INTRODUCTION
Hiatal hernia (HH) is the herniation of the abdominal organs through the diaphragmatic hiatus. This can be classified into 4 types. Type I, also known as sliding hernia, is an intrathoracic herniation of the gastroesophageal junction and is the most common type (90%–95%) [
1]. Types II–IV are paraesophageal hernias involving herniation of the stomach and abdominal viscera and are subclassified according to the degree of herniation [
2]. Symptoms are related to reflux but depend on the herniated organ and the level of hernia, ranging from gastroesophageal reflux disease (GERD) to pneumonia and strangulation of the herniated bowel. Surgery is the definitive treatment for HH. While both laparoscopic and open approaches are possible, the former is currently preferred [
34]. Surgical correction involves reducing the herniated bowel, excising the hernia sac, closing the crura, and performing anti-reflux procedures, such as fundoplication [
3].
Regarding the necessity of fundoplication for surgical correction of HH, the 2013 SAGES (Society of American Gastrointestinal and Endoscopic Surgeons) guidelines indicated that it is necessary for paraesophageal hernia [
5] but not for sliding hernia. Despite these recommendations, various opinions on its necessity have been presented recently. Solomon et al. [
6] reported that fundoplication did not reduce the recurrence rates of paraesophageal hernia compared with primary repair alone. Recent reports have indicated that the main finding in patients with recurrent HH is reherniation, characterized by a widening of the hiatus despite the presence of intact gastric wrapping [
78]. However, these guidelines are intended for adults, and there is no established consensus regarding HH repair in children due to lack of evidence. In a recent review by Garvey and Ostlie [
3], it was noted that there was only 1 report involving 20 South African patients, which suggested that anti-reflux surgery had a significant impact in reducing the recurrence of HH, with a decrease from 60% to 20%. Fundoplication is often recommended as a routine procedure in children, particularly for paraesophageal hernias. However, considering the unique characteristics of children who must maintain an oral diet, complications, such as postoperative esophageal passage disturbances, should be considered. Whether complete or partial fundoplication significantly reduces these complications has been debated. To date, no assessment of this necessity has been established.
Therefore, in this study we explored our 16-year experience with HH and evaluated outcomes and factors associated with them. In this process, we aimed to reassess the surgical management of HH in pediatric patients.
METHODS
We retrospectively reviewed the medical records of 49 patients who underwent HH repair between January 2006 and December 2021 at Asan Medical Center in Seoul, Korea. This study was approved by the Institutional Review Board of Asan Medical Center (No. 2022-0491) and informed consent was waived due to the retrospective nature of the study. The primary outcome of HH repair was evaluated based on symptoms, chest radiographs, and other imaging modalities (e.g., CT and fluoroscopic examination). Data regarding patient demographics, surgical procedures, and clinical outcomes were also collected. We compared the baseline patient characteristics and treatment outcomes between the groups. Following the adoption of the laparoscopic approach, in most cases, laparotomy was not conducted solely for the repair of HH. Laparotomy was selectively performed when conducted in conjunction with open surgery.
Surgical techniques
The patients were placed in the supine position, prepared, and draped in the usual manner. The surgeons chose between open and laparoscopic approaches. Three ports were used for laparoscopic repair. The left lateral segment of the liver was retracted to the anterolateral side by either tying the umbilical ligament to the anterior abdominal wall or by using a retractor through an additional port. The hiatus was exposed, and the hernia sac was resected. After reducing the hernia, the approximated crura were closed with 2 to three simple interrupted sutures using 4-0 or 3-0 ethylene terephthalate (Ethibond, Ethicon US, LLC) suture material. Both crura were repaired, and the distal esophagus was anchored to the crura at the level of the gastroesophageal junction using interrupted sutures.
