1. Kim YE, Park H, Jo MW, Oh IH, Go DS, Jung J, et al. Trends and patterns of burden of disease and injuries in Korea using disability-adjusted life years. J Korean Med Sci. 2019; 34(Suppl 1):e75. PMID:
30923488.

2. Ock M, Han JW, Lee JY, Kim SH, Jo MW. Estimating quality-adjusted life-year loss due to noncommunicable diseases in Korean adults through to the year 2040. Value Health. 2015; 18(1):61–66. PMID:
25595235.


3. Drach-Zahavy A. Workplace health friendliness: a cross level model for predicting workers' health. J Occup Health Psychol. 2008; 13(3):197–213. PMID:
18572992.


4. Shanafelt TD, Mungo M, Schmitgen J, Storz KA, Reeves D, Hayes SN, et al. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc. 2016; 91(4):422–431. PMID:
27046522.

5. Tawfik DS, Profit J, Morgenthaler TI, Satele DV, Sinsky CA, Dyrbye LN, et al. Physician burnout, well-being, and work unit safety grades in relationship to reported medical errors. Mayo Clin Proc. 2018; 93(11):1571–1580. PMID:
30001832.



6. Lee W, Pyo J, Jang SG, Choi JE, Ock M. Experiences and responses of second victims of patient safety incidents in Korea: a qualitative study. BMC Health Serv Res. 2019; 19(1):100. PMID:
30728008.



7. Oreskovich MR, Shanafelt T, Dyrbye LN, Tan L, Sotile W, Satele D, et al. The prevalence of substance use disorders in American physicians. Am J Addict. 2015; 24(1):30–38. PMID:
25823633.


8. Shanafelt TD, Balch CM, Dyrbye L, Bechamps G, Russell T, Satele D, et al. Special report: suicidal ideation among American surgeons. Arch Surg. 2011; 146(1):54–62. PMID:
21242446.

9. Balch CM, Oreskovich MR, Dyrbye LN, Colaiano JM, Satele DV, Sloan JA, et al. Personal consequences of malpractice lawsuits on American surgeons. J Am Coll Surg. 2011; 213(5):657–667. PMID:
21890381.


10. Compton MT, Frank E. Mental health concerns among Canadian physicians: results from the 2007–2008 Canadian Physician Health Study. Compr Psychiatry. 2011; 52(5):542–547. PMID:
21129737.


11. Kheiraoui F, Gualano MR, Mannocci A, Boccia A, La Torre G. Quality of life among healthcare workers: a multicentre cross-sectional study in Italy. Public Health. 2012; 126(7):624–629. PMID:
22626999.


12. Letvak SA, Ruhm CJ, Gupta SN. Nurses' presenteeism and its effects on self-reported quality of care and costs. Am J Nurs. 2012; 112(2):30–38.
13. Shields M, Wilkins K. Findings from the 2005 National Survey of the Work and Health of Nurses. Ottawa: Health Canada and Canadian Institute for Health Information;2006.
14. Hoben M, Knopp-Sihota JA, Nesari M, Chamberlain SA, Squires JE, Norton PG, et al. Health of health care workers in Canadian nursing homes and pediatric hospitals: a cross-sectional study. CMAJ Open. 2017; 5(4):E791–9.

15. Tountas Y, Demakakos PT, Yfantopoulos Y, Aga J, Houliara L, Pavi E. The health related quality of life of the employees in the Greek hospitals: assessing how healthy are the health workers. Health Qual Life Outcomes. 2003; 1(1):61. PMID:
14613561.


16. Lall MD, Gaeta TJ, Chung AS, Dehon E, Malcolm W, Ross A, et al. Assessment of physician well-being, part one: burnout and other negative states. West J Emerg Med. 2019; 20(2):278–290. PMID:
30881548.



17. Lall MD, Gaeta TJ, Chung AS, Chinai SA, Garg M, Husain A, et al. Assessment of physician well-being, part two: beyond burnout. West J Emerg Med. 2019; 20(2):291–304. PMID:
30881549.



18. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007; 19(6):349–357. PMID:
17872937.


19. Kim YC. Qualitative Research Methodology I: Bricoleur. Paju: Academy Press;2016.
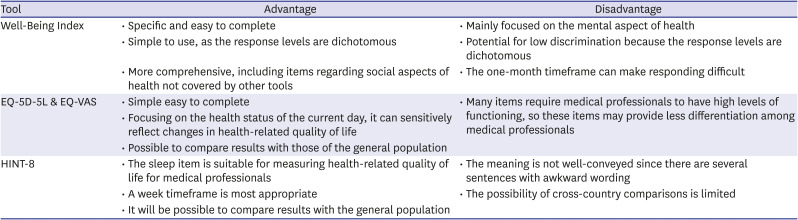
22. Feng Y, Parkin D, Devlin NJ. Assessing the performance of the EQ-VAS in the NHS PROMs programme. Qual Life Res. 2014; 23(3):977–989. PMID:
24081873.


23. Lee J, Ahn J. A study on deriving a conversion formulae using mapping between HINT-8 and EQ-5D instruments. Korean J Health Econ Policy. 2019; 25(1):77–103.
24. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005; 15(9):1277–1288. PMID:
16204405.


25. Guba EG. Criteria for assessing the trustworthiness of naturalistic inquiries. ECTJ. 1981; 29(2):75.
26. Guba EG, Lincoln YS. Effective Evaluation. 1st ed. San Francisco, CA: Jossey-Bass;1981.
27. Lee HJ, Ock M, Kim SY, Kim SH, Jo MW. Health group and disease group's perceptions of health and health-related quality of life: a focus group study and in-depth interviews. Korean J Health Promot. 2016; 16(1):56–66.

28. Embriaco N, Azoulay E, Barrau K, Kentish N, Pochard F, Loundou A, et al. High level of burnout in intensivists: prevalence and associated factors. Am J Respir Crit Care Med. 2007; 175(7):686–692. PMID:
17234905.

29. Dyrbye LN, Johnson PO, Johnson LM, Halasy MP, Gossard AA, Satele D, et al. Efficacy of the Well-Being Index to identify distress and stratify well-being in nurse practitioners and physician assistants. J Am Assoc Nurse Pract. 2019; 31(7):403–412. PMID:
30829967.


30. Kim SH, Jo MW, Ock M, Lee SI. Exploratory study of dimensions of health-related quality of life in the general population of South Korea. J Prev Med Public Health. 2017; 50(6):361–368. PMID:
29207449.



31. Kim I, Koo MJ, Lee HE, Won YL, Song J. Overwork-related disorders and recent improvement of national policy in South Korea. J Occup Health. 2019; 61(4):288–296. PMID:
31025505.



32. Han ER, Chung EK. The perception of medical residents and faculty members on resident duty hour regulation. Korean J Med Educ. 2020; 32(1):67–72. PMID:
32130852.



33. Pyo J, Choi EY, Lee W, Jang SG, Park YK, Ock M, et al. Physicians' difficulties due to patient safety incidents in Korea: a cross-sectional study. J Korean Med Sci. 2020; 35(17):e118. PMID:
32356419.

34. Ock M, Lim SY, Jo MW, Lee SI. Frequency, expected effects, obstacles, and facilitators of disclosure of patient safety incidents: a systematic review. J Prev Med Public Health. 2017; 50(2):68–82. PMID:
28372351.



35. Edrees H, Connors C, Paine L, Norvell M, Taylor H, Wu AW. Implementing the RISE second victim support programme at the Johns Hopkins Hospital: a case study. BMJ Open. 2016; 6(9):e011708.

36. Jo MW, Lee HJ, Kim SY, Kim SH, Chang H, Ahn J, et al. Development and validation of a novel generic health-related quality of life instrument with 20 Items (HINT-20). J Prev Med Public Health. 2017; 50(1):38–59. PMID:
28173686.







 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download