This article has been
cited by other articles in ScienceCentral.
Abstract
Background
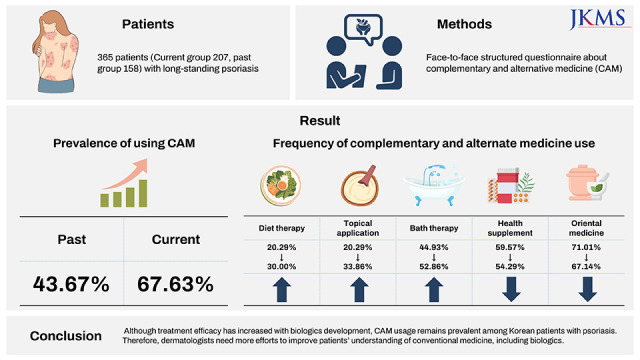
Patients with long-standing psoriasis who are not treated with conventional medicine seek complementary and alternative medicine (CAM). The biological revolution in the field of psoriasis since the late 2000s has progressed, expecting clearance or almost clearance of the disease. The frequency and type of CAM usage may have changed after these advances. We aimed to investigate changes in CAM use in Korean patients with psoriasis before and after the prevalent use of biologics.
Methods
Patients with psoriasis who visited Pusan National University Hospitals (Busan and Yangsan) between March 2020 and June 2022 were made to complete a face-to-face structured questionnaire. These results were compared with our previous study conducted approximately 10 years ago.
Results
In total, 207 patients were included. Compared with the previous results, the frequency of CAM use (67.6%) increased (P < 0.001). Oriental medicine (67.1%) has most commonly been used, followed by health supplements and bath therapy. The biggest reason for using CAM was “to try all the potential treatments.” Meanwhile, negative concerns about conventional medicine (13.5%) significantly decreased during the 10-year period (P < 0.001).
Conclusion
Although treatment efficacy has increased with biologics development, CAM usage remains prevalent among Korean patients with psoriasis. Therefore, dermatologists need more efforts to improve patients’ understanding of conventional medicine, including biologics.
Keywords: Alternative Medicine, Complementary Medicine, Integrative Medicine, Patient Acceptance of Health Care, Psoriasis
INTRODUCTION
Psoriasis is a chronic cutaneous inflammatory disease with a lifelong course of relapse and remission. Many patients complain of decreased quality of life, psychosocial stress due to skin lesions, and a relapsing course.
1 Therefore, patients dissatisfied with their current treatment commonly use complementary and alternative medicine (CAM).
2 This tendency was demonstrated in our previous study on Korean patients with chronic dermatologic diseases, including psoriasis.
34 Furthermore, satisfaction with treatment differed according to the treatment option.
4
Recent advances in immunologic research have enhanced our understanding of the pathophysiology of psoriasis and psoriatic arthritis and the options available for their treatment. The therapeutic options include biological drugs such as tumor necrosis factor inhibitors and interleukin (IL)-12/23 inhibitors. Further discovery of antibodies targeting IL-17 and IL-23 has shown higher efficacy.
However, the prevalence and pattern in the usage of CAM may have changed after the development of biologics. Therefore, we aimed to investigate the changes in CAM usage among Korean patients with psoriasis before and after the biologics revolution.
METHODS
A total of 207 patients with psoriasis who visited the dermatology departments of Pusan National University Hospitals (Busan and Yangsan) between March 2020 and June 2020 were recruited. Psoriasis was diagnosed based on clinical presentation and/or histopathological examination. These results were compared with our previous study conducted from 2008 to 2010.
5 Patients included in the previous study were excluded from the current study.
CAM is defined by the National Institutes of Health as a group of diverse medical and healthcare systems, practices, and products that are not presently considered to be part of conventional medicine.
6 A self-directed questionnaire was designed based on our previous study.
35 Questions related to the use of biological agents were also added to the questionnaire (
Supplementary Table 1). Participants were asked to respond only to CAM use over the past 10 years.
Statistical analysis
T-test, χ2 test, and Spearman’s correlation test were performed using GraphPad Prism 5.0 (GraphPad Software, Inc., San Diego, CA, USA). Statistical significance was defined as a P value less than 0.05.
