INTRODUCTION
The provision of comprehensive medical services with continuity is instrumental to quality healthcare services. However, under the current healthcare system, services are provided in a fragmented manner between different settings, such as acute care, subacute care, and community care services, far from a seamless integration among the areas of prevention, treatment, and rehabilitation. These problems eventually lead to preventable admission and unplanned readmission, which impair patients’ physical functions and lower their quality of life. In particular, with an increase in the population of older adults and growing emphasis on active utilization of community-based home care services, there has been an increasing emphasis on the importance of proper transitional care and management of patients who are discharged from acute care providers.
The transition period refers to the time when patients are discharged from the hospital and moved to their homes or nursing facilities.
1 If proper care and management are not provided in this period, it not only increases the burden of diseases such as declining physical functions, increasing severity of the condition, and recurrence of the disease, but also causes economic losses such as medical expenses due to readmission and financial loss of health insurance.
2345
For these reasons, many countries provide translational care for patients through the public system of healthcare support.
6 In the case of the National Care for the Elderly Program launched in the Netherlands in 2008, with the goal of reducing impairment of physical function and loss of independence for discharged patients, older adults, primary care providers, health insurance providers, and local government officials formed a committee at the local community level.
7 In the United States, the Hospital Readmissions Reduction Program (HRRP) was launched in 2012 with the goal of reducing preventable readmissions under the Affordable Care Act (ACA) and Centers for Medicare & Medicaid Services (CMS). At the initial stage of the program introduction, the areas of priority application were heart failure, acute myocardial infarction, and pneumonia. The scope of its application expanded to include hip and knee arthroplasties, chronic obstructive pulmonary disease (COPD) in 2015, and coronary artery bypass grafting in 2017. The HRRP penalized hospitals that exceeded the readmission level predicted based on the readmission rate of a specific disease over the last three years; in the early stage, the penalty was up to 1% of the total annual Medicare Diagnosis-Related Group payment (DRG), but in 2015, it was increased to 3%.
In Korea, as part of a project on the Development of Collaborative System for Public Healthcare of “Regional Healthcare Improvement Measures,” announced in 2019, essential health services in aspects such as cerebral infarction, heart, respiratory system, fractures in older adults, cancer, rehabilitation, chronic diseases, outpatient care planning for discharged patients, and pilot operation of connection to community resources program (discharged patient management project), have been carried out for patients in 50 regional and local accountable care hospitals.
8 As a separate project, the MOHW and Health Insurance Review and Assessment Service (HIRA) are undertaking a pilot project to support discharge management of patients with acute conditions and connect with community services from December 2020 to December 2023 for patients with cerebrovascular diseases in national and public hospitals, general hospitals, or higher.
9 The project entails forming an in-hospital patient support team to evaluate the needs of patients, establish a discharge plan, and provide follow-up management through medical institutions and connections to community services/resources. Support for the pilot project is provided through health insurance. The project is divided into three areas: discharge planning, connecting activities, and follow-up management. For discharge plans, an integrated evaluation fee is provided; for connecting activities, a management fee for connection to community services is provided; and for follow-up management, a fee-for-service is applied for telephone and text message services for the home-based management of discharged patients and fees for patient management between different hospitals.
Korea is at a good starting point since it has also begun providing services to patients during their transition period. However, as the pilot project is still in its infancy, many areas need to be developed and improved for the transitional care service (TCS) to be established and disseminated as a sustainable system. First, standardized service content needs to be developed to provide care during the transition period. Since the goals and detailed services of TCS differ for each country, direct application of the existing TCS in Korean healthcare settings is practically difficult. Thus, we need to establish the goals and directions of TCS implementation in Korea and develop as well as present relevant and appropriate services for the established goals and directions.
Second, the development of indicators for the evaluation of TCS outcomes is required. The US HRRP uses the 30-day readmission rate as an outcome indicator for TCS evaluation. The HIRA in Korea also performed the first evaluation for institutions of general hospitals with 500 beds or more in 2013 treatment records, including the risk-standardized readmission ratio in the Quality Assessment of Healthcare Benefits from 2015, and announced the results in 2015. The second evaluation was carried out for 2017 treatment records, and the third evaluation has been underway since 2021 for the treatment records of 2020.