Statistical analysis
Continuous values are presented as mean ± standard deviation or range unless otherwise stated. Categorical values are presented as frequencies and percentages. A P-value less than 0.05 was considered statistically significant. The effect of fundoplication on HH recurrence was evaluated using Kaplan-Meier analysis. IBM SPSS Statistics for Windows ver. 21 (IBM Corp.) was used for statistical analysis.
RESULTS
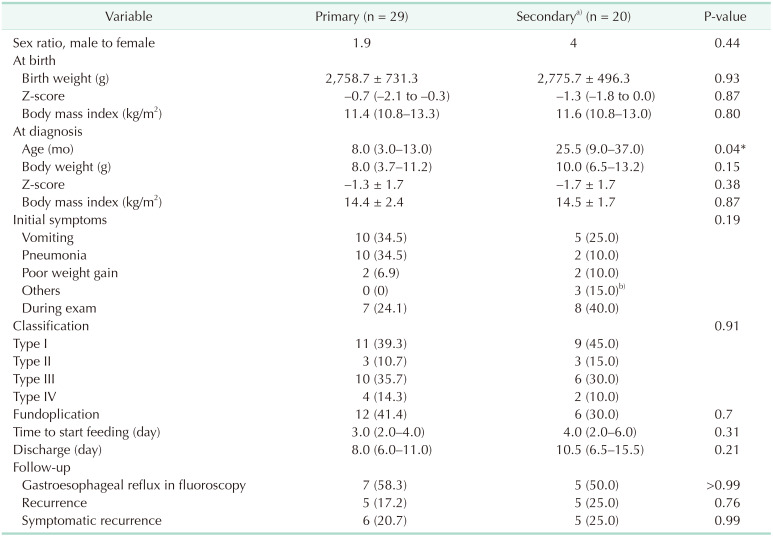
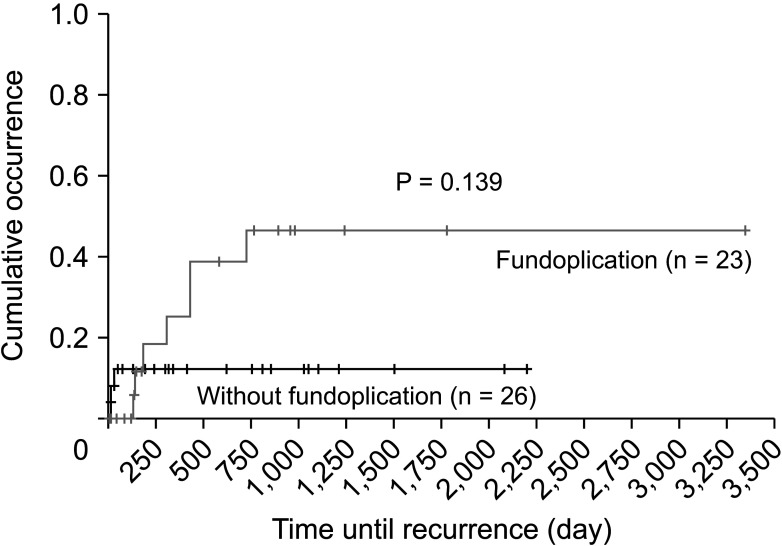
The median age of patients at diagnosis was 10.0 months (interquartile range [IQR], 5.0–27.0 months) (
Table 1). Fifty-nine percent of the patients had major diseases affecting the development of HH. Esophageal atresia (EA) was the most common (n = 11), followed by congenital diaphragmatic hernia (CDH; n = 9). In 41% of the children, HH occurred without any predisposing factors (
Table 2).
