1. Lin X, Xu Y, Pan X, Xu J, Ding Y, Sun X, Song X, Ren Y, Shan PF. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci Rep. 2020; 10:14790. PMID:
32901098.
2. Naser KA, Gruber A, Thomson GA. The emerging pandemic of obesity and diabetes: are we doing enough to prevent a disaster? Int J Clin Pract. 2006; 60:1093–1097. PMID:
16939551.
3. Kannenkeril D, Karg MV, Bosch A, Ott C, Linz P, Nagel AM, Uder M, Schmieder RE. Tissue sodium content in patients with type 2 diabetes mellitus. J Diabetes Complications. 2019; 33:485–489. PMID:
31101486.
4. Radzeviciene L, Ostrauskas R. Adding salt to meals as a risk factor of type 2 diabetes mellitus: a case-control study. Nutrients. 2017; 9:67. PMID:
28098780.
5. Han S, Cheng D, Liu N, Kuang H. The relationship between diabetic risk factors, diabetic complications and salt intake. J Diabetes Complications. 2018; 32:531–537. PMID:
29534865.
6. Premilovac D, Richards SM, Rattigan S, Keske MA. A vascular mechanism for high-sodium-induced insulin resistance in rats. Diabetologia. 2014; 57:2586–2595. PMID:
25212260.
7. Kim MK. Dietary sodium intake in patients with type 2 diabetes mellitus. Diabetes Metab J. 2016; 40:280–282. PMID:
27550209.
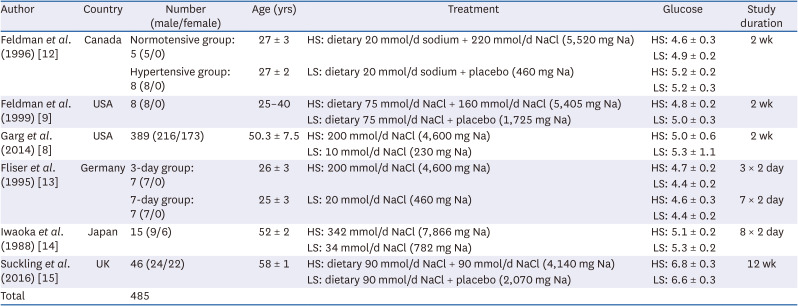
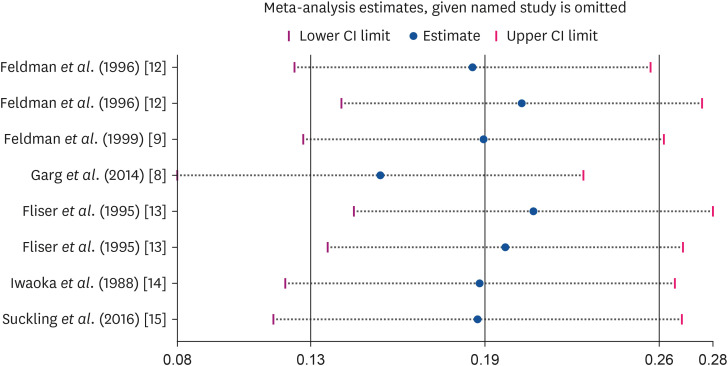
8. Garg R, Williams GH, Hurwitz S, Brown NJ, Hopkins PN, Adler GK. Low-salt diet increases insulin resistance in healthy subjects. Metabolism. 2011; 60:965–968. PMID:
21036373.
9. Feldman RD, Schmidt ND. Moderate dietary salt restriction increases vascular and systemic insulin resistance. Am J Hypertens. 1999; 12:643–647. PMID:
10371376.
10. Wellek S, Blettner M. On the proper use of the crossover design in clinical trials: part 18 of a series on evaluation of scientific publications. Dtsch Arztebl Int. 2012; 109:276–281. PMID:
22567063.
11. Wang T, Malone J, Fu H, Heilmann C, Qu Y, Huster WJ. Crossover design and its application in late-phase diabetes studies. J Diabetes. 2016; 8:610–618. PMID:
27100270.