10
As can be seen in the above cases and examples, it is clear that readmission rate is an important indicator for evaluating the adequacy of care during hospitalization. However, although the readmission rate can serve as one of the indicators for assessing the outcomes of TCS, it is not appropriate to evaluate the entire service and quality of care for TCS using this single indicator when the TCS system has not been fully established. Services provided during the transition period are also a part of services to improve the comprehensive quality of care; provision of services based on comprehensive components using structure and process measures that high-quality care must fulfill, and evaluating the outcomes, are necessary. This is because if TCS is evaluated based on indicators of reduction in unnecessary medical expenses and 30-day readmission rate alone, as reported in previous studies, there may be unexpected negative impacts during the operation of the system. An example is the critical view of an HRRP operating in the United States. According to a previous study examining the negative aspects of implementation of the HRRP system in the United States, after the system was implemented, hospitals did not admit patients immediately, but increased the observation time in the observation unit or the waiting time in the emergency room to avoid being penalized for readmission, thus artificially reducing the 30-day readmission rate.
11 It has also been pointed out that medical institutions with high mortality rates have lower readmission rates, leading to an unanticipated impact of reduced penalties.
12 On the other hand, since the readmission rate involves the sociodemographic characteristics of patients in addition to the treatment capabilities of hospitals, the readmission rate is high in safety-net hospitals that provide treatments for the vulnerable or disadvantaged. Therefore, in practice, although hospitals that actually provide treatments for the underprivileged should receive support so that they can improve their post-discharge management of patients, they are penalized because of using readmission rate as an indicator.
In studies overseas, in addition to using readmission rate as an indicator of TCS, emergency department (ED) visits, mortality rate, and quality of life have been used as evaluation indicators for discharged patient management projects.
131415 Furthermore, in some cases, “providing education and counseling for patients during hospitalization,” which may affect patient skills for post-discharge self-management, is included as an indicator.
1316 In contrast, in the case of a pilot project titled Support of Post-discharge Management and Connection to Community Resources for Patients with Acute Conditions, which was implemented in Korea in 2020, only pre- and post-discharge patient satisfaction and participation were used as indicators; thus, there is a clear need for the development of more comprehensive evaluation indicators.
The detailed services and indicators of TCS in South Korea, which is in the early stages of introduction, need to be considered and presented within a comprehensive framework for improving the quality of care. In addition, as the detailed services of TCS to be provided for patients vary depending on the period of hospitalization/discharge, different evaluation indicators need to be applied to reflect such differences. Therefore, in this study, through application of the quality of care framework presented by the Organization for Economic Co-operation and Development (OECD)’s
17 Health Care Quality and Outcomes Indicators and the UK’s National Health Service (NHS) Outcomes Framework,
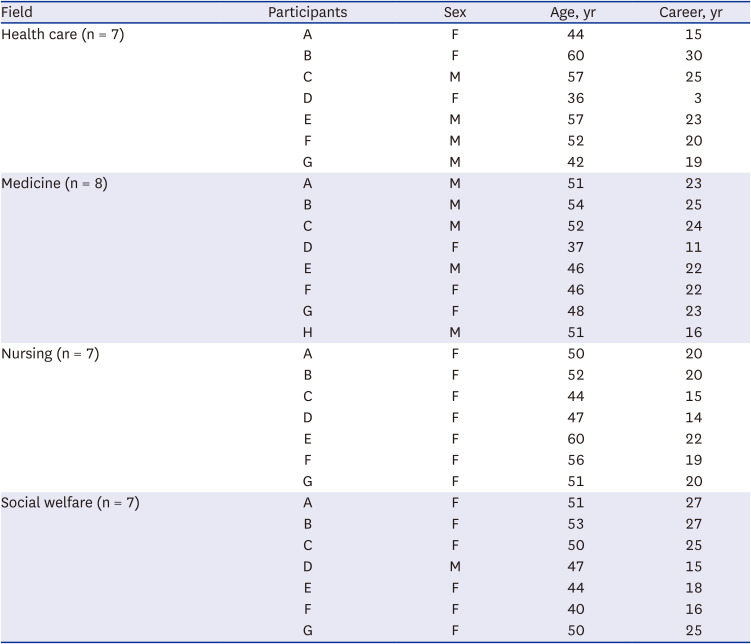
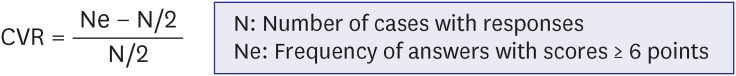
18 we propose detailed service items for respective periods of TCS and the outcome indicators according to the categories of effectiveness, patient safety, and patient centeredness. Through a scoping review of existing works conducted overseas, for each category, a list of services with scientific evidence was prepared. To assess the necessity of the items on this list for provision of TCS in Korea, and adequacy as outcome indicators, expert opinions were collected by applying the Delphi method with a panel of experts and professionals in each field in Korea.
