Abstract
Purpose
Specialty choice in residency training has a significant impact on an individual’s career and satisfaction, as well as the supply-demand imbalance in the healthcare system. The current study aimed to investigate the quality of life (QOL), stress, self-confidence, and job satisfaction of residents, and to explore factors associated with such variables, including postgraduate year, sex, and especially specialty, through a cross-sectional survey.
Methods
An online survey was administered to residents at 2 affiliated teaching hospitals. The survey had a total of 46 items encompassing overall residency life such as workload, QOL, stress, confidence, relationship, harassment, and satisfaction. Related survey items were then reconstructed into 4 key categories through exploratory factor analysis for comparison according to group classification.
Results
The weekly work hours of residents in vital and other specialties were similar, but residents in vital specialties had significantly more on-call days per month. Residents in vital specialties had significantly lower scores for QOL and satisfaction. Specifically, vital-surgical residents had significantly lower QOL scores and higher stress scores than the other specialty groups. Satisfaction scores were also lowest among vital-surgical residents, with a marginal difference from vital-medical, and a significant difference from other-surgical residents. Female residents had significantly lower satisfaction scores than their male counterparts.
The period between the ages of 28 and 33 years, commonly known as the ‘age 30 transition,’ is crucial for achieving early adulthood goals such as pursuing aspirations, establishing a niche in society, and raising a family [1]. Residency training creates barriers to satisfactory progress through this stage. A survey conducted by the Korean Intern Resident Association (KIRA) in 2022 found that 54.3% of Korean medical residents reported perceived stress, which was more than twice that of the general population, and 17.4% of them experienced suicidal ideation [2]. Distress symptoms are more prevalent in trainees than in practicing surgeons [34]. The prevalence of burnout among medical students, residents, and practicing physicians in the United States exceeds 50% [5].
Although the duty hour restriction law has been in effect since December 2016, the results of a 2022 survey conducted by KIRA revealed that 52% of Korean residents still work over 80 hours per week. The survey also highlighted discrepancies between specialties, with more than 70% of residents in cardiothoracic surgery, surgery, orthopedic surgery, and neurosurgery reporting working ≥24 hours continuously at least once a week. Workload and lifestyle are significant factors that influence choosing or abandoning a medical specialty [2678910].
In 2023, certain specialties in Korea such as pediatrics, surgery, obstetrics-gynecology (OB-GYN), and cardiothoracic surgery failed to fill their resident quotas. The average attrition rate for the past 5 years was over 10% for certain specialties such as internal medicine, surgery, OB-GYN, pediatrics, as well as cardiothoracic surgery, neurosurgery, and urology. According to a 2017 report by the Korean Research Institute for Healthcare Policy (RIHP), residents identified inadequate compensation due to low reimbursement (52.9%) and poor working conditions (17.5%) as the 2 most important factors for avoiding certain specialties. Furthermore, 48.1% of those contemplating abandoning residency training cited heavy workload as the primary reason [8]. Specialty choice not only affects an individual’s career and satisfaction but also contributes to the supply-demand imbalance in the healthcare system [7]. Inadequate recruitment and unexpected attrition would further hamper the quality of training and the lives of the remaining residents. Depression and burnout among healthcare professionals, including residents, have been linked to decreased professionalism, increased medical errors, poorer patient outcomes, and worse hospital economics [11121314].
Few recent studies have reported significant concerns regarding perceived quality of life (QOL) or stress during residency in Korea. The current study aimed to (1) investigate the perceived QOL, physical/mental stress, clinical self-confidence, and overall job satisfaction of residents, and (2) explore possible factors related to such variables including postgraduate year (PGY), sex, and particularly specialty (departments). There have been previous studies on residents’ QOL, stress, and burnout, but most of them either did not compare across specialties or were limited to specific specialties [111213141516]. Identifying differences between specialties in areas such as perceived QOL, stress, and job-related satisfaction would help identify factors contributing to such differences and prioritize support.