Ethics statement
The study protocol was approved by the Pusan National University Hospital Institutional Review Board (IRB) (IRB No. 2109-003-106), and informed consent was obtained from all patients included in the study.
RESULTS
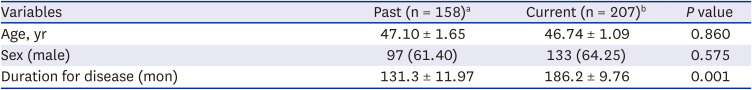
Baseline characteristics
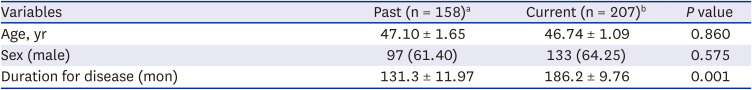
A total of 365 patients were recruited from the past (n = 158) and current (n = 207) studies. The mean age of the patients was 47.10 ± 1.65 years in the past group and 46.74 ± 1.09 years in the current group. Both the past (male:female = 1.6:1) and current groups (male:female = 1.8:1) had a male-dominant distribution of patients. No significant differences in age or sex were observed between both groups. However, a significant difference was noted in the duration of psoriasis; the average duration of psoriasis was 131.3 months in the past group, whereas it was 186.2 months in the current group. The demographic characteristics of the study population are shown in
Table 1.
Table 1
Demographics of study participants
|
Variables |
Past (n = 158)a
|
Current (n = 207)b
|
P value |
|
Age, yr |
47.10 ± 1.65 |
46.74 ± 1.09 |
0.860 |
|
Sex (male) |
97 (61.40) |
133 (64.25) |
0.575 |
|
Duration for disease (mon) |
131.3 ± 11.97 |
186.2 ± 9.76 |
0.001 |
Prevalence and types of CAM usage
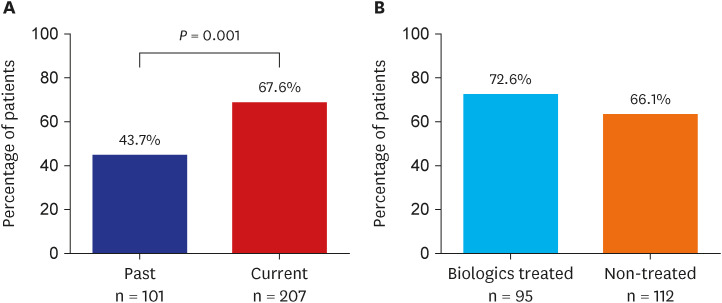
