Introduction
Metabolic Syndrome (MetS) is defined as the coexistence of several metabolic risk factors, and it is a risk factor for type 2 diabetes and atherosclerotic cardiovascular disease (ASCVD) [
1,
2]. MetS is common among Koreans, as its prevalence in the population is approximately 30% [
3], and this statistic has attracted attention in Korea because cardiovascular disease and diabetes have been ranked the 3
rd and 5
th leading causes of mortality, respectively [
4].
The etiology of MetS is not clear, although lifestyle components, including diet, are considered metabolic risk factors [
2]. Recently, comprehensive approaches, such as the analyses of dietary patterns or diet quality indices and scores, focusing on more than a single nutrient have been used to investigate the association between diet and disease. These studies have demonstrated that the "meat and alcohol" diet pattern was associated with a higher risk for developing metabolic abnormalities, while the "Korean healthy" diet pattern was related to a reduced risk for the development of these abnormalities among Korean individuals [
5].
Dietary quality indices or scores that are based on recommended diets or dietary guidelines have been used to obtain a comprehensive idea of food intake. From a long-term follow-up study of 300 healthy women, the composite nutritional risk, which is a validated 19-nutrient index used to assess diet quality, was found to predict the development of abdominal obesity and MetS [
6]. From a cross-sectional study, Fogli-Cawley et al. reported that adherence to the 2005 Dietary Guidelines for Americans Adherence Index (DGAI) was associated with a lower prevalence of MetS [
7]. However, dietary indices do not consider the correlation between the structure of the food and the nutrient intake, and these represent only the formal sums of non-adjusted single effects [
8]. Recently, a hybrid method was developed and tested; the weighted DGAI (wDGAI) method weighs dietary components based on their adherence to dietary recommendations and uses a data-driven dietary pattern approach as well as a criteria-based dietary score approach [
9]. Higher wDGAI scores were found to be significantly associated with slower progression of atherosclerosis, although these associations were not found in a longitudinal study [
9].
Consumption of a diet consistent with dietary guidelines has beneficial effects on the prevention of chronic diseases and promotes the health of the general population [
10]. Recently, food-based dietary guidelines, such as the Korean Food Guidance System (KFGS), have been developed in many countries as practical tools for evaluating and planning healthy diets. The KFGS was developed using the Dietary Reference Intakes for Koreans (KDRIs) and the Dietary Guidelines for Koreans. However, as far as we know, there have not been studies done to assess the association between the adherence to the Dietary Guidelines and the disease risk among Koreans using the latest KFGS. Therefore, in this study, we examined the association between the adherence to the KFGS, as established using the revised 2010 KDRIs, and presence of metabolic abnormalities in Korean individuals.
Subjects and Methods
Subjects
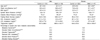
Six hundred and sixty-three adults 30-59 years of age were recruited between June and September 2009 and between May and October 2010 at the Bundang Jesaeng General Hospital (BJGH) in Sungnam, Korea. Participants from the 2009 recruitment were residents of the South Gyeonggi Province and nearby Seoul; they were recruited by advertisement. Participants recruited in 2010 had received a medical checkup at BJGH between October 2009 and October 2010. The subjects fit the inclusion criteria if they were not taking any regular medications and had not been diagnosed with any fulminant disease. Five hundred and ninety-six adults who had completed the dietary assessment and who expressed biomarkers for a MetS diagnosis were included in the analysis. This study was approved by the Institutional Review Board at the BJGH, and written, informed consent was received from each participant.
Assessment of anthropometric measures, biomarkers, and blood pressure
The body weights and heights were measured using an automatic height and weight scale (GL-150; G-Tech International, Korea). The waist circumference was measured over light clothing with a tape measure at the narrowest part of the waist. Blood pressure was measured using sphygmomanometer (EW 3152; Panasonic, Japan). Venous blood was collected after at least 8 hours of fasting. The measurements for the serum levels of TG, HDL cholesterol, and glucose were performed using an enzymatic colorimetric test (GPO-PAP), an enzymatic method, and HK-G6PD (UV), respectively, at the Department of Laboratory Medicine of BJGH.
Dietary assessment
All subjects were interviewed once for a 24-hr recall at the hospital and submitted a 2-day dietary record within 2 weeks from the day of the interview. The interviews were conducted by trained dietitians. Using a 2-dimensional model to represent the amount of food intake, the subjects were instructed how to complete the dietary record. Three days (2 weekdays and 1 weekend day) of dietary data were collected in total. The dietary data were analyzed using the Diet Evaluation System program (DES), which is a web-based computer program for dietary assessment developed by the Human Nutrition Lab at Seoul National University.
Diagnostic criteria for Mets
The existence of MetS was defined according to the modified National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) criteria. For the relationship between waist circumference and MetS, a population-specified cut-off for circumference from the Korean Society for the Study of Obesity was used. Those individuals who tested positive for 3 out of 5 components (waist circumference ≥ 90 cm for men and ≥ 85 cm for women; blood TG ≥ 150 mg/dL; HDL cholesterol < 40 mg/dL for men and < 50 mg/dL for women; systolic blood pressure ≥ 130 mmHg or diastolic blood pressure ≥ 85 mmHg; or fasting blood glucose ≥ 100 mg/dL) were classified as having MetS, and the others were classified as the control group.