Table 1
Demographics of the patients
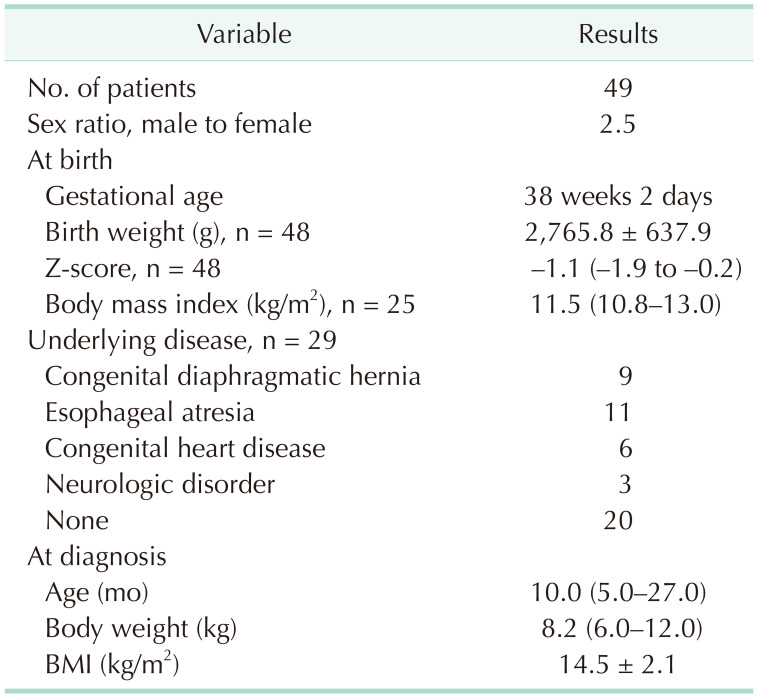

Table 2
Disease characteristics of patients
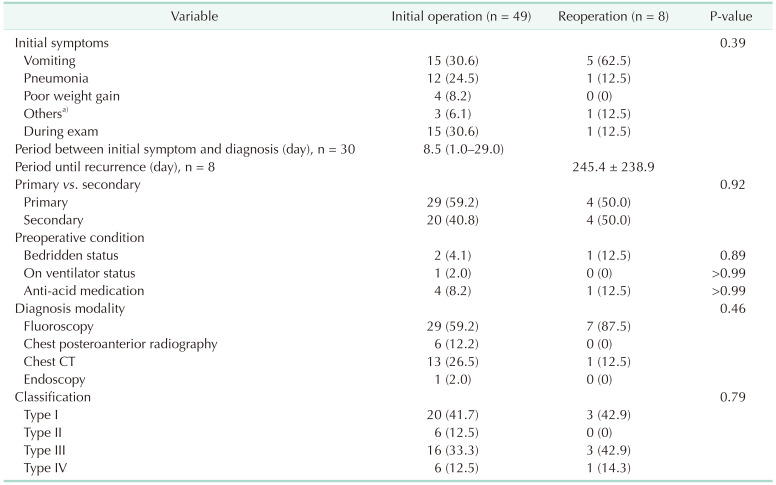

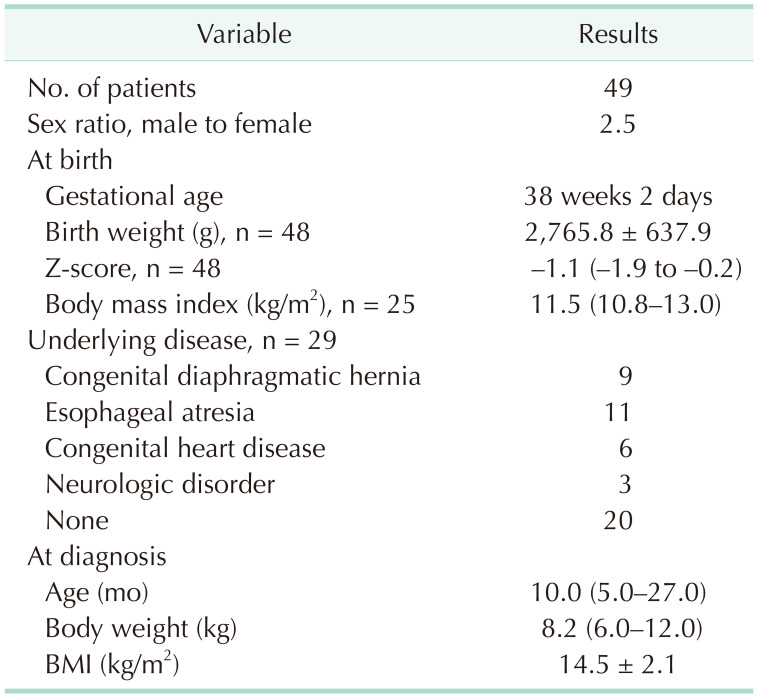
HH recurred in 10 children (20.4%), and reoperation was performed in 8 of them. We compared and analyzed the characteristics of patients who underwent surgery for initial (n = 49) and recurrent (n = 8) HHs (
Table 3). In 70% of the children, the first diagnosis of HH was made due to vomiting, pneumonia, and poor weight gain, whereas in the remaining 30%, it was incidentally found during examinations for other diseases. Recurrent HH was most commonly detected in cases of vomiting (62.5%). Sixty percent of HHs occurred spontaneously, and 40% occurred in relation to other medical conditions. Only 3 children had medical conditions that could cause HH, such as bedridden status. The diagnostic modalities varied; fluoroscopy was the most widely used, but in some cases, the diagnosis was confirmed by chest radiography. Sliding