This study protocol was approved by the Institutional Review Boards of Asan Medical Center and Gangneung Asan Hospital where the study was conducted (No. AMC 2022-1278 and GNAH 2022-10-001-001). This study adhered to the ethical guidelines of the World Medical Association’s Declaration of Helsinki. Informed consent was obtained from all subjects at the time of enrollment.
In September 2022, an online survey was conducted to collect data from current residents at Asan Medical Center and Gangneung Asan Hospital, which were affiliated under the same foundation and partially shared residents’ rotation schedules. To initiate the survey, a letter of cooperation and information about the study was sent to all working residents along with an online survey link via a multimedia messaging system. The survey was conducted anonymously using Google Forms for a period of 1 month. Prior to beginning the survey, participants were required to provide informed consent indicating their willingness to volunteer.
In designing our survey, we referred to previous studies [31718] to cover a wide range of topics in a descriptive manner, rather than using a limited set of highly detailed gold-standard measures. Therefore, we adapted our dataset by modifying and simplifying the referenced surveys to align with our specific requirements. The survey encompassed a total of 46 items, including demographic information (PGY, sex, specialty), workload (weekly work hours and monthly on-call days), as well as inquiries regarding overall residency life such as perceived QOL, stress, confidence in practice, relationship, harassment, and satisfaction. We conducted a pilot test with a cohort of 8 residents and incorporated their feedback to eliminate the open-ended questions and to use a uniform 10-point Likert scale ranging from 0 (not at all) to 9 (very positive/very confident) for the convenience of response. The completion time for the survey averaged approximately fifteen minutes. To assess self-reported confidence in clinical practice, the survey included questions on various tasks representing clinical, procedural, and communication skills, adapted from a previous study [18]. The term “stress” was not formally defined in the questionnaire to capture individual perceptions, as these experiences may vary among individuals [317]. Job satisfaction was assessed by items related to satisfaction with the specialty, and satisfaction with the medical profession as a physician. To minimize response bias, the survey included a mix of positive and negative items. All survey questions are listed in Supplementary Material 1.
We first grouped the residents by PGY, sex, and specialty. Regarding specialty, although specialties in clinical medicine can be broadly categorized as medical, surgical, and clinical support departments [1920], we first classified them as “vital” and “others (other than vital).” Internal medicine, surgery, pediatrics, and OB-GYN were arbitrarily designated as “vital” specialties, while all other specialties were grouped as “other” specialties for terminological convenience. We then further subdivided the specialties into “surgical” and “medical (other than surgical)” within the vital and other specialties, respectively. Notably, among our “other-surgical” respondents (residents with surgical specialties outside of surgery and OB-GYN), there were no cardiothoracic surgery residents and only one each in neurosurgery and urology, while plastic surgery, otolaryngology, and orthopedic surgery residents accounted for 25 of 31 respondents (80.6%). Of note, our preliminary analysis categorizing the specialties as medical, surgical, and clinical support yielded only 2 significant results: the QOL score of the clinical support specialty was higher than that of the surgical specialty, and the self-confidence score of the clinical support specialty was lower than that of the medical or surgical specialties (Supplementary Table 1). We assumed that these results might be due to the fact that “medical” or “surgical” specialties are a mixture of different specialties with different workloads, and thus revised our specialty classification accordingly.
