1. Mucke L. Neuroscience: Alzheimer’s disease. Nature. 2009; 461:895–897. PMID:
19829367.
2. Lane CA, Hardy J, Schott JM. Alzheimer’s disease. Eur J Neurol. 2018; 25:59–70. PMID:
28872215.
3. Chang EH, Chavan SS, Pavlov VA. Cholinergic control of inflammation, metabolic dysfunction, and cognitive impairment in obesity-associated disorders: mechanisms and novel therapeutic opportunities. Front Neurosci. 2019; 13:263. PMID:
31024226.
4. Block ML, Hong JS. Microglia and inflammation-mediated neurodegeneration: multiple triggers with a common mechanism. Prog Neurobiol. 2005; 76:77–98. PMID:
16081203.
5. Abdelhak A, Foschi M, Abu-Rumeileh S, Yue JK, D’Anna L, Huss A, Oeckl P, Ludolph AC, Kuhle J, Petzold A, et al. Blood GFAP as an emerging biomarker in brain and spinal cord disorders. Nat Rev Neurol. 2022; 18:158–172. PMID:
35115728.
6. Jurga AM, Paleczna M, Kadluczka J, Kuter KZ. Beyond the GFAP-astrocyte protein markers in the brain. Biomolecules. 2021; 11:1361. PMID:
34572572.
7. Zhang S, Wu M, Peng C, Zhao G, Gu R. GFAP expression in injured astrocytes in rats. Exp Ther Med. 2017; 14:1905–1908. PMID:
28962102.
8. Bettcher BM, Olson KE, Carlson NE, McConnell BV, Boyd T, Adame V, Solano DA, Anton P, Markham N, Thaker AA, et al. Astrogliosis and episodic memory in late life: higher GFAP is related to worse memory and white matter microstructure in healthy aging and Alzheimer’s disease. Neurobiol Aging. 2021; 103:68–77. PMID:
33845398.
9. Tang KS. The cellular and molecular processes associated with scopolamine-induced memory deficit: a model of Alzheimer’s biomarkers. Life Sci. 2019; 233:116695. PMID:
31351082.
10. Anand P, Singh B. A review on cholinesterase inhibitors for Alzheimer’s disease. Arch Pharm Res. 2013; 36:375–399. PMID:
23435942.
11. Pepeu G, Grazia Giovannini M. The fate of the brain cholinergic neurons in neurodegenerative diseases. Brain Res. 2017; 1670:173–184. PMID:
28652219.
12. Rosas-Ballina M, Tracey KJ. Cholinergic control of inflammation. J Intern Med. 2009; 265:663–679. PMID:
19493060.
13. Bajo R, Pusil S, López ME, Canuet L, Pereda E, Osipova D, Maestú F, Pekkonen E. Scopolamine effects on functional brain connectivity: a pharmacological model of Alzheimer’s disease. Sci Rep. 2015; 5:9748. PMID:
26130273.
14. Choi JH, Lee EB, Jang HH, Cha YS, Park YS, Lee SH. Allium hookeri extracts improve scopolamine-induced cognitive impairment via activation of the cholinergic system and anti-neuroinflammation in mice. Nutrients. 2021; 13:2890. PMID:
34445062.
15. Klinkenberg I, Blokland A. The validity of scopolamine as a pharmacological model for cognitive impairment: a review of animal behavioral studies. Neurosci Biobehav Rev. 2010; 34:1307–1350. PMID:
20398692.
16. Chen WN, Yeong KY. Scopolamine, a toxin-induced experimental model, used for research in Alzheimer’s disease. CNS Neurol Disord Drug Targets. 2020; 19:85–93. PMID:
32056532.
17. Wang S, Hu Y, Tan W, Wu X, Chen R, Cao J, Chen M, Wang Y. Compatibility art of traditional Chinese medicine: from the perspective of herb pairs. J Ethnopharmacol. 2012; 143:412–423. PMID:
22871585.
18. Rolnik A, Olas B. The plants of the Asteraceae family as agents in the protection of human health. Int J Mol Sci. 2021; 22:3009. PMID:
33809449.