12. Feldman RD, Logan AG, Schmidt ND. Dietary salt restriction increases vascular insulin resistance. Clin Pharmacol Ther. 1996; 60:444–451. PMID:
8873692.
13. Fliser D, Fode P, Arnold U, Nowicki M, Kohl B, Ritz E. The effect of dietary salt on insulin sensitivity. Eur J Clin Invest. 1995; 25:39–43. PMID:
7705385.
14. Iwaoka T, Umeda T, Ohno M, Inoue J, Naomi S, Sato T, Kawakami I. The effect of low and high NaCl diets on oral glucose tolerance. Klin Wochenschr. 1988; 66:724–728. PMID:
3050268.
15. Suckling RJ, He FJ, Markandu ND, MacGregor GA. Modest salt reduction lowers blood pressure and albumin excretion in impaired glucose tolerance and type 2 diabetes mellitus: a randomized double-blind trial. Hypertension. 2016; 67:1189–1195. PMID:
27160199.
16. Raji A, Williams GH, Jeunemaitre X, Hopkins PN, Hunt SC, Hollenberg NK, Seely EW. Insulin resistance in hypertensives: effect of salt sensitivity, renin status and sodium intake. J Hypertens. 2001; 19:99–105. PMID:
11204310.
17. Townsend RR, Kapoor S, McFadden CB. Salt intake and insulin sensitivity in healthy human volunteers. Clin Sci (Lond). 2007; 113:141–148. PMID:
17425514.
18. Gomi T, Shibuya Y, Sakurai J, Hirawa N, Hasegawa K, Ikeda T. Strict dietary sodium reduction worsens insulin sensitivity by increasing sympathetic nervous activity in patients with primary hypertension. Am J Hypertens. 1998; 11:1048–1055. PMID:
9752889.
19. Oh H, Lee HY, Jun DW, Lee SM. Low salt diet and insulin resistance. Clin Nutr Res. 2016; 5:1–6. PMID:
26839871.
20. Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, Baugh V, Bekedam H, Billo N, Casswell S, et al. Priority actions for the non-communicable disease crisis. Lancet. 2011; 377:1438–1447. PMID:
21474174.
21. World Health Organization. Guideline: Sodium Intake for Adults and Children. Geneva: World Health Organization;2012.
22. Lima NK, Tozetto DJ, Lima LG, Nobre F, Moriguti JC, Ferriolli E, Foss MC. Salt and insulin sensitivity after short and prolonged high salt intake in elderly subjects. Braz J Med Biol Res. 2009; 42:738–743. PMID:
19649400.
23. Laws A, Reaven GM. Effect of physical activity on age-related glucose intolerance. Clin Geriatr Med. 1990; 6:849–863. PMID:
2224751.
24. Shamshirgaran SM, Mamaghanian A, Aliasgarzadeh A, Aiminisani N, Iranparvar-Alamdari M, Ataie J. Age differences in diabetes-related complications and glycemic control. BMC Endocr Disord. 2017; 17:25. PMID:
28472985.
25. Abdullah MF, Sidi H, Ravindran A, Gosse PJ, Kaunismaa ES, Mainland RL, Mustafa N, Hatta NH, Arnawati P, Zulkifli AY, et al. How much do we know about the biopsychosocial predictors of glycaemic control? Age and clinical factors predict glycaemic control, but psychological factors do not. J Diabetes Res. 2020; 2020:2654208. PMID:
32455131.
26. Vasdev S, Gill VD, Parai S, Gadag V. Effect of moderately high dietary salt and lipoic acid on blood pressure in Wistar-Kyoto rats. Exp Clin Cardiol. 2007; 12:77–81. PMID:
18650986.
27. Alderman MH. Evidence relating dietary sodium to cardiovascular disease. J Am Coll Nutr. 2006; 25:256S–261S. PMID:
16772637.
28. He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013; 346:f1325. PMID:
23558162.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download