In the second step, we assessed the reliability and validity of the 41 items in the questionnaire (excluding demographics and workload) using a Cronbach alpha reliability coefficient of 0.822. Subsequently, we conducted a principal component analysis and employed the Varimax rotation method to explore the underlying structure that explains the patterns of correlation among the survey variables and to enhance the interpretability of the factors. Then the 41 items were divided into 7 categories and reduced to 34 items (60% explanatory power). We carefully selected 4 key categories among them that we consider to be highly pertinent to the topic under investigation (Supplementary Table 2); QOL, stress, confidence, and satisfaction. The 4 key categories analyzed in this study consisted of a total of 22 items and had a Cronbach alpha of 0.715. The reliability expressed as Cronbach alpha for each category was as follows: confidence (0.928), QOL (0.890), stress (0.782), and satisfaction (0.743). Finally, 2 items representing perceived workload (weekly work hours and monthly on-call days) and the 4 key categories that intuitively represent the hospital life of residents were analyzed according to group classification.
The statistical analysis methods used to verify reliability and validity were Cronbach alpha and factor analysis. Descriptive statistics, t-test, analysis of variance, and one-way univariate general linear model were used to analyze differences between the groups (PGY, sex, and specialty). Data were analyzed using IBM SPSS Statistics ver. 27 for Windows (IBM Corp.). A P-value of 0.05 was chosen as the statistical significance threshold.
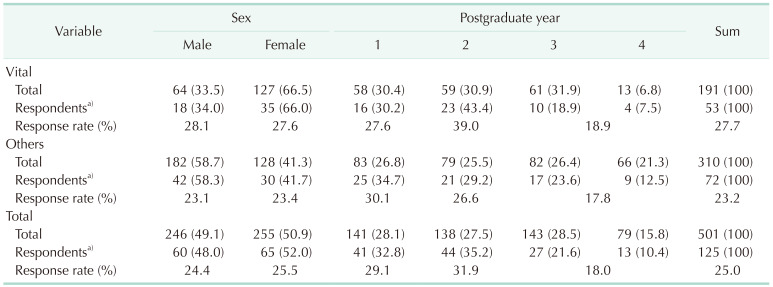
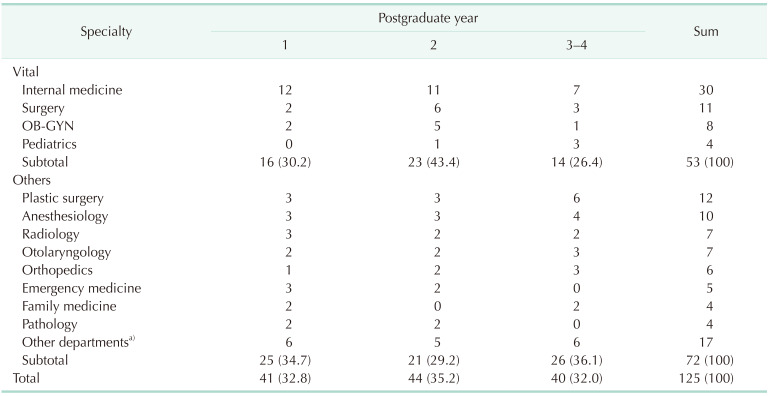
Of the 501 total eligible participants, 125 completed the survey, with a response rate of 25.0%. There was no significant difference in the response rate between vital and other specialties (27.7% vs. 23.2%, P = 0.264). There was no difference in the distribution of PGY between respondents in the vital and other specialties (P = 0.721), but 66% of respondents in the vital specialties, as opposed to 41.7% of respondents in the other specialties, were female; a significantly higher proportion (P = 0.006) (Table 1). All respondents’ specialties are summarized in Table 2.
The survey consisted of a total of 43 questions (excluding demographics) covering perceived workload (weekly work hours and monthly on-call days) and overall residency life including perceived QOL, stress, confidence in practice, relationship, harassment, and satisfaction (Supplementary Material). The mean (±standard deviation) weekly work hours were 78.34 (±17.93) hours, and the average on-call days per month was 6.26 (±3.67) days.
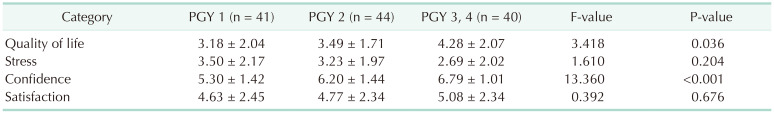
The comparison of weekly work hours between PGY 1, 2, and 3–4 residents showed no significant difference (81.71 ± 17.20, 78.93 ± 17.48, and 74.31 ± 18.79 hours for PGY 1, 2, and 3–4, respectively; P = 0.176). However, the mean number of on-call days per month differed significantly (7.23 ± 4.53, 6.42 ± 2.89, and 5.03 ± 3.20 days for PGY 1, 2, and 3–4, respectively; P = 0.024). Specifically, there were significant differences between PGY 1 vs. PGY 3–4 (P = 0.007) and PGY 2 vs. PGY 3–4 (P = 0.019), but no significant difference between PGY 1 and 2 (P = 0.170). In terms of the key category scores, QOL score increased with increasing years of training, with statistically significant differences between PGY 1 and PGY 3–4. Similarly, confidence scores also increased with PGY level, with significant differences between PGY 1 vs. PGY 2 and between PGY 1 vs. PGY 3–4 (Table 3).
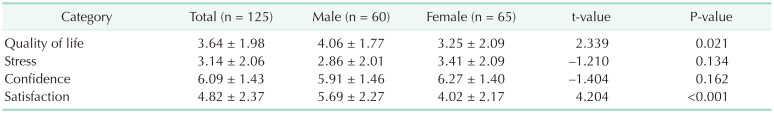
The analysis did not reveal any significant differences in work hours or on-call days between male and female residents. However, the key category analysis showed that female residents had significantly lower scores for QOL and satisfaction. No significant sex differences were found in stress or confidence scores (Table 4).
We performed a subgroup analysis to determine whether the significant sex differences observed were influenced by differences in the sex distribution between vital and other specialties. Within the vital subgroup, female residents had significantly lower satisfaction scores than their male counterparts (3.48 vs. 5.24, P = 0.011). A similar trend was observed within the other specialty subgroups, albeit to a lesser extent (4.66 vs. 5.88, P = 0.016). However, there were no significant sex differences in the other categories for either subgroup (Supplementary Table 3).
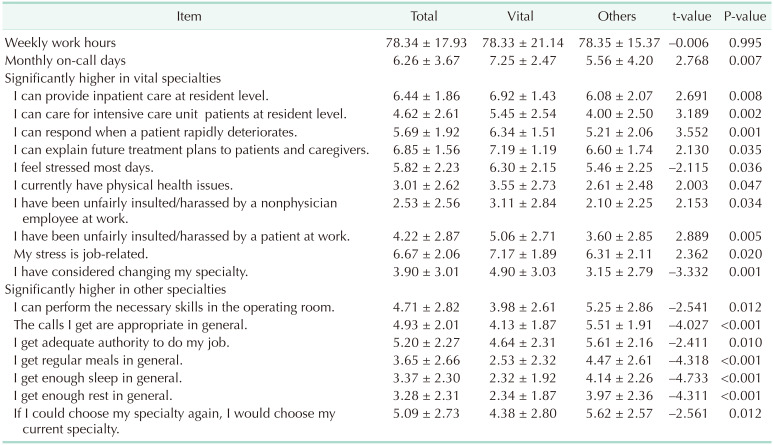
The weekly work hours of residents in vital and other specialties were similar, with a mean of 78.33 (±21.14) hours and 78.35 (±15.37) hours, respectively (P = 0.995). However, there was a significant difference in their monthly on-call days, with residents in vital specialties having an average of 7.25 (±2.47) days compared to 5.56 (±4.20) days for those in other specialties (P = 0.007). Table 5 highlights other significant differences in the survey results.