19. Bessada SM, Barreira JC, Oliveira MB. Asteraceae species with most prominent bioactivity and their potential applications: a review. Ind Crops Prod. 2015; 76:604–615.
20. Lee HH, Lee SY. Cytotoxic and antioxidant effects of Taraxacum coreanum Nakai. and T. officinale WEB. extracts. Korean J Med Crop Sci. 2008; 16:79–85.
21. Park MS, So JS, Bahk GJ. Antioxidative and anticancer activities of water extracts from different parts of Taraxacum coreanum Nakai cultivated in Korea. J Korean Soc Food Sci Nutr. 2015; 44:1234–1240.
22. Jin Y, Qu C, Tang Y, Pang H, Liu L, Zhu Z, Shang E, Huang S, Sun D, Duan JA. Herb pairs containing
Angelicae Sinensis Radix (Danggui): a review of bio-active constituents and compatibility effects. J Ethnopharmacol. 2016; 181:158–171. PMID:
26807913.
23. Jiang M, Zhao S, Yang S, Lin X, He X, Wei X, Song Q, Li R, Fu C, Zhang J, et al. An “essential herbal medicine”-licorice: a review of phytochemicals and its effects in combination preparations. J Ethnopharmacol. 2020; 249:112439. PMID:
31811935.
24. Shang H, Zhang B, Wang Y, Gao X, Zhao Y. A method for proportion screening of TCM small prescriptions. Chin J Exp Tradit Med Formulae. 2003; 3:1–3.
25. Sheng YM, Chen L, Xie XL. Optimization of the best ratio of Astragalus polysaccharide and Astragalus saponin for immunomodulation based on increase-decrease baseline geometric proportion design method. Chin J Hosp Pharm. 2016; 36:59–62.
26. Chen CC, Qin XM, Du GH, Zhou YZ. The “compatible art” of effective components from traditional Chinese medicine: research on the compatibility and proportion of effective components. Acta Pharm Sinica. 2019; 54:808–817.
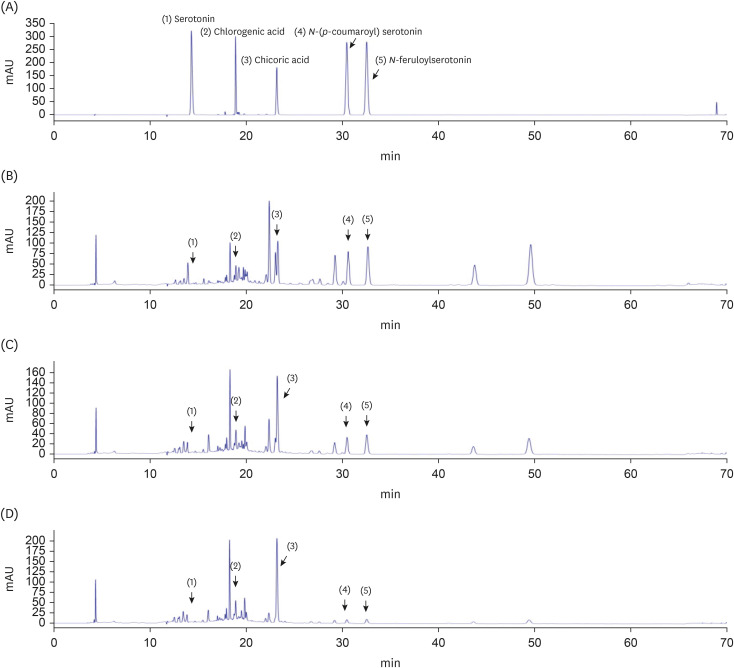
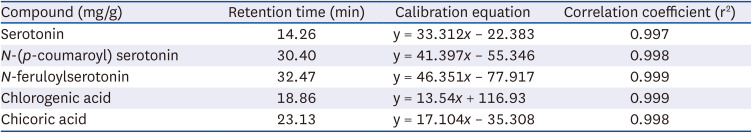
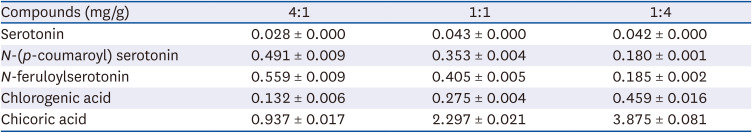
27. Mani V, Lee SK, Yeo Y, Hahn BS. A metabolic perspective and opportunities in pharmacologically important safflower. Metabolites. 2020; 10:253. PMID:
32560514.
