1. United Nations. World Population Ageing 2017 - Highlights (ST/ESA/SER.A/397). New York (NY): UN;2017.
2. Arredondo A, Aviles R. Costs and epidemiological changes of chronic diseases: implications and challenges for health systems. PLoS One. 2015; 10:e0118611. PMID:
25781625.

3. Kennedy BK, Berger SL, Brunet A, Campisi J, Cuervo AM, Epel ES, Franceschi C, Lithgow GJ, Morimoto RI, Pessin JE, et al. Aging: a common driver of chronic diseases and a target for novel interventions. Cell. 2014; 159:709–713. PMID:
25417146.
5. Sowa A, Tobiasz-Adamczyk B, Topór-Mądry R, Poscia A, la Milia DI. Predictors of healthy ageing: public health policy targets. BMC Health Serv Res. 2016; 16(Suppl 5):289. PMID:
27609315.

6. Hanson MA, Cooper C, Aihie Sayer A, Eendebak RJ, Clough GF, Beard JR. Developmental aspects of a life course approach to healthy ageing. J Physiol. 2016; 594:2147–2160. PMID:
26518329.

7. Crichton GE, Alkerwi A. Physical activity, sedentary behavior time and lipid levels in the Observation of Cardiovascular Risk Factors in Luxembourg study. Lipids Health Dis. 2015; 14:87. PMID:
26256803.

8. Qiu S, Cai X, Schumann U, Velders M, Sun Z, Steinacker JM. Impact of walking on glycemic control and other cardiovascular risk factors in type 2 diabetes: a meta-analysis. PLoS One. 2014; 9:e109767. PMID:
25329391.

9. Friedenreich CM, Neilson HK, Farris MS, Courneya KS. Physical activity and cancer outcomes: a precision medicine approach. Clin Cancer Res. 2016; 22:4766–4775. PMID:
27407093.

10. Bherer L, Erickson KI, Liu-Ambrose T. A review of the effects of physical activity and exercise on cognitive and brain functions in older adults. J Aging Res. 2013; 2013:657508. PMID:
24102028.

11. Steffl M, Bohannon RW, Sontakova L, Tufano JJ, Shiells K, Holmerova I. Relationship between sarcopenia and physical activity in older people: a systematic review and meta-analysis. Clin Interv Aging. 2017; 12:835–845. PMID:
28553092.

12. Iolascon G, Di Pietro G, Gimigliano F, Mauro GL, Moretti A, Giamattei MT, Ortolani S, Tarantino U, Brandi ML. Physical exercise and sarcopenia in older people: position paper of the Italian Society of Orthopaedics and Medicine (OrtoMed). Clin Cases Miner Bone Metab. 2014; 11:215–221. PMID:
25568656.

13. Welk GJ. Physical Activity Assessments for Health-Related Research. Champaign (IL): Human Kinetics;2002.
14. WHO. Global Recommendations on Physical Activity for Health. Geneva: WHO Press;2010.
15. Pinheiro Volp AC, Esteves de Oliveira FC, Duarte Moreira Alves R, Esteves EA, Bressan J. Energy expenditure: components and evaluation methods. Nutr Hosp. 2011; 26:430–440. PMID:
21892558.
16. Ndahimana D, Kim EK. Measurement methods for physical activity and energy expenditure: a review. Clin Nutr Res. 2017; 6:68–80. PMID:
28503503.

17. Crouter SE, Clowers KG, Bassett DR Jr. A novel method for using accelerometer data to predict energy expenditure. J Appl Physiol (1985). 2006; 100:1324–1331. PMID:
16322367.

19. Lyden K, Kozey SL, Staudenmeyer JW, Freedson PS. A comprehensive evaluation of commonly used accelerometer energy expenditure and MET prediction equations. Eur J Appl Physiol. 2011; 111:187–201. PMID:
20842375.

20. Santos-Lozano A, Santín-Medeiros F, Cardon G, Torres-Luque G, Bailón R, Bergmeir C, Ruiz JR, Lucia A, Garatachea N. ActiGraph GT3X: validation and determination of physical activity intensity cut points. Int J Sports Med. 2013; 34:975–982. PMID:
23700330.

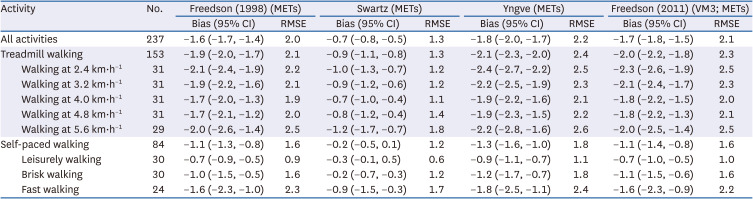
21. Aguilar-Farias N, Peeters GM, Brychta RJ, Chen KY, Brown WJ. Comparing ActiGraph equations for estimating energy expenditure in older adults. J Sports Sci. 2019; 37:188–195. PMID:
29912666.

22. Hall KS, Howe CA, Rana SR, Martin CL, Morey MC. METs and accelerometry of walking in older adults: standard versus measured energy cost. Med Sci Sports Exerc. 2013; 45:574–582. PMID:
23059862.
23. Jones LM, Waters DL, Legge M. Walking speed at self-selected exercise pace is lower but energy cost higher in older versus younger women. J Phys Act Health. 2009; 6:327–332. PMID:
19564661.

24. Whitcher L, Papadopoulos C. Accelerometer derived activity counts and oxygen consumption between young and older individuals. J Aging Res. 2014; 2014:184693. PMID:
25006459.