Residents in vital specialties reported lower scores for regular meals (2.53 vs. 4.47 in other specialties, P < 0.001), adequate sleep (2.32 vs. 4.14, P < 0.001), and enough rest (2.34 vs. 3.97, P < 0.001). They also reported higher scores on the question, “I feel stressed most days.” (6.30 vs. 5.46, P = 0.036), with work-related stress being the most significant factor (7.17 vs. 6.31, P = 0.020). In terms of job performance, residents in vital specialties reported lower scores for receiving appropriate calls (4.13 vs. 5.51, P < 0.001) and having appropriate authority (4.64 vs. 5.61, P = 0.017). The score for considering specialty change was also higher for residents in vital specialties, with a mean score of 4.90 vs. 3.15 for residents in other specialties (P = 0.001) on a 10-point Likert scale.
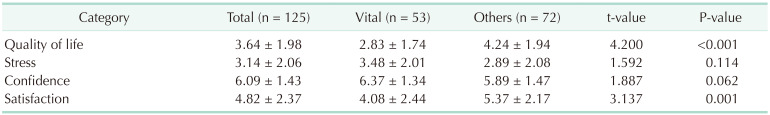
Category analysis revealed that residents in vital specialties had significantly lower scores for QOL and satisfaction than residents in other specialties. Although stress tended to be higher in the vital specialties, and confidence tended to be higher as well, these differences were not significant (Table 6).
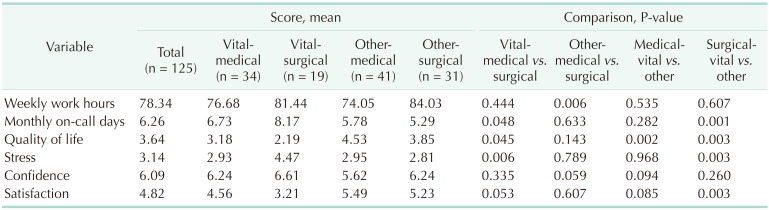
When we further divided the specialties into medical (nonsurgical) and surgical subdivisions within vital or other specialties, comparisons were made between (1) vital-medical vs. vital-surgical, (2) other-medical vs. other-surgical, (3) vital-medical vs. other-medical, and (4) vital-surgical vs. other-surgical. With regard to workload, the mean work hours per week was significantly higher for other-surgical residents compared to other-medical residents (84.03 vs. 74.05, P = 0.006), and the mean number of on-call days per month was significantly higher for vital-surgical residents compared to vital-medical or other-surgical residents (8.17, 6.73, and 5.29, respectively).
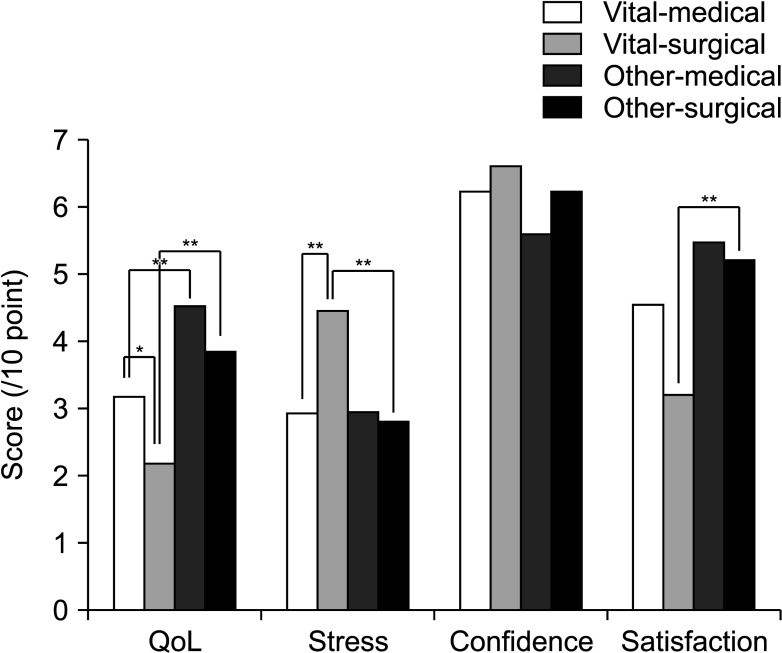
When it comes to the key category analysis, vital-surgical residents showed significantly worse QOL and higher stress than vital-medical or other-surgical residents. Vital-medical residents had significantly lower QOL score compared to other-medical residents. Satisfaction score was lowest in vital-surgical residents (3.21), showing a marginal difference with vital-medical (4.56, P = 0.053), and significant difference with other-surgical residents (5.23, P = 0.003). The highest satisfaction score was observed in the other-medical group (5.49) but the differences were not significant compared to vital-medical or other-surgical counterparts (no comparison was made with vital-surgical group) (Table 7, Fig. 1).
Medical students’ specialty choice is influenced by a number of factors. Traditionally, interests and preferences, personal traits, sociodemographic factors, and learning experiences are known to be important [7]. A change has taken place in recent decades among medical students to follow specialties that offer greater control over lifestyle, and the less flexible lifestyle of surgical specialties has become an important reason for viewing this field as less attractive [7910]. A 2013 Korean study found that income, lower workload, and intellectual stimulation were the most influential factors [21], while a 2017 Canadian study rated job satisfaction and lifestyle following training as the highest [6]. Avoidance of risk is another important factor. Ariely and Lanier [22] claimed that asymmetrical reward is one of the significant negative factors for physicians’ well-being, as they receive little or no reward or recognition for what they do while facing immense negative consequences for malpractices. Korean residents cited inadequate compensation and high risk as the main reasons for avoiding certain specialties [2]. As a result, specialties in medicine are a mixture of highly competitive and noncompetitive subspecialties, as the Careers in Medicine of Association of American Medical Colleges classified specialties into 3 different levels of competitiveness [23].
Residents’ overwhelming workload often results in sleep deprivation and unhealthy diets which are associated with stress and burnout [34]. A 2022 Korean study showed that objectively measured health indicators such as body mass index, blood pressure, and laboratory results worsened significantly during residency, particularly for surgical residents [19]. In the 2017 RIHP report, more than half of the surgical residents reported mealtimes of less than 20 minutes, compared with 19% of medical and clinical support department residents [8]. Our study found that residents in vital specialties reported significantly worse perceived QOL than residents in other specialties. Specifically, vital-surgical residents reported the lowest QOL score (2.19), which was significantly different from all other groups.