28. Akhtar U, Wankhade AM, Vyas JV, Paithankar VV. A review on: phytoconstituents, traditional and medicinal uses of Taraxacum offinale (Dandelion). J Pharmacogn Phytochem. 2023; 15:139–144.
29. Mahboubi M, Mahboubi M. Hepatoprotection by dandelion (Taraxacum officinale) and mechanisms. Asian Pac J Trop Biomed. 2020; 10:1–10.
30. Kim JH, He MT, Kim MJ, Yang CY, Shin YS, Yokozawa T, Park CH, Cho EJ. Safflower (
Carthamus tinctorius L.) seed attenuates memory impairment induced by scopolamine in mice via regulation of cholinergic dysfunction and oxidative stress. Food Funct. 2019; 10:3650–3659. PMID:
31165850.
31. Kim EJ, Jung IH, Van Le TK, Jeong JJ, Kim NJ, Kim DH. Ginsenosides Rg5 and Rh3 protect scopolamine-induced memory deficits in mice. J Ethnopharmacol. 2013; 146:294–299. PMID:
23313392.
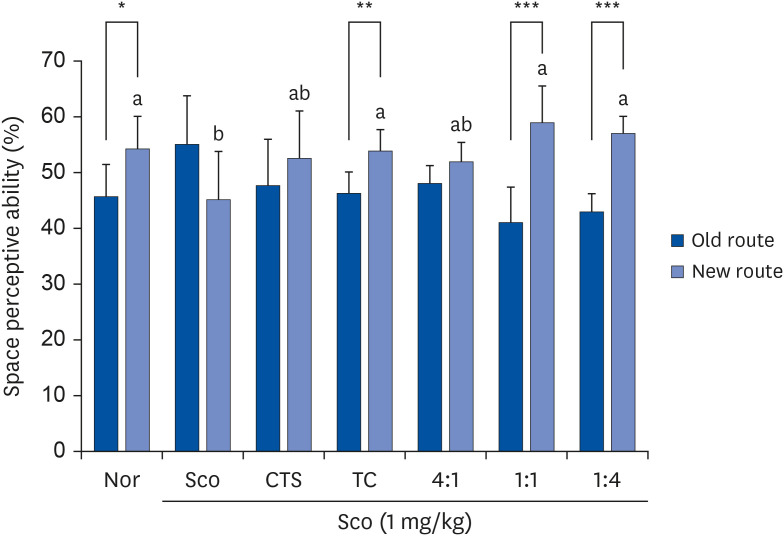
32. Montgomery KC. A test of two explanations of spontaneous alternation. J Comp Physiol Psychol. 1952; 45:287–293. PMID:
14946277.
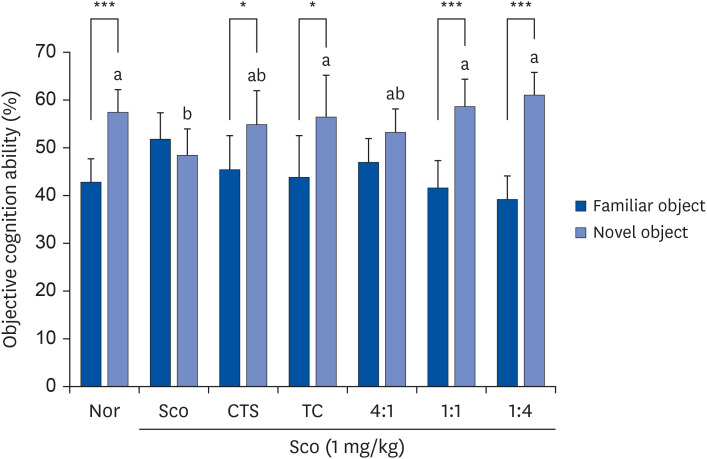
33. Bevins RA, Besheer J. Object recognition in rats and mice: a one-trial non-matching-to-sample learning task to study ‘recognition memory’. Nat Protoc. 2006; 1:1306–1311. PMID:
17406415.