DISCUSSION
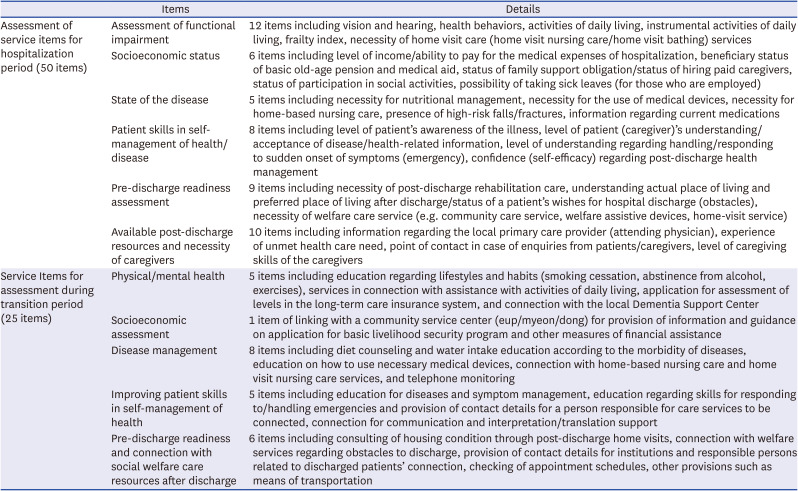
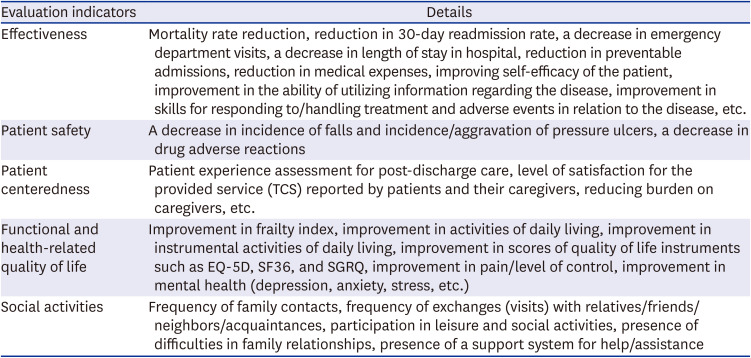
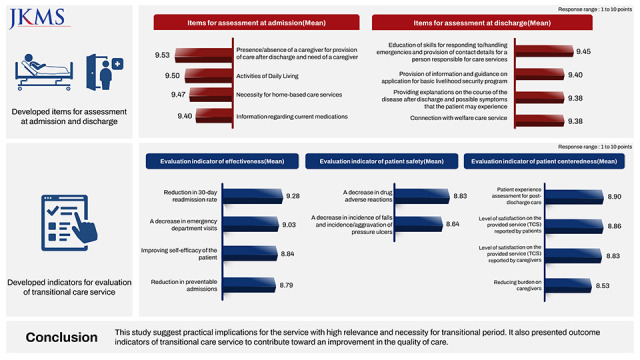
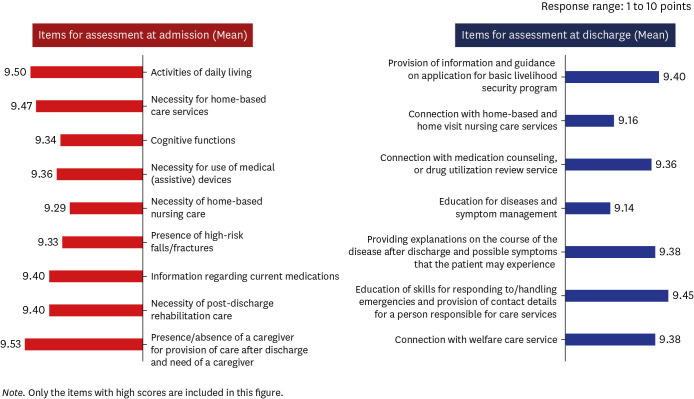
In order to provide effective TCS, the service should begin not from the moment after a patient’s discharge, but from the moment immediately after their admission to establish a discharge plan. During the hospital stay, education to enhance the patient’s health self-management skills is required. In addition, to evaluate the outcomes of services for discharged patients, it is necessary to consider not only simple indicators such as readmission rate, but also other factors such as assessing health and functions of the patient, increasing patient safety, and patient-centeredness, which need to be taken into account to perform a comprehensive evaluation. In this study, a scoping review was conducted to derive the key concepts for the services to be provided during the hospitalization and care transition period, and a Delphi study with a panel of experts was conducted on the derived service items of TCS and evaluation indicators to collect their opinions. The main findings of this study are as follows: First, as a result of the scoping review, themes of service components (assessment of need by different periods of TCS, multi-professional teams, connection to community resources, etc.) and outcome indicators (effectiveness, patient safety, patient-centeredness, etc.) were derived. Second, the items that needed to be assessed during hospitalization and the transition period to provide TCS were categorized, and the results of the three-round Delphi study are as follows: During hospitalization, the presence/absence of a caregiver and need for a caregiver, activities of daily living, and necessity for home-based care services/use of medical devices were identified as service items with high priority of assessment; in terms of patient safety, risk of falls and fracture during hospitalization and necessity for medication reconciliation were rated as items of high priority. During the transition period, the items to be assessed with high priority were provision of education regarding adequate responses and handling of emergencies, guidance on the application of services for basic livelihood security program beneficiaries, and education for patient skills in self-management of health. Third, for the outcome indicators of TCS, categories of effectiveness, patient safety, and patient-centeredness were derived by applying the NHS Outcomes Framework. For each category, the outcome indicators rated with high priority were as follows: In the effectiveness category, the relevance of indicators for a decrease in ED visits, reduction of preventable admissions were rated high, along with a reduction in the 30-day readmission rate. In the patient safety category, a decrease in adverse drug reactions, reduction in incidence of falls, and pressure ulcers were identified as indicators of higher priority. In the patient centeredness category, patient experience assessment, level of service satisfaction reported by patients and their caregivers, and reducing burdens on caregivers were rated as high priority.