Residents in other-surgical specialties in this study worked mostly in less critical surgery departments such as plastic surgery, otolaryngology, and orthopedics whereas more than half of the residents in other-medical specialties worked in clinical support departments such as anesthesiology, radiology, emergency medicine, and pathology. Despite a difference of almost 10 hours in weekly work hours (84.03 vs. 74.05), perceived QOL, stress, and satisfaction scores were not significantly different between other-surgical and other-medical specialty groups. On the other hand, vital-surgical residents reported significantly lower QOL, higher stress, and lower satisfaction scores than vital-medical or other-surgical residents (except for a marginally significant difference in satisfaction compared with the vital-medical group, P = 0.053), even though there was no significant difference in perceived weekly work hours. These findings suggest that residents’ perceived QOL, stress, and job-related satisfaction are related to the intensity and urgency of their work rather than to total work hours.
When we examined job-related self-confidence, residents with vital specialties showed significantly higher scores on items involving ‘providing inpatient care,’ ‘caring for intensive care unit patient,’ and ‘responding to a rapidly deteriorating patient.’ These results indirectly demonstrate that they have more experience in these situations, which is to be expected. The higher confidence scores of our vital specialty residents, however, did not translate into higher satisfaction scores. This may be partly explained by their significantly lower scores on items related to working conditions such as ‘getting appropriate calls’ and ‘having adequate autonomy’ because greater well-being is achieved only when success in a task is controlled by one’s own motivation (autonomy).
According to Rodrigues et al. [24], residents in surgical/urgency specialties such as general surgery, anesthesiology, OB-GYN, and orthopedics have the highest prevalence of burnout syndrome, which is consistent with our findings for the specialty group of vital (or more specifically vital-surgical) specialty residents. A study of American general surgery residents found that 43% considered leaving their training due to overwhelming stress [1624]. According to the 2017 RIHP report, approximately 20% of Korean residents reported that they had considered changing or leaving their residency program [8]. Our survey asked respondents about their thoughts on changing specialty, choosing their current specialty again if given the chance, and becoming a doctor if reborn. These items were combined into the satisfaction category and showed a significant difference between vital and other specialties (4.08 vs. 5.37). This finding suggests the need for more active approaches to residents’ QOL and well-being, as well-being is more than the reduction or elimination of a pathological condition.
Job satisfaction should be approached qualitatively rather than through numerical restrictions on work hours since studies have shown that duty hour restrictions have improved residents’ satisfaction with their personal lives but not with their work [25]. In a study of Korean emergency medicine residents, work-related factor was actually found to be the lowest cause of occupational stress and the highest cause of occupational satisfaction. The highest cause of occupational stress was the environmental factor, with excessive demands from patients being the most common [15]. As our study did not address the specific causes of stress or satisfaction, further studies are needed to elucidate these factors. Qualitative studies of residents in specific specialties, such as focused group interviews, may yield meaningful results, as demonstrated in the study above. In addition, certain sociodemographic factors such as being young, female, and unmarried, and various extrinsic factors such as finances and interpersonal relationships have also been reported as common stressors among residents, although not being analyzed in the current study [1624]. The Happy Docs study in Canada found that career and financial counseling were the top 2 resources that residents would like to have available to them [17]. Providing support in these areas could also help improve residents’ work performance.