34. Barmak MJ, Nouri E, Shahraki MH, Ghalamfarsa G, Zibara K, Delaviz H, Ghanbari A. Safflower seed oil, a rich source of linoleic acid, stimulates hypothalamic neurogenesis
in vivo
. Anat Cell Biol. 2023; 56:219–227. PMID:
36967238.
35. Liang Y, Wang L.
Carthamus tinctorius L.: a natural neuroprotective source for anti-Alzheimer’s disease drugs. J Ethnopharmacol. 2022; 298:115656. PMID:
36041691.
36. He MT, Kim JH, Kim JH, Park CH, Cho EJ. Combination of Carthamus tinctorius L. seed and Taraxacum coreanum exerts synergistic effects on learning and memory function by regulating metabolism of amyloid beta in mice. J Funct Foods. 2020; 72:104048.
37. Dongare PN, Kadu TB, Pohane AL, Dighade SJ, Patil PG. Review on Pharmacognosy, phytochemistry and pharmacological activity of Taraxacum officinale (Dandelion plant). World J Adv Res Rev. 2021; 12:212–218.
38. Jalili C, Taghadosi M, Pazhouhi M, Bahrehmand F, Miraghaee SS, Pourmand D, Rashidi I. An overview of therapeutic potentials of Taraxacum officinale (dandelion): a traditionally valuable herb with a reach historical background. World Cancer Res J. 2020; 7:e1679.
39. Yoon CS, Ko W, Lee DS, Kim DC, Kim J, Choi M, Beom JS, An RB, Oh H, Kim YC.
Taraxacum coreanum protects against glutamate-induced neurotoxicity through heme oxygenase-1 expression in mouse hippocampal HT22 cells. Mol Med Rep. 2017; 15:2347–2352. PMID:
28260050.
40. Lee AY, Yamabe N, Kang KS, Kim YH, Lee S, Cho EJ. Cognition and memory function of Taraxacum coreanum in an in vivo amyloid-β-induced mouse model of Alzheimer’s disease. Arch Biol Sci. 2014; 66:1357–1366.
41. Sohn MK, Shin YW. A comparative study of memory improving effects of Taraxaci Herba on scopolamine-induced amnesia in mouse. Kor J Herbology. 2012; 27:27–35.
42. van Asselen M, Kessels RP, Neggers SF, Kappelle LJ, Frijns CJ, Postma A. Brain areas involved in spatial working memory. Neuropsychologia. 2006; 44:1185–1194. PMID:
16300806.
43. Falsafi SK, Deli A, Höger H, Pollak A, Lubec G. Scopolamine administration modulates muscarinic, nicotinic and NMDA receptor systems. PLoS One. 2012; 7:e32082. PMID:
22384146.
44. Antonova E, Parslow D, Brammer M, Simmons A, Williams S, Dawson GR, Morris R. Scopolamine disrupts hippocampal activity during allocentric spatial memory in humans: an fMRI study using a virtual reality analogue of the Morris Water Maze. J Psychopharmacol. 2011; 25:1256–1265. PMID:
20823079.
45. Yamazaki M, Okabe M, Yamamoto N, Yarimizu J, Harada K. Novel 5-HT5A receptor antagonists ameliorate scopolamine-induced working memory deficit in mice and reference memory impairment in aged rats. J Pharmacol Sci. 2015; 127:362–369. PMID:
25837935.
46. Antunes M, Biala G. The novel object recognition memory: neurobiology, test procedure, and its modifications. Cogn Process. 2012; 13:93–110. PMID:
22160349.
47. Can MV, Tran AH, Pham DM, Dinh BQ, Le QV, Nguyen BV, Nguyen MT, Nguyen HX, Nguyen NT, Nishijo H.
Willughbeia cochinchinensis prevents scopolamine-induced deficits in memory, spatial learning, and object recognition in rodents. J Ethnopharmacol. 2018; 214:99–105. PMID:
28652013.
48. Brown MW, Aggleton JP. Recognition memory: what are the roles of the perirhinal cortex and hippocampus? Nat Rev Neurosci. 2001; 2:51–61. PMID:
11253359.
