1. Jantzen da Silva Lucas A, Menegon de Oliveira L, da Rocha M, Prentice C. Edible insects: An alternative of nutritional, functional and bioactive compounds. Food Chem. 2020; 311:126022. PMID:
31869637.
2. Boehm E, Borzekowski D, Ververis E, Lohmann M, Böl GF. Communicating food risk-benefit assessments: edible insects as red meat replacers. Front Nutr. 2021; 8:749696. PMID:
34977112.
3. Saeb A, Grundmann SM, Gessner DK, Schuchardt S, Most E, Wen G, Eder K, Ringseis R. Feeding of cuticles from
Tenebrio molitor larvae modulates the gut microbiota and attenuates hepatic steatosis in obese Zucker rats. Food Funct. 2022; 13:1421–1436. PMID:
35048923.
4. Seo M, Goo TW, Chung MY, Baek M, Hwang JS, Kim MA, Yun EY.
Tenebrio molitor larvae inhibit adipogenesis through AMPK and MAPKs signaling in 3T3-L1 adipocytes and obesity in high-fat diet-induced obese mice. Int J Mol Sci. 2017; 18:518. PMID:
28264489.
5. Yu JM, Jang JY, Kim HJ, Cho YH, Kim D, Kwon O, Cho YJ, An BJ. Antioxidant capacity and Raw 264.7 macrophage anti-inflammatory effect of the Tenebrio molitor. Korean Journal of Food Preservation. 2016; 23:890–898.
6. Ahn EM, Myung NY, Jung HA, Kim SJ. The ameliorative effect of
Protaetia brevitarsis larvae in HFD-induced obese mice. Food Sci Biotechnol. 2019; 28:1177–1186. PMID:
31275718.
7. Park CE, Lee SO. Nrf2-mediated protective effect of protein hydrolysates from
Protaetia brevitarsis larvae against oxidative stress-induced hepatotoxicity. Food Sci Biotechnol. 2023; 32:1561–1571. PMID:
37637846.
8. Jang HY, Kim JM, Kim JS, Kim BS, Lee YR, Bae JS.
Protaetia brevitarsis extract attenuates RANKL-induced osteoclastogenesis by inhibiting the JNK/NF-κB/PLCγ2 signaling pathway. Nutrients. 2023; 15:3193. PMID:
37513611.
9. MacKichan ML, DeFranco AL. Role of ceramide in lipopolysaccharide (LPS)-induced signaling. LPS increases ceramide rather than acting as a structural homolog. J Biol Chem. 1999; 274:1767–1775. PMID:
9880559.
10. Xiang H, Jin S, Tan F, Xu Y, Lu Y, Wu T. Physiological functions and therapeutic applications of neutral sphingomyelinase and acid sphingomyelinase. Biomed Pharmacother. 2021; 139:111610. PMID:
33957567.
11. García-Ruiz C, Colell A, Marí M, Morales A, Calvo M, Enrich C, Fernández-Checa JC. Defective TNF-alpha-mediated hepatocellular apoptosis and liver damage in acidic sphingomyelinase knockout mice. J Clin Invest. 2003; 111:197–208. PMID:
12531875.
12. Fernandez A, Matias N, Fucho R, Ribas V, Von Montfort C, Nuño N, Baulies A, Martinez L, Tarrats N, Mari M, et al. ASMase is required for chronic alcohol induced hepatic endoplasmic reticulum stress and mitochondrial cholesterol loading. J Hepatol. 2013; 59:805–813. PMID:
23707365.
13. Lang PA, Schenck M, Nicolay JP, Becker JU, Kempe DS, Lupescu A, Koka S, Eisele K, Klarl BA, Rübben H, et al. Liver cell death and anemia in Wilson disease involve acid sphingomyelinase and ceramide. Nat Med. 2007; 13:164–170. PMID:
17259995.