Sex issues deserve special attention. Several previous studies have found that female medical students tended to value a controllable lifestyle, lower workload, and reduced risk more than their male counterparts [21], though this differs from the findings of a study by Lambert and Holmboe [26]. In addition, female residents reported lower self-reported levels of confidence than male residents [18], although external evaluations did not show a significant difference [27]. These were attributed to differences in opportunity, experience, feedback, or sex imprinting [182829]. However, our results showed that the confidence scores of female residents tended to be higher, although not statistically significant. The proportion of female residents in Korea increased from 35.7% in 2017 to 38.1% in 2019, with an even faster increase of females in critical surgical specialties such as surgery, cardiothoracic surgery, and OB-GYN. As a result, the aforementioned sex differences in career choice motivation and self-confidence are now being challenged.
Stress and burnout among female residents are a real problem. Female physicians are reported to experience higher levels of perceived and occupational stress and are at higher risk for burnout than their male counterparts [2425]. Recently, a Korean study reported that female faculty members reported significantly higher emotional exhaustion and depersonalization [30]. Our study also found significantly lower QOL and satisfaction scores among female residents compared to male residents. It is notable that satisfaction score was significantly lower for female residents than their male counterparts when comparisons were made within either vital or other specialty subgroup.
The current study has several limitations. First, the study was conducted in only 2 teaching hospitals, which limits the generalizability to the entire population of more than 10,000 residents in Korea. Therefore, the results of this study cannot be applied to individual hospitals and can only be used as a guide to a certain trend. However, we believe that the homogeneity of the participating hospitals allowed for a reliable comparison across specialties and sexs. Second, the response rate was relatively low (25%) compared with other previous studies [31725], which may introduce selection bias and active participant bias. In addition, our data precluded analysis of whether respondents were representative of the overall population by specialty distribution. Specifically, there was a difference in the sex ratio of respondents between vital and other specialties, as well as a difference in the proportion of PGY, which may have contributed to the bias. Another limitation is that we used a questionnaire that lacks evidence of validity, unlike previous studies that used validated survey instruments [142425]. Therefore, the results of this study cannot be directly compared to existing studies and hardly be utilized as a longitudinal study. However, the primary aim of this study was to compare the results between subgroups within the respondents, and we prioritized understanding the perceived status of residents’ lives in broad aspects. Therefore, a customized questionnaire based on similar studies was developed and used [21920]. Finally, we did not investigate specific causal factors related to stress or satisfaction, nor did we assess the availability of resources or interventions to manage stress and burnout. We expect that future well-designed studies will investigate these factors in order to develop meaningful strategies to support residents and improve their well-being.
The current study clearly showed that residents in vital specialties, especially in vital-surgical specialties, experience significantly worse working conditions across multiple dimensions. It is therefore essential to improve not only the quantity but also the quality of the system in order to increase job satisfaction and prevent attrition. Special attention and support should be given to female residents whose numbers are rapidly increasing. We expect the findings to serve as a starting point for discussions about qualitative approaches in resident support as well as resource allocation and prioritization.
References
2. Korean Intern Resident Association (KIRA). Press release from the KIRA 20230126: KIRA, announcement of the 2022 major survey results [Internet]. KIRA;2023. cited 2023 May 15. Available from: http://youngmd.org/155/?idx=14000754&bmode=view
.
3. Cohen JS, Patten S. Well-being in residency training: a survey examining resident physician satisfaction both within and outside of residency training and mental health in Alberta. BMC Med Educ. 2005; 5:21. PMID: 15972100.