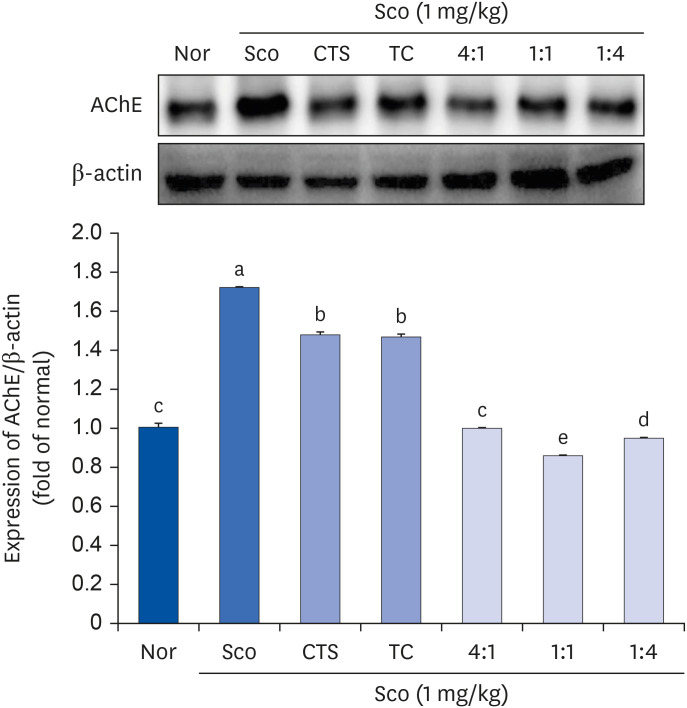
49. Lee YK, Yuk DY, Kim TI, Kim YH, Kim KT, Kim KH, Lee BJ, Nam SY, Hong JT. Protective effect of the ethanol extract of
Magnolia officinalis and 4-O-methylhonokiol on scopolamine-induced memory impairment and the inhibition of acetylcholinesterase activity. J Nat Med. 2009; 63:274–282. PMID:
19343477.
50. Deng G, Wu C, Rong X, Li S, Ju Z, Wang Y, Ma C, Ding W, Guan H, Cheng X, et al. Ameliorative effect of deoxyvasicine on scopolamine-induced cognitive dysfunction by restoration of cholinergic function in mice. Phytomedicine. 2019; 63:153007. PMID:
31301537.
51. Choi SH, Lee AY, Park CH, Shin YS, Cho EJ. Protective effect of
Carthamus tinctorius L. seed on oxidative stress and cognitive impairment induced by chronic alcohol consumption in mice. Food Sci Biotechnol. 2018; 27:1475–1484. PMID:
30319858.
52. Kwon Y, Park HJ, Shin BY, Ryu JH. Ameliorating effect of Taraxacum platycarpum extract in the scopolamine-induced cholinergic blockade mouse model. Korean J Pharmacogn. 2017; 48:119–124.
53. Ahmad A, Ramasamy K, Jaafar SM, Majeed AB, Mani V. Total isoflavones from soybean and tempeh reversed scopolamine-induced amnesia, improved cholinergic activities and reduced neuroinflammation in brain. Food Chem Toxicol. 2014; 65:120–128. PMID:
24373829.
54. Li SP, Wang YW, Qi SL, Zhang YP, Deng G, Ding WZ, Ma C, Lin QY, Guan HD, Liu W, et al. Analogous β-carboline alkaloids harmaline and harmine ameliorate scopolamine-induced cognition dysfunction by attenuating acetylcholinesterase activity, oxidative stress, and inflammation in mice. Front Pharmacol. 2018; 9:346. PMID:
29755345.
55. Agostinho P, Cunha RA, Oliveira C. Neuroinflammation, oxidative stress and the pathogenesis of Alzheimer’s disease. Curr Pharm Des. 2010; 16:2766–2778. PMID:
20698820.