In this study, the service components of TCS and evaluation indicators were derived through a scoping review, and a three-round Delphi study was conducted with experts who provide TCS in the fields of health care, medicine, nursing, and social welfare to collect opinions from a variety of interested parties of TCS. Moreover, for outcome indicators, the NHS Outcomes Framework was used as a theoretical framework to derive indicators for the respective categories of effectiveness, patient safety, and patient-centeredness. In addition to the readmission rate, the outcome indicators presented in a project on discharged patient management and patient experience assessment were reviewed to include other indicators, such as functional and health-related quality of life and social activities, for a more comprehensive evaluation.
First, at the time of a patient’s admission, the necessity for assessment of the presence of caregivers and home-based care services, functional health of the patient and current medications, and use of medical devices was rated high. This result supports the findings of a previous study that hospitalization causes functional decline in patients
2526; it also indicates the necessity for medication reconciliation by checking through duplications in prescription of medications, as well as possible adverse drug reactions.
27 Furthermore, if a patient needs to continue using a medical device after being discharged from the hospital, such as an inhaler/aspirator or a blood glucose meter, when the patient is transferred to a home or nursing facility, the necessity for using medical devices needs to be identified, and continuous training is required to ensure proper use of the device for the patient and caregivers.
Second, during the transition period, the necessity for education and connection with community services must be considered. First, for the provision of education, educational programs to explain the possible symptoms that the patient may experience after discharge and for self-management (activities of daily living, taking of medications, use of medical devices, etc.) are required, and education is also needed for methods of handling emergencies for patients and caregivers (formal/informal). In this way, it is expected to improve skills for responding to/handling treatment and adverse events in relation to the disease, as well as enhance self-efficacy and the ability to utilize information regarding the disease. Furthermore, such education is expected to reduce the 30-day readmission rate, preventable readmissions, emergency department visits, and adverse drug reactions. Next, for connection with community services, a high necessity was identified for financial assistance (application for basic livelihood security program benefits, etc.) and linking with home-based/home-visit nursing care services. The results of this study were consistent with those of previous studies. Dronina et al.