14. Osawa Y, Seki E, Adachi M, Suetsugu A, Ito H, Moriwaki H, Seishima M, Nagaki M. Role of acid sphingomyelinase of Kupffer cells in cholestatic liver injury in mice. Hepatology. 2010; 51:237–245. PMID:
19821528.
15. Moles A, Tarrats N, Morales A, Domínguez M, Bataller R, Caballería J, García-Ruiz C, Fernández-Checa JC, Marí M. Acidic sphingomyelinase controls hepatic stellate cell activation and
in vivo liver fibrogenesis. Am J Pathol. 2010; 177:1214–1224. PMID:
20651240.
16. Mir IH, Thirunavukkarasu C. The relevance of acid sphingomyelinase as a potential target for therapeutic intervention in hepatic disorders: current scenario and anticipated trends. Arch Toxicol. 2023; 97:2069–2087. PMID:
37248308.
17. Thayyullathil F, Cheratta AR, Alakkal A, Subburayan K, Pallichankandy S, Hannun YA, Galadari S. Acid sphingomyelinase-dependent autophagic degradation of GPX4 is critical for the execution of ferroptosis. Cell Death Dis. 2021; 12:26. PMID:
33414455.
18. Du YX, Zhao YT, Sun YX, Xu AH. Acid sphingomyelinase mediates ferroptosis induced by high glucose via autophagic degradation of GPX4 in type 2 diabetic osteoporosis. Mol Med. 2023; 29:125. PMID:
37710183.
19. Xie Y, Hou W, Song X, Yu Y, Huang J, Sun X, Kang R, Tang D. Ferroptosis: process and function. Cell Death Differ. 2016; 23:369–379. PMID:
26794443.
20. Yang WS, Kim KJ, Gaschler MM, Patel M, Shchepinov MS, Stockwell BR. Peroxidation of polyunsaturated fatty acids by lipoxygenases drives ferroptosis. Proc Natl Acad Sci U S A. 2016; 113:E4966–E4975. PMID:
27506793.
21. Hwang D, Goo TW, Yun EY. In Vitro Protective Effect of Paste and Sauce Extract Made with Protaetia brevitarsis Larvae on HepG2 Cells Damaged by Ethanol. Insects. 2020; 11.
22. Ganguly K, Dutta SD, Jeong MS, Patel DK, Cho SJ, Lim KT. Naturally-derived protein extract from
Gryllus bimaculatus improves antioxidant properties and promotes osteogenic differentiation of hBMSCs. PLoS One. 2021; 16:e0249291. PMID:
34077422.
23. Navarro del Hierro J, Gutiérrez-Docio A, Otero P, Reglero G, Martin D. Characterization, antioxidant activity, and inhibitory effect on pancreatic lipase of extracts from the edible insects
Acheta domesticus and
Tenebrio molitor. Food Chem. 2020; 309:125742. PMID:
31704068.
24. Kim MH, Kim SJ, Kim SH, Park WJ, Han JS.
Gryllus bimaculatus-containing diets protect against dexamethasone-induced muscle atrophy, but not high-fat diet-induced obesity. Food Sci Nutr. 2023; 11:2787–2797. PMID:
37324877.
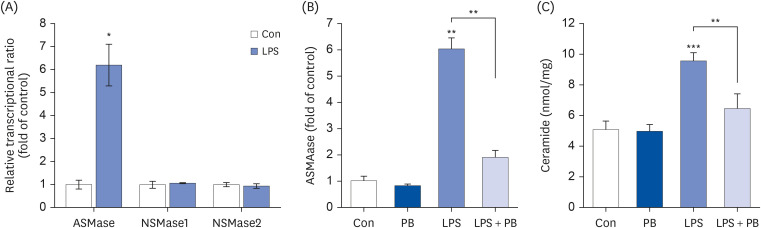
25. Kim MH, Park JW, Lee EJ, Kim S, Shin SH, Ahn JH, Jung Y, Park I, Park WJ. C16-ceramide and sphingosine 1-phosphate/S1PR2 have opposite effects on cell growth through mTOR signaling pathway regulation. Oncol Rep. 2018; 40:2977–2987. PMID:
30226616.