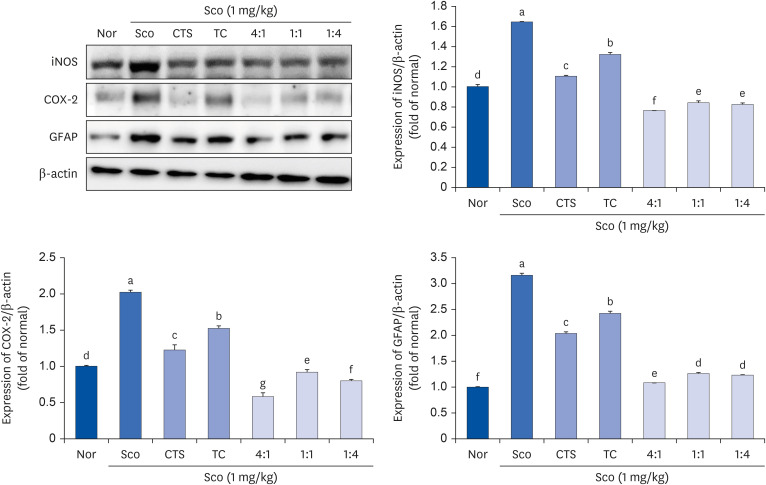
56. Aktan F. iNOS-mediated nitric oxide production and its regulation. Life Sci. 2004; 75:639–653. PMID:
15172174.
57. Khurana K, Kumar M, Bansal N. Lacidipine prevents scopolamine-induced memory impairment by reducing brain oxido-nitrosative stress in mice. Neurotox Res. 2021; 39:1087–1102. PMID:
33721210.
58. Lee JS, Kim HG, Lee HW, Han JM, Lee SK, Kim DW, Saravanakumar A, Son CG. Hippocampal memory enhancing activity of pine needle extract against scopolamine-induced amnesia in a mouse model. Sci Rep. 2015; 5:9651. PMID:
25974329.
59. Khan AA, Iadarola M, Yang HY, Dionne RA. Expression of COX-1 and COX-2 in a clinical model of acute inflammation. J Pain. 2007; 8:349–354. PMID:
17270500.
60. Cui J, Jia J. Natural COX-2 inhibitors as promising anti-inflammatory agents: an update. Curr Med Chem. 2021; 28:3622–3646. PMID:
32942970.
61. Xian YF, Ip SP, Mao QQ, Su ZR, Chen JN, Lai XP, Lin ZX. Honokiol improves learning and memory impairments induced by scopolamine in mice. Eur J Pharmacol. 2015; 760:88–95. PMID:
25912802.
62. Cho BJ, Kim M, Song YO. Effects of root of Taraxacum coreanum Nakai on the inhibition of inflammation and oxidative stress induced by lipopolysaccharide in ICR Mice. J Korean Soc Food Sci Nutr. 2015; 44:1763–1770.
63. Kassubek R, Gorges M, Schocke M, Hagenston VA, Huss A, Ludolph AC, Kassubek J, Tumani H. GFAP in early multiple sclerosis: a biomarker for inflammation. Neurosci Lett. 2017; 657:166–170. PMID:
28802830.
64. Memudu AE, Adewumi AE. Alpha lipoic acid ameliorates scopolamine induced memory deficit and neurodegeneration in the cerebello-hippocampal cortex. Metab Brain Dis. 2021; 36:1729–1745. PMID:
34021876.
65. Konar A, Shah N, Singh R, Saxena N, Kaul SC, Wadhwa R, Thakur MK. Protective role of
Ashwagandha leaf extract and its component withanone on scopolamine-induced changes in the brain and brain-derived cells. PLoS One. 2011; 6:e27265. PMID:
22096544.
66. Pereira JB, Janelidze S, Smith R, Mattsson-Carlgren N, Palmqvist S, Teunissen CE, Zetterberg H, Stomrud E, Ashton NJ, Blennow K, et al. Plasma GFAP is an early marker of amyloid-β but not tau pathology in Alzheimer’s disease. Brain. 2021; 144:3505–3516. PMID:
34259835.
67. Oeckl P, Anderl-Straub S, Von Arnim CA, Baldeiras I, Diehl-Schmid J, Grimmer T, Halbgebauer S, Kort AM, Lima M, Marques TM, et al. Serum GFAP differentiates Alzheimer’s disease from frontotemporal dementia and predicts MCI-to-dementia conversion. J Neurol Neurosurg Psychiatry. 2022; 93:659–667.
