrates a heatmap representing the perceived difficulties in choosing a vital department within pediatrics, with the option for respondents to select up to two factors, across the different stages of medical education. The heatmap shows that litigation risk and psychological burden were consistently perceived as significant difficulties across all stages.
Fig. 4
Perspectives of medical students on the distribution of intensive care units for neonates and children. (A) Opinions on the necessity of NICUs. A NICU should be mandatory in every hospital; one NICU per city with a population of over 200,000 people and one NICU per autonomous province. NICUs are only necessary in metropolitan cities. (B) Opinions on the necessity of PICUs. A PICU should be mandatory in every hospital; one PICU per city with a population of over 200,000; one PICU per autonomous province; PICUs are only necessary in metropolitan cities.
NICU = neonatal intensive care unit, PICU = pediatric intensive care unit.
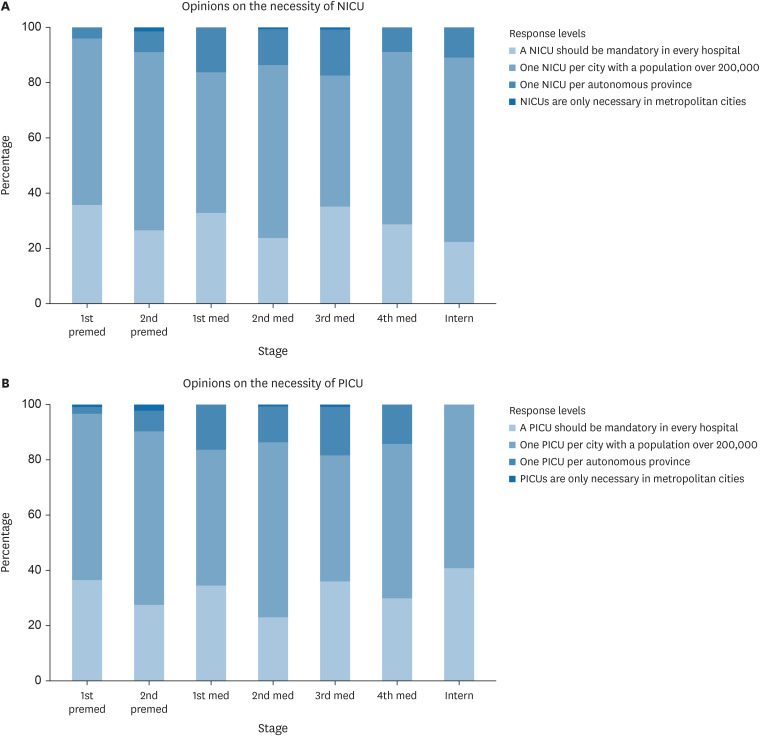
Fig. 5
Influence of various factors on challenges faced by medical students in choosing a vital department. Litigation risk, psychological burden, social perception, knowledge update, staff shortage anxiety.
Issues related to low birth rates
DISCUSSION
In this study, we investigated the determinants influencing the departmental choices of medical students and interns, with a particular focus on pediatrics. Several studies have identified the factors influencing the choice of departments.
9101112 Several factors have been identified as affecting the choice of pediatrics, such as early exposure to pediatrics, lifestyle factors, varied clinical work and enjoyable working atmosphere, and role models and mentors.
1314151617 However, this study considers South Korea’s unique challenges, such as declining birth rates and reluctance toward choosing pediatrics. Analyzing the medical students’ and interns’ responses helped us understand factors affecting the pediatric workforce, including demographic trends, education, and attitudes toward pediatrics and child-rearing. We also explored how awareness of recent incidents in pediatrics impacts their specialty views. This study offers insights into influences on medical students’ and interns’ specialty choices, avoiding broad generalizations or ambitious claims.
The survey and heatmap analysis revealed a clear pattern: interest in pediatrics waned as students progressed, despite the appeal of aiding children and personal satisfaction. Positive motives were offset by concerns over legal issues, guardian interactions, and financial stability. Addressing these issues is key to encouraging pediatrics as a choice, by offering legal support, improved communication skills with guardians, and financial or career insights. The survey data revealed that 67.55% of students perceive mass media and societal views as negative influences on deciding to choose pediatrics. This highlights the need for efforts to improve these perceptions. Enhancing pediatrics' image with strategic communications could markedly persuade students’ specialty selections, advocating for efforts to better represent and value the field socially.
According to the survey, ongoing policies showed mixed effectiveness. Some students were influenced by the prospect of higher salaries in pediatrics; however, the varied responses indicated that financial incentives alone were insufficient to attract them to this specialty. The strong preference for a shorter residency highlights students’ desire to enter the professional field sooner. However, skepticism toward increasing medical school quotas to solve the pediatric workforce shortage suggests that students seek more specific measures. Conversely, the acknowledgment that higher medical school quotas may affect personal career choices suggests uncertainty regarding the long-term effects of such policies. This feedback underscores the urgent need for strategies beyond expanding medical school admissions. Emphasizing a targeted exploration of pediatric training and career development nuances is crucial, strongly suggesting that increasing the number of medical students is not the solution to pediatric workforce challenges.