The proportions of the patients in the current and past groups who responded that they used CAM were 67.6% and 43.7%, respectively, which showed a significant difference (P = 0.0001). In the current and past groups, no significant difference in the prevalence of using CAM was observed according to the history of using biologics (72.6% and 66.1%, respectively).
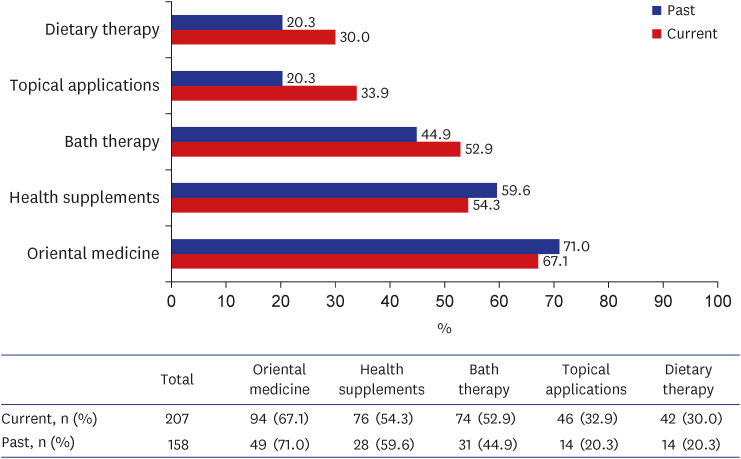
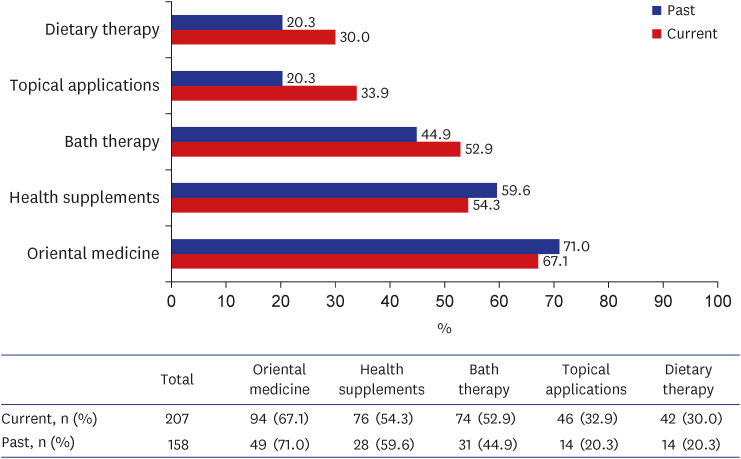
Among patients with a history of CAM usage, oriental medicine was the most commonly used CAM in both past and current groups (71.0%, 49/69 and 67.1%, 94/140, respectively), followed by health supplements, bath therapy, topically applied drugs, and dietary therapy (
Figs. 1 and
2).
Fig. 1
Prevalence of using complementary and alternative medicine. (A) Prevalence of using complementary and alternative medicine. (B) The current prevalence of using complementary and alternative medicine according to the use of biologics.
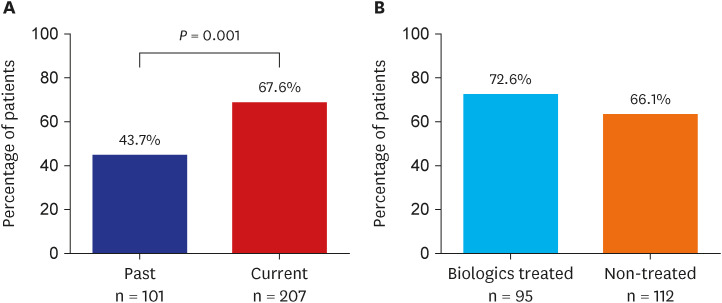
Fig. 2
Frequency of complementary and alternate medicine use according to its subtypes.
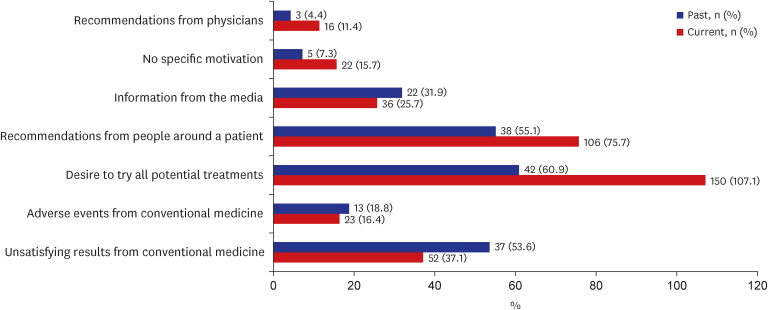
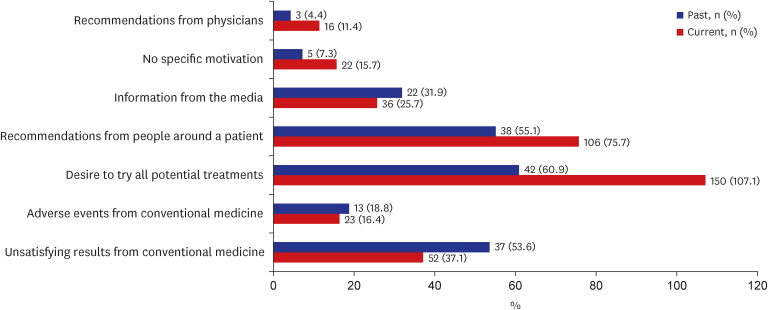
Reasons for CAM use
The main reason for CAM use was the “desire to try all potential treatments” in the past and current groups (frequency of response, 60.9% and 107.1%, respectively). The frequency of “unsatisfactory results from conventional medicine” responses decreased from 53.6% in the past group to 37.1% in the current group. The frequency of “recommendations from physicians” responses was the lowest in both groups (4.4% and 11.4%, respectively) (
Fig. 3).