68. Liu Q, Chen Y, Shen C, Xiao Y, Wang Y, Liu Z, Liu X. Chicoric acid supplementation prevents systemic inflammation-induced memory impairment and amyloidogenesis
via inhibition of NF-κB. FASEB J. 2017; 31:1494–1507. PMID:
28003341.
69. Naveed M, Hejazi V, Abbas M, Kamboh AA, Khan GJ, Shumzaid M, Ahmad F, Babazadeh D, FangFang X, Modarresi-Ghazani F, et al. Chlorogenic acid (CGA): a pharmacological review and call for further research. Biomed Pharmacother. 2018; 97:67–74. PMID:
29080460.
70. Kwon SH, Lee HK, Kim JA, Hong SI, Kim HC, Jo TH, Park YI, Lee CK, Kim YB, Lee SY, et al. Neuroprotective effects of chlorogenic acid on scopolamine-induced amnesia via anti-acetylcholinesterase and anti-oxidative activities in mice. Eur J Pharmacol. 2010; 649:210–217. PMID:
20854806.
71. Mohammad-Zadeh LF, Moses L, Gwaltney-Brant SM. Serotonin: a review. J Vet Pharmacol Ther. 2008; 31:187–199. PMID:
18471139.
72. Sakamura S, Terayama Y, Kawakatsu S, Ichihara A, Saito H. Conjugated serotonins and phenolic constituents in safflower seed (Carthamus tinctorius L.). Agric Biol Chem. 1980; 44:2951–2954.
73. He M, Park C, Shin Y, Kim J, Cho E.
N-feruloyl serotonin attenuates neuronal oxidative stress and apoptosis in Aβ
25–35-treated human neuroblastoma SH-SY5Y cells. Molecules. 2023; 28:1610. PMID:
36838597.
74. Kim DH, Moon YS, Park TS, Son JH. Serotonins of safflower seeds play a key role in anti-inflammatory effect in lipopolysaccharide-stimulated RAW 264.7 macrophages. J Plant Biotechnol. 2015; 42:364–369.
75. Jung ES, Kim SB, Kim MH, Shin SW, Lee JS, Park DH. Inhibitory effects of serotonin derivatives on adipogenesis. J Soc Cosmet Sci Korea. 2011; 37:171–176.
76. Carola C, Salazar A, Rakers C, Himbert F, Do QT, Bernard P, von Hagen J. A Cornflower extract containing N-feruloylserotonin reduces inflammation in human skin by neutralizing CCL17 and CCL22 and inhibiting COX-2 and 5-LOX. Mediators Inflamm. 2021; 2021:6652791. PMID:
34557056.
77. Han SJ, Lim MJ, Lee KM, Oh E, Shin YS, Kim S, Kim JS, Yun SP, Kang LJ. Safflower seed extract attenuates the development of osteoarthritis by blocking NF-κB signaling. Pharmaceuticals (Basel). 2021; 14:258. PMID:
33809253.
78. Gottlieb A, Keydar I, Epstein HT. Rodent brain growth stages: an analytical review. Biol Neonate. 1977; 32:166–176. PMID:
603801.
79. Chen VS, Morrison JP, Southwell MF, Foley JF, Bolon B, Elmore SA. Histology atlas of the developing prenatal and postnatal mouse central nervous system, with emphasis on prenatal days E7. 5 to E18. 5. Toxicol Pathol. 2017; 45:705–744. PMID:
28891434.
80. Ciceri G, Baggiolini A, Cho HS, Kshirsagar M, Benito-Kwiecinski S, Walsh RM, Aromolaran KA, Gonzalez-Hernandez AJ, Munguba H, Koo SY, et al. An epigenetic barrier sets the timing of human neuronal maturation. Nature. 2024; 626:881–890. PMID:
38297124.
81. Guo L, Xiong H, Kim JI, Wu YW, Lalchandani RR, Cui Y, Shu Y, Xu T, Ding JB. Dynamic rewiring of neural circuits in the motor cortex in mouse models of Parkinson’s disease. Nat Neurosci. 2015; 18:1299–1309. PMID:
26237365.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download