hernias accounted for approximately 40% of both primary and recurrent HHs. During the initial diagnosis, type IV HH was found in 6 patients (12.5%). However, there was no statistically significant difference between the number of initial and recurrent hernias. Two patients with recurrent hernias who opted for conservative treatment showed no definitive symptoms.
Table 3
Operation-related data
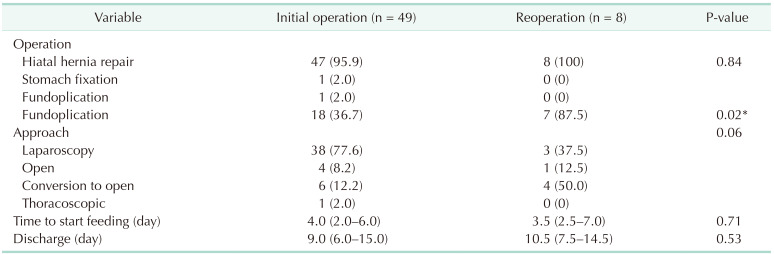

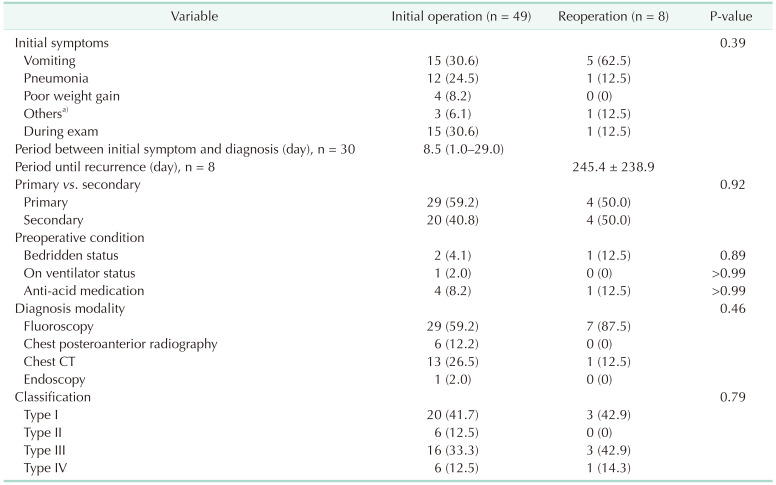
Fundoplication was performed in 18 patients (36.7%) during initial HH repair and in 7 (87.5%) during repeat HH repair (
Table 3). Fundoplication was performed in most children, regardless of the etiology, in recurrent cases. In 2 patients who were initially diagnosed with HH, stomach fixation was performed in 1 patient due to previous fundoplication, and fundoplication alone was performed in the other patient who had a history of stomach pull-up for EA. There were no significant differences between the surgical approaches and short-term outcomes.