Fig. 3
Reasons for complementary and alternate medicine use. The past group was instructed to respond to only one item, but the current group was guided to respond by the subtype of the CAM used, so duplicated answers were included. The denominator was based on the number of people who answered that they used CAM.
CAM = complementary and alternative medicine.
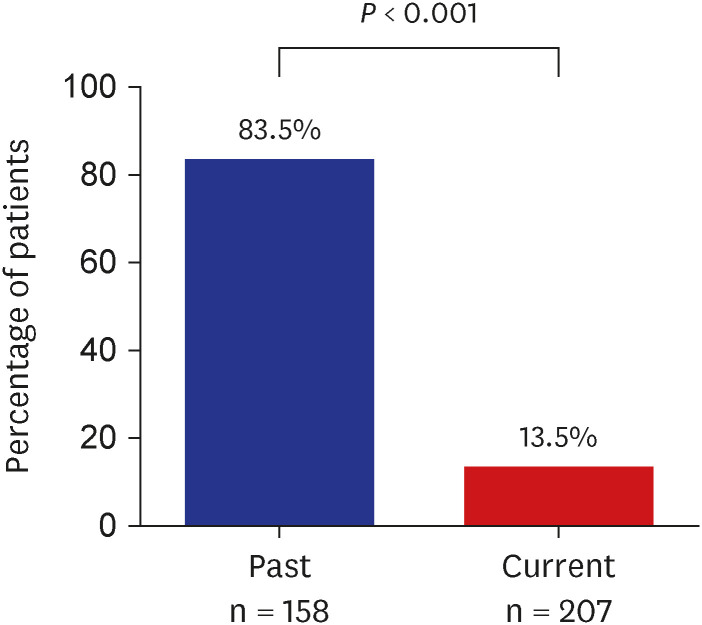
Patients’ concerns about conventional medicine
In the past group, 83.5% of the patients answered that they had negative concerns about conventional medicine, whereas only 13.5% had such concerns in the current group.
In the past group, the frequency of opinion that conventional medicine caused “frequent side effects” was the highest at 87.9%; however, only a quarter of the participants in the current group had the same opinion. In addition, the frequency of “poorly accessible” responses decreased from 31.1% in the past group to 3.6% in the current group but that of “incurability” responses increased from 32.58% in the past group to 57.1% in the current group. No significant difference in negative concerns about conventional medicine was noted among the respondents who had a history of using biologics (
Figs. 4 and
5;
Supplementary Fig. 1).
Fig. 4
Negative concerns about conventional medicine. The denominator was based on the number of people who answered that they used complementary alternative medicine.
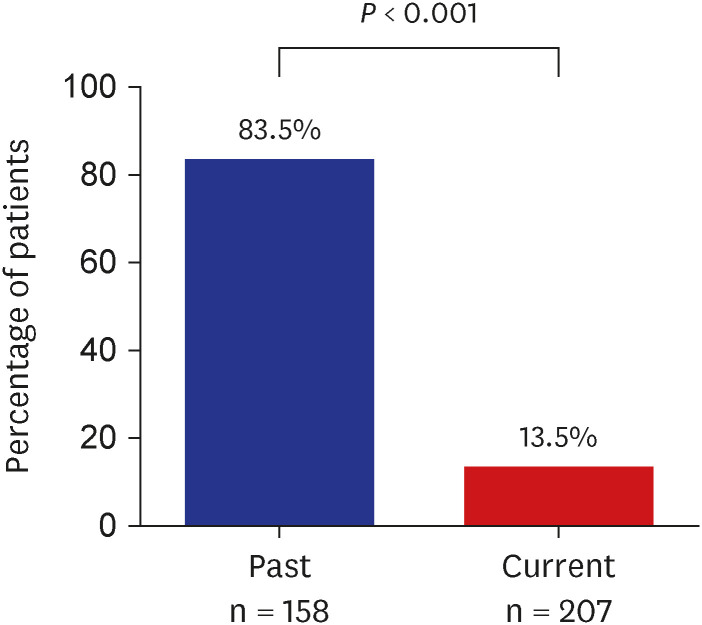
Fig. 5
Details on negative concerns about conventional medicine. The denominator was based on the number of people who answered that they used complementary and alternative medicine.