26. Choi RY, Kim IW, Ji M, Paik MJ, Ban EJ, Lee JH, Hwang JS, Kweon H, Seo M.
Protaetia brevitarsis seulensis larvae ethanol extract inhibits RANKL-stimulated osteoclastogenesis and ameliorates bone loss in ovariectomized mice. Biomed Pharmacother. 2023; 165:115112. PMID:
37413903.
27. Park YM, Noh EM, Lee HY, Shin DY, Lee YH, Kang YG, Na EJ, Kim JH, Yang HJ, Kim MJ, et al. Anti-diabetic effects of Protaetia brevitarsis in pancreatic islets and a murine diabetic model. Eur Rev Med Pharmacol Sci. 2021; 25:7508–7515. PMID:
34919253.
28. Zhao C, Xiao C, Feng S, Bai J. Artemisitene alters LPS-induced oxidative stress, inflammation and ferroptosis in liver through Nrf2/HO-1 and NF-kB pathway. Front Pharmacol. 2023; 14:1177542. PMID:
37180725.
29. Kim MH, Ahn HK, Lee EJ, Kim SJ, Kim YR, Park JW, Park WJ. Hepatic inflammatory cytokine production can be regulated by modulating sphingomyelinase and ceramide synthase 6. Int J Mol Med. 2017; 39:453–462. PMID:
28035360.
30. Yin L, Dai Y, Cui Z, Jiang X, Liu W, Han F, Lin A, Cao J, Liu J. The regulation of cellular apoptosis by the ROS-triggered PERK/EIF2α/chop pathway plays a vital role in bisphenol A-induced male reproductive toxicity. Toxicol Appl Pharmacol. 2017; 314:98–108. PMID:
27894913.
31. Sun J, Chen W, Li S, Yang S, Zhang Y, Hu X, Qiu H, Wu J, Xu S, Chu T. Nox4 promotes RANKL-induced autophagy and osteoclastogenesis via activating ROS/PERK/eIF-2α/ATF4 pathway. Front Pharmacol. 2021; 12:751845. PMID:
34650437.
32. Rodríguez-Hernández MA, Chapresto-Garzón R, Cadenas M, Navarro-Villarán E, Negrete M, Gómez-Bravo MA, Victor VM, Padillo FJ, Muntané J. Differential effectiveness of tyrosine kinase inhibitors in 2D/3D culture according to cell differentiation, p53 status and mitochondrial respiration in liver cancer cells. Cell Death Dis. 2020; 11:339. PMID:
32382022.
33. Jenkins RW, Canals D, Hannun YA. Roles and regulation of secretory and lysosomal acid sphingomyelinase. Cell Signal. 2009; 21:836–846. PMID:
19385042.
34. Insausti-Urkia N, Solsona-Vilarrasa E, Garcia-Ruiz C, Fernandez-Checa JC. Sphingomyelinases and liver diseases. Biomolecules. 2020; 10:1497. PMID:
33143193.
35. Oh E, Park WJ, Kim Y. Effects of Tenebrio molitor larvae and its protein derivatives on the antioxidant and anti-inflammatory capacities of tofu. Food Biosci. 2022; 50:102105.
36. Park WJ, Han JS.
Gryllus bimaculatus extract protects against lipopolysaccharide and palmitate-induced production of proinflammatory cytokines and inflammasome formation. Mol Med Rep. 2021; 23:206. PMID:
33495809.
37. Choi YJ, Bae IY. White-spotted flower chafer (Protaetia brevitarsis) ameliorates inflammatory responses in LPS-stimulated RAW 264.7 macrophages. J Insects Food Feed. 2023; 9:1037–1046.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download