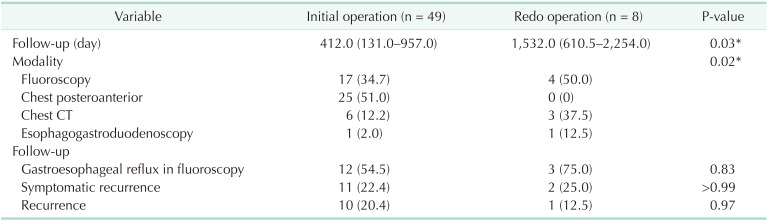
Median follow-up duration was longer in children with relapsed HH (412.0 days [IQR, 131.0–957.0 days]
vs. 1,532.0 days [IQR, 610.5–2,254.0 days]). Follow-up modalities varied, with fluoroscopy being performed more frequently in children with relapse (
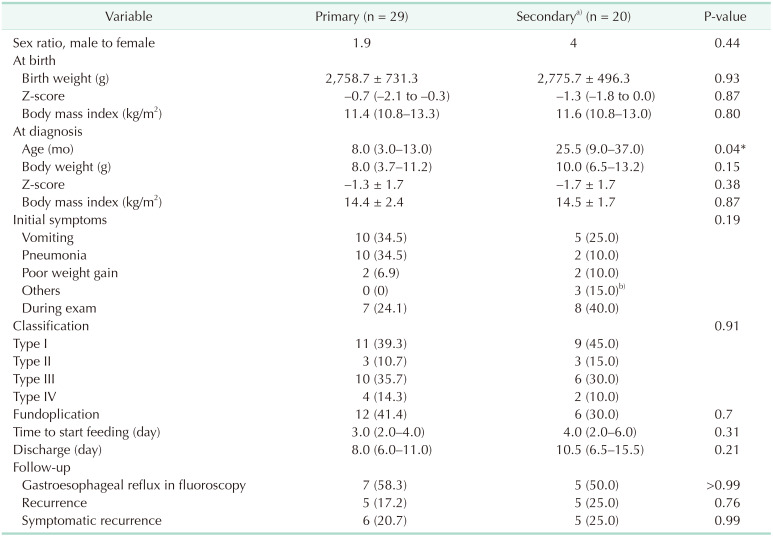
Table 4). Reflux on fluoroscopy was detected in 12 patients, reflux symptoms manifested in 11 patients, and anatomical recurrence in 10 patients. A similar trend was observed in patients who experienced relapse. There was no difference in etiology and clinical outcomes between primary and secondary HH patients (
Table 5).