The analysis indicated a gradational increase in medical students' awareness of pediatric incidents as they progressed through their academic stages. Despite this growing awareness, its influence on specialty selection remained consistent across all levels, suggesting the presence of other decisive factors. Additionally, the observed escalation in litigation concerns among more advanced students highlights the recognition of the medicolegal realities that accompany clinical practice. This pattern underscores the need to consider comprehensive educational strategies that address both the awareness of clinical issues and broader implications for career choices in pediatrics.
Regarding life-critical care in pediatrics, students highly value vital departments but are deterred by litigation risks and psychological burdens of intensive care, consistent across educational stages. These concerns were consistent across different educational stages. Implementing psychological support for healthcare professionals and legal safeguards could reduce fears and motivate students toward these essential pediatric fields. These steps would aid current students and ensure workforce sustainability in critical care areas.
The limitations of our study include its single-center design, which may not represent the broader population, and the uneven distribution of participant demographics because not all students could participate. Additionally, the reliance on online surveys introduces uncertainty regarding the sincerity of responses. Nonetheless, the survey was meticulously tailored to reflect the unique circumstances in Korea, providing a direction for addressing declining interest in pediatrics. Despite being conducted at a single center, the considerable participation rate strengthens the study’s validity. It suggests that the findings could provide valuable insights into the factors influencing specialty choice among medical students in similar contexts.
In conclusion, our findings suggest that, while medical students recognize the importance of pediatrics, their interest wanes as they progress through their education, likely due to increased awareness of the specialty’s challenges. Consistent concern across educational stages regarding legal risks and psychological burdens highlights the need for strategic interventions to support students’ career decisions. These results emphasize the importance of addressing the perceptions and realities of pediatric practice to foster a robust future workforce in the pediatrics field. Future research should aim to collect nationwide data for broader insights.
ACKNOWLEDGMENTS
We acknowledge the assistance of ChatGPT provided by OpenAI (United States) in English proofreading, figure generation, and statistical analysis in our study.
References
4. Kim J. In an era of low birth rates, support measures for children and adolescents in crisis. Med Policy Forum. 2023; 20(4):48–53.
7. Woo BS. Essential medical crisis and medical school capacity. Med Policy Forum. 2023; 21(2):3–6.
9. Khamees A, Awadi S, Al Sharie S, Faiyoumi BA, Alzu’bi E, Hailat L, et al. Factors affecting medical student’s decision in choosing a future career specialty: a cross-sectional study. Ann Med Surg (Lond). 2022; 74:103305. PMID:
35145673.
10. Al-Beitawi SN, Al-Shatanawi TN, Qudsieh SA, Abu Marar EI, Al Zoubi MS, Al-Zubi M. 6th year medical students’ future specialty preferences: a cross-sectional study. Ann Med Surg (Lond). 2021; 66:102373. PMID:
34040768.
11. Alawad AA, Khan WS, Abdelrazig YM, Elzain YI, Khalil HO, Ahmed OB, et al. Factors considered by undergraduate medical students when selecting specialty of their future careers. Pan Afr Med J. 2015; 20:102. PMID:
26090050.
12. Smith F, Lambert TW, Goldacre MJ. Factors influencing junior doctors’ choices of future specialty: trends over time and demographics based on results from UK national surveys. J R Soc Med. 2015; 108(10):396–405. PMID:
26432808.
13. Roberts C, Vick D, Oakley J. G198(P) Students’ perceptions of paediatrics and the impact of a careers workshop. Arch Dis Child. 2020; 105(Suppl 1):A70–A71.
14. Kahvo M, Whelan R, Vallabhaneni P. Why choose paediatrics? A scoping review of factors affecting the choice of paediatrics as a career. Eur J Pediatr. 2023; 182(1):9–23. PMID:
36316579.
15. Balmer DF, Gottlieb-Smith RJ, Hobday PM, Long M, Carraccio C, Bale JF, et al. Pediatric career choice: insights from a novel, medical school pathway program. Acad Pediatr. 2020; 20(1):97–103. PMID:
31404708.
16. Amudhan AS, Palaniyandi A, Rajan M, Parthiban P, Rajendraprasath S, Saminathan T, et al. The Driving factors important for evaluation student’s opinion which influenced decision making of career choice: pediatrics as a career choice as an example. Acta Inform Med. 2021; 29(2):94–98. PMID:
34584330.
17. Shortland D, Roland D, Lumsden DE, Ewing C, L’Esperance V, McColgan M, et al. Career intentions and choices of paediatricians entering training in the UK. Arch Dis Child. 2015; 100(6):537–541. PMID:
25538188.
SUPPLEMENTARY MATERIALS
Supplementary Fig. 1
Analysis of medical students’ considerations for family planning and perceived reasons for low birth rate by educational stage. (A) Main considerations for wanting children by stage: economic stability; life balance; partner’s opinion; parenting burden; children’s education burden; living environment; career interruption. (B) Reasons for low birth rate: economic burden of childcare; lack of childcare facilities/personnel; career disruption due to childbirth/childcare; quality and accessibility of housing; unequal punishment of sex offenders; lack of economic and time resources for child education and development; increased parental burden due to societal expectations; complexity in education and childcare due to social perception changes; increased childcare burden due to overemphasis in media; feeling of deprivation and inequality from media portrayal; social division due to prevalence of hate speech; social stress and anxiety due to excessive competitive psychology
jkms-39-e211-s002.doc




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download