Adherence to the Korean Food Guidance System
The Korean Food Guidance System (KFGS) consists of six major food groups, their target patterns and the representative food items in each food group. The six major food groups consist of "Grains", "Meat, Fish, Eggs, and Beans", "Vegetables", "Fruits", "Milk and Dairy products", and "Oils, Fats, and Sugars". Furthermore, this system consists of the following two types of target patterns: the A-type pattern suggests two servings of milk and dairy products, and the B-type pattern suggests one serving of milk and dairy products. These different types exist because the calcium requirements of children and adults differ. Each type of target pattern has a recommended serving suggestion based on the level of energy intake. In this study, B-type target patterns were adopted for the recommended servings for each food group, and these patterns had 4 levels of energy (1,600 kcal, 1,900 kcal, 2,000 kcal, and 2,400 kcal). For example, the 1,600 kcal energy level recommended 3 servings of grains; 2.5 servings of meat, fish, eggs, and beans; 5 servings of vegetables; 1 serving of fruits; 1 serving of milk and dairy products; and 3 servings of oils, fats, and sugars.
Prior to the calculation of the daily servings from each food group of each subject, a food group composition table was established for each food based on the KFGS. The foods that were not listed as representative food items in the KFGS were classified by the authors based on their energy and nutrient composition, and mixed foods were classified by recipe. The daily servings of each food group that were consumed by each subject were calculated using the food group composition table.
After the estimated energy requirement (EER) for each subject was calculated, this value was used to identify the target pattern energy level for each subject. As the precise physical activity level of each subject was not determined, the subjects' physical activity levels were considered sedentary because the majority of Koreans have been reported to have sedentary life styles [
11]. The subject's adherence score to the recommended dietary servings was defined as the percentage of consumed daily servings from each food group out of the recommended servings based on each subject's target pattern. The target pattern of 2,400 kcal was used for the recommended food group consumption for subjects whose EER exceeded 2,400 kcal.
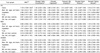
Statistical analysis
The differences in the means of continuous variables were tested by an analysis of covariance (PROC GLM in SAS). The associations between the nutrient intakes, the consumed servings from each food group and the existence of MetS or its components were analyzed by multiple logistic regression analyses with adjustments for age, sex, mean daily energy intake, and BMI (except for MetS and elevated waist circumference). In the logistic regression model, the servings from 6 food groups were included together, and these could be adjusted according to each other. The adherence to the recommended servings was divided into quartiles, and odds ratios were calculated by setting the nearest quartile to 100% as a reference. All of the statistical analyses were performed using SAS software (Statistic Analysis System; version 9.2, SAS Institute, Cary, NC.).
Discussion
This study was conducted to evaluate whether the consumption of a diet with good adherence to the KFGS was associated with the absence of metabolic abnormalities in Korean adults 30 to 59 years of age. The results from this study indeed showed that adherence to the recommended servings of milk and dairy products, vegetables, and fruit was associated with the reduced incidence of metabolic abnormalities. However, the relationships between the consumption of or adherence to the recommended servings of meat, fish, eggs, and beans as well as oils, fats, and sugars and presence of metabolic abnormalities differed based on the metabolic parameter analyzed.
Cross-sectional studies [
12-
15] have documented the association between dairy consumption and MetS. Based on the Third National Health and Nutrition Examination Survey (NHANES III), Bradlee et al. [
12] reported that the intake of dairy, grains and total fruit and vegetables was inversely associated with central obesity among adolescents. Furthermore, a study from the Third Korean National Health and Nutrition Examination Survey (KNHANES III) found that Korean overweight adults who drank milk more frequently (once a day or more) had a lower likelihood of having MetS [
13]. This association between dairy consumption and MetS has also been reported by certain prospective studies. From the French Epidemiological Study on the Insulin Resistance Syndrome (DESIR) patient cohort, a greater consumption of dairy products was associated with a lower incidence of MetS as well as impaired glucose tolerance and diabetes [
14]. The protective effect of dairy consumption has also been reported from the Atherosclerosis Risk in Communities (ARIC) patient cohort [
15].
The results from our study are consistent with findings that have reported that fruit, as part of a healthy diet such as the Dietary Approaches to Stop Hypertension (DASH) eating plan [
16] or a vegetarian diet [
17], was associated with reduced metabolic risk.