Table 4
Surgical outcome of patients in initial operation and redo operation
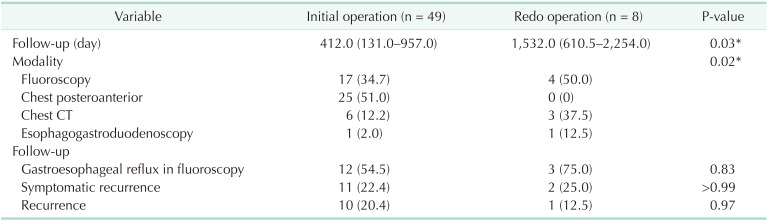

Table 5
Comparison between primary hiatal hernia and secondary hiatal hernia

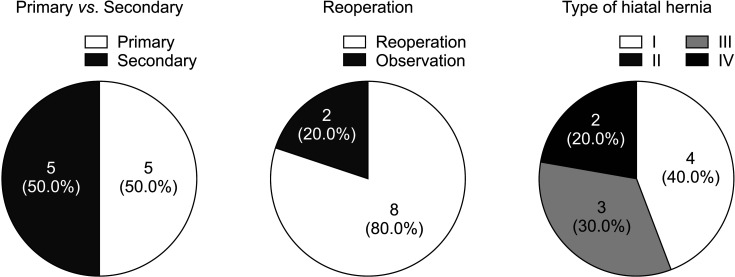
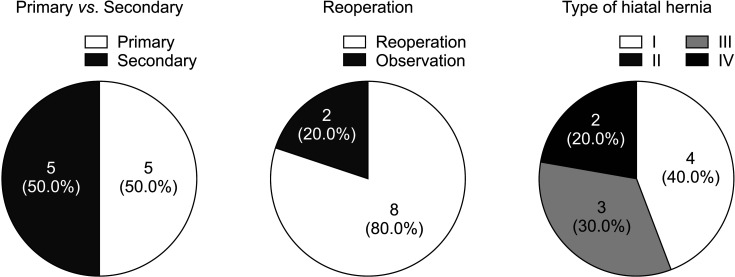
Additionally, we analyzed 10 cases of recurrence (
Fig. 1). Half of the patients experienced recurrence without any predisposing factors. Two children were followed up without repeat surgery because they were asymptomatic.
Fig. 1
Recurrence of hiatal hernia after repair (n = 10). Characteristics of patients with recurred hiatal hernia. (A) The number of patients with primary and secondary hiatal hernia was equal. (B) Reoperation was done in 8 patients (80.0%). (C) In 9 patients, the type of hiatal hernia was clarified. Four patients had type I and 3 patients were with type III. Two patients were diagnosed with type IV hiatal hernia.

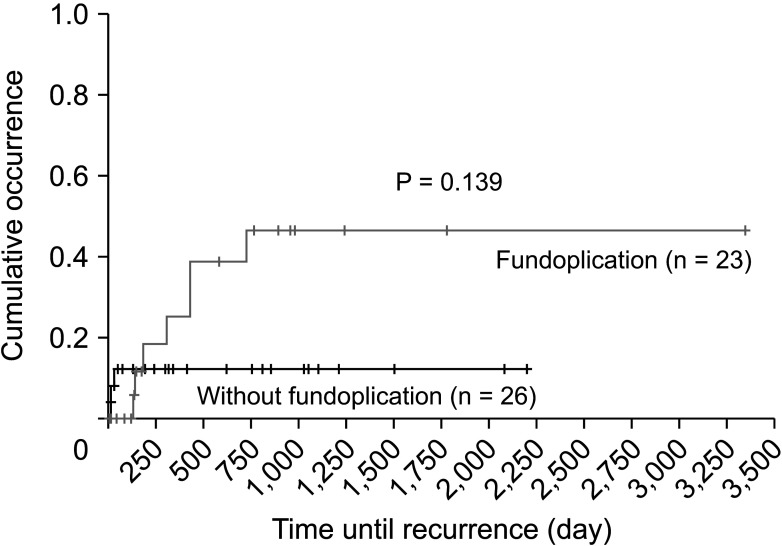
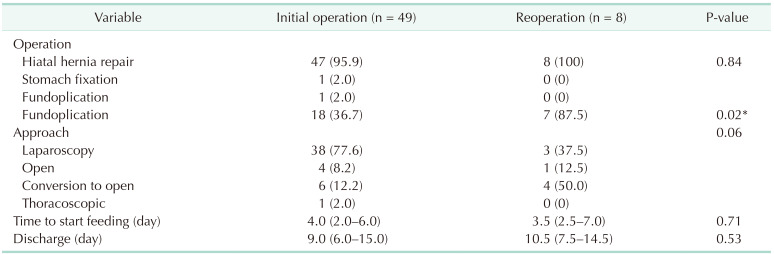
The effect of fundoplication on HH repair was also evaluated. Recurrence was detected in 3 children who underwent fundoplication (11%) and 7 children who did not (30%). There was no significant difference in reflux detected by fluoroscopy after HH repair between the patients who underwent fundoplication and those who did not. Kaplan-Meier analysis showed no statistically significant difference in recurrence-free survival (P = 0.139,
Fig. 2). Birth weight, body mass index (BMI) on the day of surgery, HH type, the existence of reflux before surgery, and surgical approach, including fundoplication, were not significantly associated with HH recurrence in the Cox regression analysis. Known predisposing factors such as CDH and EA had no significant effect on the occurrence and course of the disease (
Supplementary Tables 1,
2).