25. Pinnington HC, Wong P, Tay J, Green D, Dawson B. The level of accuracy and agreement in measures of FEO
2, FECO
2 and VE between the Cosmed K4b
2 portable, respiratory gas analysis system and a metabolic cart. J Sci Med Sport. 2001; 4:324–335. PMID:
11702919.

26. McLaughlin JE, King GA, Howley ET, Bassett DR Jr, Ainsworth BE. Validation of the COSMED K4 b
2 portable metabolic system. Int J Sports Med. 2001; 22:280–284. PMID:
11414671.

27. Schrack JA, Simonsick EM, Ferrucci L. Comparison of the Cosmed K4b
2 portable metabolic system in measuring steady-state walking energy expenditure. PLoS One. 2010; 5:e9292. PMID:
20174583.
28. Mcminn D, Acharya R, Rowe DA, Gray SR, Allan JL. Measuring activity energy expenditure: accuracy of the GT3X+ and Actiheart monitors. Int J Exerc Sci. 2013; 6:217–229.
29. Aadland E, Ylvisåker E. Reliability of the ActiGraph GT3X+ accelerometer in adults under free-living conditions. PLoS One. 2015; 10:e0134606. PMID:
26274586.

30. Schneller MB, Pedersen MT, Gupta N, Aadahl M, Holtermann A. Validation of five minimally obstructive methods to estimate physical activity energy expenditure in young adults in semi-standardized settings. Sensors (Basel). 2015; 15:6133–6151. PMID:
25781506.

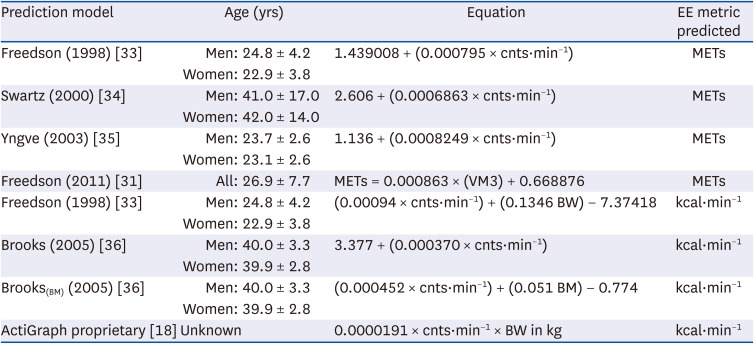
31. Sasaki JE, John D, Freedson PS. Validation and comparison of ActiGraph activity monitors. J Sci Med Sport. 2011; 14:411–416. PMID:
21616714.

32. Robusto KM, Trost SG. Comparison of three generations of ActiGraph™ activity monitors in children and adolescents. J Sports Sci. 2012; 30:1429–1435. PMID:
22857599.

33. Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc. 1998; 30:777–781. PMID:
9588623.

34. Swartz AM, Strath SJ, Bassett DR Jr, O’Brien WL, King GA, Ainsworth BE. Estimation of energy expenditure using CSA accelerometers at hip and wrist sites. Med Sci Sports Exerc. 2000; 32:S450–S456. PMID:
10993414.

35. Yngve A, Nilsson A, Sjöström M, Ekelund U. Effect of monitor placement and of activity setting on the MTI accelerometer output. Med Sci Sports Exerc. 2003; 35:320–326. PMID:
12569223.

36. Brooks AG, Gunn SM, Withers RT, Gore CJ, Plummer JL. Predicting walking METs and energy expenditure from speed or accelerometry. Med Sci Sports Exerc. 2005; 37:1216–1223. PMID:
16015141.

37. Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, O’Brien WL, Bassett DR, Schmitz KH, Emplaincourt PO, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000; 32:S498–S516. PMID:
10993420.

38. Institute of Medicine of the National Academies (US). Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Washington, D.C.: National Academies Press;2002.
39. Byrne NM, Hills AP, Hunter GR, Weinsier RL, Schutz Y. Metabolic equivalent: one size does not fit all. J Appl Physiol (1985). 2005; 99:1112–1119. PMID:
15831804.

40. Kwan M, Woo J, Kwok T. The standard oxygen consumption value equivalent to one metabolic equivalent (3.5 ml/min/kg) is not appropriate for elderly people. Int J Food Sci Nutr. 2004; 55:179–182. PMID:
15223593.

41. Bird SR, Hawley JA. Update on the effects of physical activity on insulin sensitivity in humans. BMJ Open Sport Exerc Med. 2017; 2:e000143.

42. Mansikkamäki K, Raitanen J, Nygård CH, Tomás E, Rutanen R, Luoto R. Long-term effect of physical activity on health-related quality of life among menopausal women: a 4-year follow-up study to a randomised controlled trial. BMJ Open. 2015; 5:e008232.

43. Crouter SE, Churilla JR, Bassett DR Jr. Estimating energy expenditure using accelerometers. Eur J Appl Physiol. 2006; 98:601–612. PMID:
17058102.

44. Ortega JD, Farley CT. Individual limb work does not explain the greater metabolic cost of walking in elderly adults. J Appl Physiol (1985). 2007; 102:2266–2273. PMID:
17363623.

45. Mian OS, Thom JM, Ardigò LP, Narici MV, Minetti AE. Metabolic cost, mechanical work, and efficiency during walking in young and older men. Acta Physiol (Oxf). 2006; 186:127–139. PMID:
16497190.





 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download