4. Raj KS. Well-being in residency: a systematic review. J Grad Med Educ. 2016; 8:674–684. PMID: 28018531.

5. Rothenberger DA. Physician burnout and well-being: a systematic review and framework for action. Dis Colon Rectum. 2017; 60:567–576. PMID: 28481850.

6. Vo A, McLean L, McInnes MD. Medical specialty preferences in early medical school training in Canada. Int J Med Educ. 2017; 8:400–407. PMID: 29140793.

7. Hohf-Nova M, Hun-Pacheco R, Muñoz-Bustos D, Soto-Carriel A, Pérez-Villalobos C. When it is time to decide: factors associated to the choice of a medical specialty. Rev Med Chil. 2021; 149:1352–1359. PMID: 35319690.

8. Research Institute for Healthcare Policy (RHIP), Korea Medical Association (KMA). Research Report: 2017 Survey on major training and working environments [Internet]. RHIP, KMA;2017. cited 2023 May 15. Available from: https://www.rihp.re.kr/bbs/board.php?bo_table=research_report&wr_id=264&sst=wr_datetime&sod=desc&sop=and&page=3
.
9. Schwartz RW, Haley JV, Williams C, Jarecky RK, Strodel WE, Young B, et al. The controllable lifestyle factor and students’ attitudes about specialty selection. Acad Med. 1990; 65:207–210. PMID: 2306321.

10. Dorsey ER, Jarjoura D, Rutecki GW. Influence of controllable lifestyle on recent trends in specialty choice by US medical students. JAMA. 2003; 290:1173–1178. PMID: 12952999.

11. Sobhonslidsuk A, Thakkinstian A, Satitpornkul P. Health-related quality of life and happiness within an internal medicine residency training program: a longitudinal follow-up study. J Educ Eval Health Prof. 2015; 12:3. PMID: 25748482.

12. Choi SM, Park YS, Yoo JH, Kim GY. Occupational stress and physical symptoms among family medicine residents. Korean J Fam Med. 2013; 34:49–57. PMID: 23372906.

13. Shiga T, Hifumi T, Hagiwara Y, Otani N, Tanaka H, Nakano M, et al. Career satisfaction among acute care resident physicians in Japan. Acute Med Surg. 2022; 9:e779. PMID: 36051448.