Fig. 2
The effect of fundoplication in recurrence-free survival. No statistically significant difference was observed between patients who got fundoplication and those who didn’t in recurrence-free survival in Kaplan-Meier analysis (P = 0.139). This finding suggests that fundoplication didn’t show preventive effect on hiatal hernia recurrence.

DISCUSSION
HH was first reported by Henry Bowditch in 1853 [
1]. Although its etiology remains unknown, several embryological hypotheses explain the development of congenital HH. Some contributing factors include retained right pneumoenteric recesses during development, laxity of gastric attachments, diaphragmatic hiatus deficiency, and abnormal development of the lumbar component of the diaphragm. The anatomical anti-reflux barrier, composed of the lower esophageal sphincter, crural diaphragm, angle of His, and gastroesophageal flap valve, is disrupted in patients with HH, especially paraesophageal hernia [
6]. Thus, trauma and dissection around the esophagus during prior surgery, such as fundoplication, may induce acquired HH.
We classified patients according to factors that could affect the anatomy and physiology of the hiatus (e.g., CDH, EA, congenital heart disease, and neurological disorders) as having secondary HH (n = 29, 59.2%) and compared them with patients with primary HH without a specific cause. Son et al. [
9] demonstrated that the incidence of HH increased in EA. No significant differences in patient characteristics, clinical manifestations, or clinical outcomes were observed between the 2 groups. We further found that each disease affecting the occurrence of HH, CDH (n = 9) and EA (n = 11), had no significant effect on the manifestation and outcome of HH. Therefore, our results showed that while diseases causing changes in the hiatus contributed to the increased prevalence of HH, there was no significant difference in the onset pattern or course compared to primary HH. This means that regardless of the presence or absence of an underlying disease that affects the onset, the same surgical treatment principles may be equally effective.
The clinical manifestations of HH varied widely between patients. Patients may exhibit symptoms ranging from being asymptomatic to gastrointestinal symptoms, respiratory distress, and failure to thrive. Symptoms related to GERD were observed in more than half of the patients. Surgical correction is the definitive treatment for this condition. Indications for surgery have not yet been clearly described; however, surgery is mostly performed when there are complications due to reflux. In our patients, vomiting, pneumonia, and poor weight gain were the major indications for surgery. Surgery included hiatal reconstruction and an anti-reflux procedure. Complete dissection of hiatus and reduction of herniated organs, sac removal whenever a sac exists (type II–IV), and repair of the hiatus are critical for preventing recurrence. When a child has an HH with reflux symptoms, fundoplication should be carefully selected by considering the possibility of complications such as dysphagia.
In their review article, which analyzed 4 papers evaluating the postoperative quality of life of patients who underwent fundoplication for GERD, Pilli et al. [
10] reported that fundoplication improved the quality of life, but most of the patients had underlying diseases, compelling them to undergo gastrostomy. Solomon et al. [
6] reviewed 9 articles and reported that fundoplication did not reduce the recurrence rate of HH compared to primary repair alone. They asserted that tailored fundoplication, based on appropriate preoperative assessment including manometry to exclude possible esophageal motility disorders, could prevent complications such as dysphagia and bloating [
11]. In addition, the surgical method of fundoplication should be considered [
1213]. This is important because healthy children without underlying diseases require a diet for growth after surgery; however, complications, such as dysphagia or bloating, may impede this. Mauritz et al. [
14] reported that severe dysphagia requiring endoscopic dilatation was more common in patients who underwent complete (Nissen) fundoplication (17%) based on a meta-analysis of 8 papers on fundoplication for GERD in pediatric patients.