The relationship between the adherence to the guidelines for the consumption of meat, fish, eggs, and beans and the components of MetS was somewhat contradictory. Those subjects in the highest quartile for meat, fish, eggs, and beans consumption were less likely to have larger waist circumferences. Those who consumed meat, fish, eggs, and beans slightly below the recommended number of servings were less likely to have elevated fasting glucose levels. As this food group contains various protein-containing foods, such as red meat, for which a greater intake is related to MetS and central obesity [
18], and beans, which have a low in glycemic index, this association should be interpreted carefully. These inconsistencies could be partially explained by the fact that subjects in the highest quartile (who consumed beyond the recommended servings) showed significantly reduced energy intake from carbohydrates (57.8 ± 7.8%) and higher energy intake from protein (18.3 ± 3.1%) compared to those in the reference quartile (60.2 ± 7.2% for carbohydrate energy and 16.9 ± 2.4% for protein energy), while the energy intake from fat was not different between these two groups (23.0 ± 6.2 and 23.8 ± 6.3 for the highest and reference quartiles, respectively). Subjects in the highest quartile consumed more fish (2.4 ± 1.7 servings) than those in the reference quartile (1.5 ± 0.9 servings), whereas the extent of the difference in the consumption of meat, eggs, and beans approximately 0.1 servings. A reduced energy intake from carbohydrate sources and a greater energy intake from protein could be related to obesity prevalence [
19], and a high intake of fish could be beneficial for the prevention of MetS and abdominal obesity [
20].
The consumption of more servings of oils, fats, and sugars was associated with a lower risk of having elevated blood pressure. In addition, subjects who consumed more servings of oils, fats, and sugars tended to consume more energy and nutrients. However, there is no clear explanation for the observed association between the increased intake of oils, fats, and sugars and the lower risk of elevated blood pressure, although the reduced consumption of salted vegetables by subjects who consumed more servings of oils, fats, and sugars may suggest a possible explanation. Furthermore, the blood pressure levels of the subjects in this study were not extraordinarily high, as the mean systolic and diastolic blood pressures for MetS subjects were at the lower end of the elevated blood pressure range (130/85 mmHg).
In this study, the distribution patterns of the adherence to the recommended servings of each food groups were quite different. The interquartile range for the adherence scores for grains were the smallest at 29.1% and was followed by that for vegetables (54.6%) and for meat, fish, eggs, and beans (59.8%). As typical Korean meals consist of cooked rice, savory soup, seasoned side dishes made with raw, pickled, and steamed vegetables, and protein-rich foods, such as tofu, fish, and meat, these three food groups are usually consumed as meals rather than desserts or snacks among Koreans [
21]. In contrast, the consumption of fruits and milk and dairy products had wider distribution ranges. The interquartile ranges of the adherence scores for these food groups were greater than 90%. For milk and dairy products, at least 25% of subjects consumed less than 5% of the recommended servings, and less than 25% of subjects consumed the recommended numbers of servings. On the other hand, the adherence scores for oils, fats, and sugars had a distribution near 100% for most subjects. Representative food items in this food group include butter, mayonnaise, coffee creamer, vegetable oils, coffee mix (instant coffee with sugar and powdered creamer), honey, sugar, syrup, and candy. Besides those used for cooking, these food items should not be consumed beyond the recommended number of servings because they provide empty calories [
22]. However, the majority of people were found to consume these food items in excess of the recommended servings. Independent of energy intake, the consumption of additional servings of oils, fats, and sugars was associated with the risk of having an elevated waist circumference. This difference between the recommended and the actual intake levels suggests the need for a public health policy or a nutritional education program that emphasizes the benefits of a diet low in oils, fats, and sugars. In young Finnish men, a distinction was made between core foods (healthy foods) and extra foods (unhealthy foods that provide lots of oils, fats, and sugars); nutritional education was associated with core foods but not with extra foods [
23]. Therefore, a food policy or program should involve the food choices related to oils, fats, and sugars.
The risk for elevated TG levels in men was decreased by the addition of a single serving of grains, while this association was reversed for women. The distribution of the range of grains intake was broader for women (0.9-6.9 servings per day) than men (1.3-5.0 servings per day), and the majority of men consumed grains below the recommended servings. Thus, it should not be interpreted that an increased consumption of grains would decrease the existence of elevated TG levels in men. Although only a 3-day alcohol intake was recorded, this intake was greater in men who consumed grains below the recommended levels (2.15 ± 2.93 drinks per day) compared to those who consumed above the recommended levels (1.33 ± 2.35 drinks per day). Also, there was a weak but significant negative correlation between the servings of grains and the number of drinks in men (correlation coefficient = -0.1790, P < 0.01), but this correlation was not observed in women.
This was the first study to evaluate the adherence of individuals to the revised Korean Food Guidance System and explore the association between adherence and the existence of metabolic abnormalities. However, there were several limitations of this study. First, information on the subject's lifestyle, such as smoking, alcohol intake, and physical activity, was incomplete, and therefore, these variables could not be included as covariates in the statistical analyses. Second, this was a cross-sectional study conducted at a hospital, and it did not use a nationally representative sample. Therefore, the association between diet and disease should be interpreted with limitations.
In summary, adherence to the KFGS was associated with beneficial MetS parameters, although this needs to be confirmed by prospective studies to demonstrate causal association. These results can be used for the development of a guideline adherence index to investigate the relationship between the adherence to healthy dietary practice and disease.






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download