Patients’ satisfaction and subjective efficacy with CAM
The proportion of patients who responded that the CAM was satisfactory (rated by the patients as “very good” or “good”) was less than 20% in both groups. In both groups, the proportion of patients who were satisfied with health supplements was the highest at 17.9% in the past group and 13.2% in the current group, respectively. In the past group, Oriental medicine showed the lowest satisfaction rate at 6.1%, while topical applicants showed the lowest satisfaction rate at 2.8% in the current group.
The proportion of patients who responded that CAM was effective (rated by the patients as “continuous improvement” or “temporary improvement”) ranged from 21.4% to 57.1%, according to CAM usage in the past group. However, in the current group, it ranged from 18.9 to 41.1%, indicating that the overall subjective efficacy was reduced (
Supplementary Figs. 2 and
3).
DISCUSSION
Many studies have been conducted on sociodemographic factors, such as age, sex, education level, and area of residence, which influence the use of CAM. However, research on the use of CAM based on changes in conventional medicine is limited.
78 Advancement of biologics in patients with psoriasis has led to a change in treatment paradigms. This study aimed to analyze the changes in CAM usage in patients before and after the revolution of biologics. The data from this study will help show the relationship between treatment advances and changes in CAM usage.
This study showed a significant increase in the usage of CAM despite advances in psoriasis treatment modalities, such as biologics. In addition, no significant difference was observed in the order of patients’ usage in the subtype of CAM used between the past and current groups. In previous studies conducted on Koreans, the CAM usage rate increased from 29% in 1999 to about 75% in 2006.
9
Several reasons can be found for these findings: First, the difference in the disease duration between the past and current groups seems to be a reason for the increase in CAM usage. Second, high expectations to find a cure for patients with psoriasis may have caused high rates of CAM usage. Third, CAM-related indiscriminate mass media advertisements and increased accessibility to CAM may have led to an increase in its usage. Lastly, despite the increase in the development and use of highly effective biologics, the growing awareness of the difficulty in radical cures may have been a factor responsible.
Interestingly, when we evaluated the reason for increased CAM usage, both the past and current groups had the lowest proportion of patients with physician recommendations. This indicates that physicians prefer conventional medicine over CAM. The decrease in the frequency of “unsatisfactory outcomes of conventional medicine” responses is considered a result of the revolution of biologics.
Recently, negative concerns about conventional medicine and dissatisfaction with its treatment effects have also decreased. This has been achieved through the development of biologics and the efforts of the medical profession by increasing the therapeutic effect of biologics as well as expanding information on conventional medicine to patients through various media. This change in perception is thought to be a positive factor in helping patients actively use conventional medicine and achieve better treatment outcomes.
Satisfaction rates for each subtype of CAM ranged from “very good” to “good” at 6.1–17.9%, while the subjective efficacy rates of CAM ranged from “continuous improvement” and “temporary improvement” at 2.8–13.5%. Satisfaction and subjective efficacy of CAM were relatively low. In addition, when the past and current groups were compared, the evaluation of patient satisfaction and the effectiveness of CAM decreased over time.
This study had several limitations. This study was conducted at tertiary hospitals with a relatively small number of patients. In addition, comparisons were made between patient groups based on demographic differences, such as disease duration, and the patients had a long recall period.
In conclusion, despite advances in biologics, CAM usage remains high in Korean patients with psoriasis. This finding shows that conventional medicine has not yet met the needs of the patients. A lack of understanding of conventional medicine or patients’ higher treatment goals for the current treatment could be a reason. Further research on this topic is required. In the future, dermatologists should focus more on the needs of patients before proceeding with treatment. Moreover, more precise guidance must be provided to patients regarding the correct use of CAM.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download