28 investigated the need for TCS in older adults and reported that the need for “information on social welfare services/resources available in an area in proximity to the patient’s place of living” was high. As a result of examining the need for financial assistance for older women with liver cancer,
29 patients exhibited a high need (72.2%) for support of connection to community resources through the in-hospital social services team. In other words, there were many cases wherein, after consulting with a nurse at the hospital where the patient was admitted, patients were interested in means of financial assistance through the hospital social services team; however, the eligibility for application for such financial assistance is often limited to near-poverty or low-income families, and the conditions to be qualified as beneficiaries of such assistance tend to involve complicated factors. Thus, a multifaceted approach is required at the hospital and local community levels in terms of connecting patients to community resources and services.
Third, for the effective provision of home-based/home-visit nursing care services, continuing education needs to be provided to the nurses. Since nursing care is provided in a special situation—the home of a patient—and treatments are provided in the absence of fellow medical staff to resolve a patient’s health problem, nurses need to be equipped with various skills to handle these special situations.
3031 In order to develop the clinical decision-making ability of nurses of home-based/home-visit nursing care services, it is necessary to provide continuing education considering their clinical background and a range of educational programs focusing on real-life cases. The connection to community services/resources with these methods is expected to improve the patient’s quality of life and social support systems and reduce the caregivers’ burden of care.
Finally, to improve the quality of care for TCS, a wide range of outcome indicators needs to be considered. Currently, several countries and institutions use the readmission rate as an outcome indicator for the quality of TCS and related policies. In cases overseas, there is a policy program in which hospitals are penalized for high readmission upon assessment of the readmission rates. However, since it is acknowledged that there is a limitation to reducing readmission rate by the efforts of hospitals alone, regional circumstances and environments are considered for the assessment, including whether the care setting in the local community allows transfer of a patient to a nursing hospital after their discharge. In addition, in the United States, readmission is classified based on health insurance claims data and then corrected based on discharge notes. However, since the readmission rate is assessed based on health insurance claims data alone in Korea, regional factors or patient characteristics are not factored in, resulting in practical limitations. The UK NHS Outcomes Framework proposes “support for recovery in quality of life from illness” and presents support in terms of patient safety that helps patients recover from their disease or injury, and in terms of patient-centeredness that evaluates the patient’s experience of care. Accordingly, in the results of this study, as outcome indicators of TCS, the presence of risk of falls and fractures and a decrease in drug adverse reactions in the category of patient safety, and patient experience and satisfaction in the category of patient-centeredness were identified as exhibiting a high need for assessment. Therefore, along with indicators related to effectiveness, those in the categories of patient safety and patient-centeredness must be considered as outcome indicators. Patient safety and experience during hospitalization were assessed to evaluate the quality of care in the present study. However, in the future, if an infrastructure can be developed that allows continuous monitoring for the provision of patient safety and patient-centeredness even after the patient’s discharge and transfer to home or nursing homes, it is expected to contribute to improving the quality of care in hospitals and for TCS.
This study was designed to reflect the opinions of experts in various fields encompassing health care, medicine, nursing, and social welfare, and to include health care professionals currently engaged in the provision of TCS to reflect the real need to practice it. However, since convenience sampling was used for recruiting the panel of experts, it is difficult to generalize the findings of this study. In addition, as this study employed an online survey, it had the advantage of ensuring anonymity and objectivity of opinions; however, there was a disadvantage in that understanding the purpose of the Delphi study and the degree of agreement on responses may be lowered because the participating experts responded individually to the process. Therefore, for future studies, it is necessary to develop and elaborate detailed content related to the provision of TCS from a practical point of view through qualitative research, such as interviews and in-depth interviews with health professionals, patients, and caregivers or guardians.
In this study, a Delphi process was employed as an exploratory methodology to derive priority service items for TCS and evaluation indicators. Through our findings, we presented a method for the provision of tailored services for hospitalization and the transition period, and useful applications for the derived outcome indicators of TCS, which are believed to contribute toward improving the quality of care for TCS.





 PDF
PDF Citation
Citation Print
Print





 XML Download
XML Download