1. Lee KB, Kim MK, Kim MJ, Ahn SI, Hwang YH. The path to glaucoma diagnosis. J Korean Ophthalmol Soc. 2016; 57:794–799.
2. Woo GJ, Kim YJ, Oh KW. Prevalence, awareness and treatment rates of eye diseases: Korea National Health and Nutrition Examination Survey. Public Health Wkly Rep. 2019; 12:717–721.
4. Hyman L, Wu SY, Connell AM, Schachat A, Nemesure B, Hennis A, Leske MC. Prevalence and causes of visual impairment in The Barbados Eye Study. Ophthalmology. 2001; 108:1751–1756. PMID:
11581045.
5. Park SS, Lee HJ, Kim HJ, Lee EH. The prevalence of cataract and glaucoma in Korean. Korean J Vis Sci. 2012; 14:77–84.
6. Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006; 90:262–267. PMID:
16488940.
7. Le A, Mukesh BN, McCarty CA, Taylor HR. Risk factors associated with the incidence of open-angle glaucoma: the visual impairment project. Invest Ophthalmol Vis Sci. 2003; 44:3783–3789. PMID:
12939292.
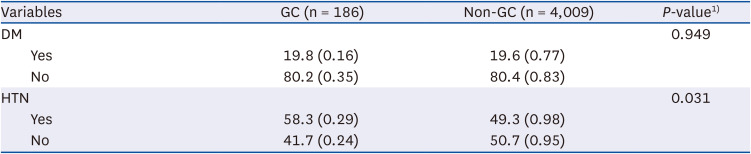
8. McMonnies CW. Glaucoma history and risk factors. J Optom. 2017; 10:71–78. PMID:
27025415.
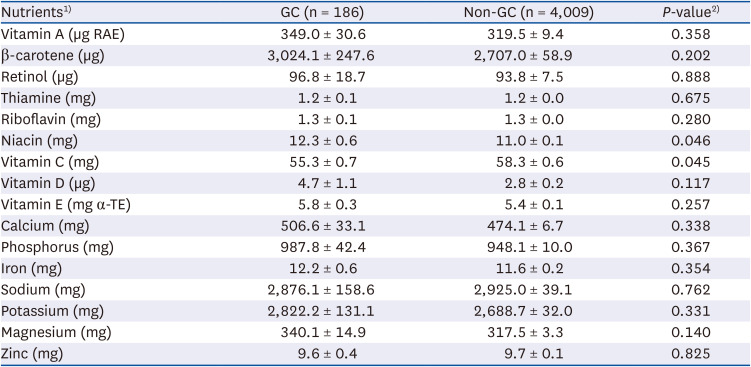
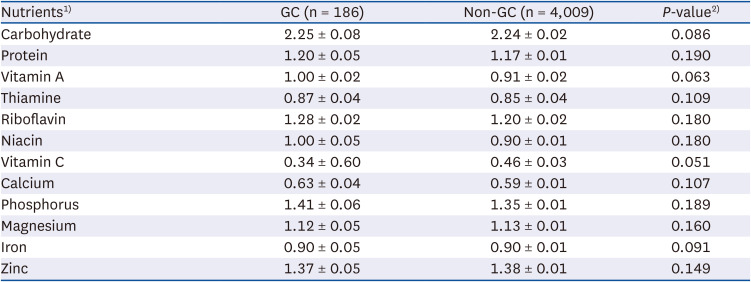
9. Hwang HJ, Shin KO, Shin SJ. A study on the relationship between eye disease and nutrient intake in Korean adults: data from Korean National Health and Nutrition Examination Survey 2015, 2016. J Korean Diet Assoc. 2021; 27:77–91.
10. Pasquale LR, Kang JH. Lifestyle, nutrition, and glaucoma. J Glaucoma. 2009; 18:423–428. PMID:
19680048.
11. Kim H. Relations of glaucoma and dietary pattern factor. J Korean Ophthalmic Opt Soc. 2013; 18:61–65.
12. Ministry of Health and Welfare (KR). The Korean Nutrition Society. Dietary Reference Intakes for Koreans 2020. Sejong: Ministry of Health and Welfare;2020.
13. Ramdas WD, Schouten JS, Webers CA. The effect of vitamins on glaucoma: a systematic review and meta-analysis. Nutrients. 2018; 10:359. PMID:
29547516.
14. Wang SY, Singh K, Lin SC. Glaucoma and vitamins A, C, and E supplement intake and serum levels in a population-based sample of the United States. Eye (Lond). 2013; 27:487–494. PMID:
23429409.
15. Giaconi JA, Yu F, Stone KL, Pedula KL, Ensrud KE, Cauley JA, Hochberg MC, Coleman AL. Study of Osteoporotic Fractures Research Group. The association of consumption of fruits/vegetables with decreased risk of glaucoma among older African-American women in the study of osteoporotic fractures. Am J Ophthalmol. 2012; 154:635–644. PMID:
22818906.
16. Taechameekietichai T, Chansangpetch S, Peerawaranun P, Lin SC. Association between daily niacin intake and glaucoma: National Health and Nutrition Examination Survey. Nutrients. 2021; 13:4263. PMID:
34959814.
17. Jung KI, Kim YC, Park CK. Dietary niacin and open-angle glaucoma: the Korean National Health and Nutrition Examination Survey. Nutrients. 2018; 10:387. PMID:
29565276.
18. Tittler EH, de Barros DS, Navarro JB, Freitas DG, Gheith ME, Siam GA, Spaeth GL. Oral niacin can increase intraocular pressure. Ophthalmic Surg Lasers Imaging. 2008; 39:341–342. PMID:
18717445.
19. Lee SYC, Tseng VL, Avallone TJ, Yu F, Caprioli J, Coleman AL. Associations between niacin intake and glaucoma in the National Health and Nutrition Examination Survey. Invest Ophthalmol Vis Sci. 2021; 62:1604.
20. Kang JH, Pasquale LR, Willett WC, Rosner BA, Egan KM, Faberowski N, Hankinson SE. Dietary fat consumption and primary open-angle glaucoma. Am J Clin Nutr. 2004; 79:755–764. PMID:
15113712.
21. Bengtsson B, Leske MC, Hyman L, Heijl A. Early Manifest Glaucoma Trial Group. Fluctuation of intraocular pressure and glaucoma progression in the early manifest glaucoma trial. Ophthalmology. 2007; 114:205–209. PMID:
17097736.
22. Nguyen CT, Bui BV, Sinclair AJ, Vingrys AJ. Dietary omega 3 fatty acids decrease intraocular pressure with age by increasing aqueous outflow. Invest Ophthalmol Vis Sci. 2007; 48:756–762. PMID:
17251475.
23. Wang YE, Tseng VL, Yu F, Caprioli J, Coleman AL. Association of dietary fatty acid intake with glaucoma in the United States. JAMA Ophthalmol. 2018; 136:141–147. PMID:
29270632.
24. Perez CI, Singh K, Lin S. Relationship of lifestyle, exercise, and nutrition with glaucoma. Curr Opin Ophthalmol. 2019; 30:82–88. PMID:
30562241.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download