To determine which factors affected the recurrence of HH in our patients, we compared patients with first-onset and relapsed HH. There were no significant differences in the patient or HH characteristics between the initial and relapsed HH groups. Armijo et al [
15]. reported that hernia recurrence is only related to the size of the hernial defect. Nguyen et al. [
16] asserted that cruroplasty is enough for redoing HH repair. However, in this study, we could not determine this relationship because data regarding the size of the HH were not available in the preoperative evaluation or surgical records. For paraesophageal hernias, these factors did not appear to affect the recurrence. Surgeons appear to be more prone to performing fundoplication in recurrent cases. Unexpectedly, the number of patients who had previously undergone fundoplication was higher than that of the relapsed patients. Therefore, we assumed that fundoplication itself did not affect HH recurrence. These findings indicate that there is potential for reconsidering the necessity of fundoplication in the surgical repair of HH in preventing recurrence in children. Additionally, birth weight, BMI on the day of the operation, HH type, presence of reflux before surgery, and surgical approach, including fundoplication, did not affect HH recurrence (Cox regression analysis, P < 0.05). To confirm the level of HH recurrence according to whether fundoplication was performed, we conducted a Kaplan-Meier analysis and found that fundoplication did not have a significant effect on recurrence (P = 0.140). We found similar results for the recurrence of reflux symptoms.
When analyzing 10 relapsed patients, including 2 patients who had relapse but did not undergo surgery, the number of patients with and without underlying diseases was the same. Of the 9 patients with confirmed types, 4 had sliding hernias and 5 had paraesophageal hernias, all of which were more severe than type III hernias. There was no significant difference in the clinical course between first-time and recurrent hernias; however, a longer follow-up period is necessary to clarify its clinical course in patients with recurrence.
The lack of statistical significance due to the small number of children is a limitation of this study. This is due to the rarity of the disease itself, and multicenter studies may help overcome this limitation. In addition, the analysis of the factors contributing to the progression of HH in children has been insufficient because of a lack of existing studies. Our study only provided limited information on HH, highlighting the need for further comprehensive analysis through follow-up studies.
As Pilli et al. [
10] have noted, fundoplication may be considered crucial and beneficial for individuals with neurological disabilities who are expected to face a long-term inability to orally consume food and are consequently undergoing gastrostomy tube placement. In the context of these patients, should muscle weakness progressively worsen over an extended duration, leading to hiatal laxity and a less toned stomach, there exists a risk of gradual reflux occurring solely because of the pressure exerted by the stomach during feeding. Additionally, there is an elevated risk of HH recurrence in this population. Additionally, it is believed that further benefits may accrue to patients who experience recurrent increases in abdominal tension due to general stiffness and seizures. Prophylactic fundoplication is considered effective not only in mitigating reflux in such patients but also in averting herniation for a certain period if hiatal laxity ensues due to decreased tone in the crus muscle. It's worth noting that concerns related to bloating and feeding challenges, which were subjects of interest in this study, are unlikely to pose significant issues. This is primarily due to the fact that feeding and drainage through the gastrostomy tube remain feasible and effective solutions. Nevertheless, when it comes to patients who do not necessitate gastrostomy feeding as they undergo growth and development, drawing upon the current literature review and the findings of this study, it can be deduced that fundoplication alone does not exert a substantial influence on the clinical progression of these patients.
In conclusion, our experience demonstrated that the surgical plan for HH repair is not affected by the presence or absence of an underlying disease or the occurrence of recurrence. Furthermore, it indicates the necessity to reassess the requirement for fundoplication in the treatment of HH.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download