14. Lebares CC, Guvva EV, Ascher NL, O’Sullivan PS, Harris HW, Epel ES. Burnout and stress among us surgery residents: psychological distress and resilience. J Am Coll Surg. 2018; 226:80–90. PMID: 29107117.

15. Kim YG, Ryoo HW, Seo KS, Park JB, Chung JM, Kim JK, et al. Job stress, job satisfaction of emergency residents and its related factors. J Korean Soc Emerg Med. 2008; 19:749–759.
16. Ha GQ, Go JT, Murayama KM, Steinemann S. Identifying sources of stress across years of general surgery residency. Hawaii J Health Soc Welf. 2020; 79:75–81. PMID: 32190839.
17. Cohen JS, Leung Y, Fahey M, Hoyt L, Sinha R, Cailler L, et al. The happy docs study: a Canadian Association of Internes and Residents well-being survey examining resident physician health and satisfaction within and outside of residency training in Canada. BMC Res Notes. 2008; 1:105. PMID: 18957136.

18. Gavinski K, Cleveland E, Didwania AK, Feinglass JM, Sulistio MS. Relationship between confidence, gender, and career choice in internal medicine. J Gen Intern Med. 2021; 36:662–667. PMID: 32989713.

19. Ahn JS, Cho S, Park WJ. Changes in the health indicators of hospital medical residents during the four-year training period in Korea. J Korean Med Sci. 2022; 37:e202. PMID: 35762145.

20. Kwon OY, Park SY. Specialty choice preference of medical students according to personality traits by Five-Factor Model. Korean J Med Educ. 2016; 28:95–102. PMID: 26838573.

21. Lee CW. Gender difference and specialty preference in medical career choice. Korean J Med Educ. 2013; 25:15–21. PMID: 25804649.

22. Ariely D, Lanier WL. Disturbing trends in physician burnout and satisfaction with work-life balance: dealing with malady among the nation’s healers. Mayo Clin Proc. 2015; 90:1593–1596. PMID: 26653295.

23. Mitsouras K, Dong F, Safaoui MN, Helf SC. Student academic performance factors affecting matching into first-choice residency and competitive specialties. BMC Med Educ. 2019; 19:241. PMID: 31262294.

24. Rodrigues H, Cobucci R, Oliveira A, Cabral JV, Medeiros L, Gurgel K, et al. Burnout syndrome among medical residents: a systematic review and meta-analysis. PLoS One. 2018; 13:e0206840. PMID: 30418984.

25. Kassam A, Horton J, Shoimer I, Patten S. Predictors of well-being in resident physicians: a descriptive and psychometric study. J Grad Med Educ. 2015; 7:70–74. PMID: 26217426.

26. Lambert EM, Holmboe ES. The relationship between specialty choice and gender of U.S. medical students, 1990-2003. Acad Med. 2005; 80:797–802. PMID: 16123456.

27. Holmboe ES, Huot SJ, Brienza RS, Hawkins RE. The association of faculty and residents’ gender on faculty evaluations of internal medicine residents in 16 residencies. Acad Med. 2009; 84:381–384. PMID: 19240452.

28. Gong D, Winn BJ, Beal CJ, Blomquist PH, Chen RW, Culican SM, et al. Gender differences in case volume among ophthalmology residents. JAMA Ophthalmol. 2019; 137:1015–1020. PMID: 31318390.

29. Mueller AS, Jenkins TM, Osborne M, Dayal A, O’Connor DM, Arora VM. Gender differences in attending physicians’ feedback to residents: a qualitative analysis. J Grad Med Educ. 2017; 9:577–585. PMID: 29075375.

30. Seo JH, Bae HO, Kim BJ, Huh S, Ahn YJ, Jung SS, et al. Burnout of faculty members of medical schools in Korea. J Korean Med Sci. 2022; 37:e74. PMID: 35257529.

SUPPLEMENTARY MATERIALS
Supplementary Material 1 and Supplementary Tables 1–3 can be found via https://doi.org/10.4174/astr.2023.105.4.188.
Supplementary Table 1
Preliminary results comparing workload and scores between medical, surgical, and clinical support specialties
Supplementary Table 3
Comparison between male and female residents within either vital or other specialty group
Fig. 1
Key category scores comparison between residents’ specialty subgroups. Comparisons were made between (1) vital-medical vs. vital-surgical, (2) other-medical vs. other-surgical, (3) vital-medical vs. other-medical, and (4) vital-surgical vs. other-surgical specialties. QOL, quality of life. *P < 0.05, **P <0.01.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download