1. Kim HS, Lee US, Kim SH, Cha YS. Evaluation of dietary habits according to breakfast consumption in Korean adolescents: based on the 6th Korea National Health and Nutrition Examination Survey, 2013–2015. J Nutr Health. 2019; 52:217–226.

2. Deshmukh-Taskar PR, Nicklas TA, O'Neil CE, Keast DR, Radcliffe JD, Cho S. The relationship of breakfast skipping and type of breakfast consumption with nutrient intake and weight status in children and adolescents: the National Health and Nutrition Examination Survey 1999–2006. J Am Diet Assoc. 2010; 110:869–878. PMID:
20497776.

3. Christensen CB, Mikkelsen BE, Toft U. The effect of introducing a free breakfast club on eating habits among students at vocational schools. BMC Public Health. 2019; 19:369. PMID:
30943941.

4. Oh YJ. A study on the factors of dietary life related to breakfast in high school students [master's thesis]. Gyeongsan: Yeungnam University;2008.
5. Smith KJ, Gall SL, McNaughton SA, Blizzard L, Dwyer T, Venn AJ. Skipping breakfast: longitudinal associations with cardiometabolic risk factors in the Childhood Determinants of Adult Health Study. Am J Clin Nutr. 2010; 92:1316–1325. PMID:
20926520.

6. Freitas Júnior IF, Christofaro DGD, Codogno JS, Monteiro PA, Silveira LS, Fernandes RA. The association between skipping breakfast and biochemical variables in sedentary obese children and adolescents. J Pediatr. 2012; 161:871–874. PMID:
22682613.

7. Mustafa N, Abd Majid H, Toumpakari Z, Carroll HA, Yazid Jalaludin M, Al Sadat N, Johnson L. The association of breakfast frequency and cardiovascular disease (CVD) risk factors among adolescents in Malaysia. Nutrients. 2019; 11:973.

8. Guasch-Ferré M, Hruby A, Toledo E, Clish CB, Martínez-González MA, Salas-Salvadó J, Hu FB. Metabolomics in prediabetes and diabetes: a systematic review and meta-analysis. Diabetes Care. 2016; 39:833–846. PMID:
27208380.

9. Roberts LD, Koulman A, Griffin JL. Towards metabolic biomarkers of insulin resistance and type 2 diabetes: progress from the metabolome. Lancet Diabetes Endocrinol. 2014; 2:65–75. PMID:
24622670.

10. Tillin T, Hughes AD, Wang Q, Würtz P, Ala-Korpela M, Sattar N, Forouhi NG, Godsland IF, Eastwood SV, McKeigue PM, et al. Diabetes risk and amino acid profiles: cross-sectional and prospective analyses of ethnicity, amino acids and diabetes in a South Asian and European cohort from the SABRE (Southall And Brent REvisited) Study. Diabetologia. 2015; 58:968–979. PMID:
25693751.

11. Wang-Sattler R, Yu Z, Herder C, Messias AC, Floegel A, He Y, Heim K, Campillos M, Holzapfel C, Thorand B, et al. Novel biomarkers for pre-diabetes identified by metabolomics. Mol Syst Biol. 2012; 8:615. PMID:
23010998.

12. Frohnert BI, Rewers MJ. Metabolomics in childhood diabetes. Pediatr Diabetes. 2016; 17:3–14.

13. Wang TJ, Larson MG, Vasan RS, Cheng S, Rhee EP, McCabe E, Lewis GD, Fox CS, Jacques PF, Fernandez C, et al. Metabolite profiles and the risk of developing diabetes. Nat Med. 2011; 17:448–453. PMID:
21423183.

14. Jung SJ, Chae SW. Effects of adherence to Korean diets on serum GGT and cardiovascular disease risk factors in patients with hypertension and diabetes. J Nutr Health. 2018; 51:386.

15. Choi E, Kim SA, Joung H. Relationship between obesity and Korean and Mediterranean dietary patterns: a review of the literature. J Obes Metab Syndr. 2019; 28:30–39. PMID:
31089577.

16. Kim J, Jo I. Grains, vegetables, and fish dietary pattern is inversely associated with the risk of metabolic syndrome in South Korean adults. J Am Diet Assoc. 2011; 111:1141–1149. PMID:
21802559.

17. Song Y, Joung H. A traditional Korean dietary pattern and metabolic syndrome abnormalities. Nutr Metab Cardiovasc Dis. 2012; 22:456–462. PMID:
21215606.

18. Cha YS, Kim SR, Yang JA, Back HI, Kim MG, Jung SJ, Song WO, Chae SW. Kochujang, fermented soybean-based red pepper paste, decreases visceral fat and improves blood lipid profiles in overweight adults. Nutr Metab (Lond). 2013; 10:24. PMID:
23442518.

19. Jin EH. A study on health related action rates of dietary guidelines and pattern of dietary in middle-aged women. J Korean Soc Health Inf Health Stat. 2009; 34:12.
20. Song Y, Park MJ, Paik HY, Joung H. Secular trends in dietary patterns and obesity-related risk factors in Korean adolescents aged 10–19 years. Int J Obes. 2010; 34:48–56.

21. Choi WH, Ahn JY, Jung CH, Seo JS, Ha TY. Korean diet prevents obesity and ameliorates insulin resistance in mice fed a high-fat diet. J Ethn Foods. 2017; 4:36–43.

22. Monzani A, Ricotti R, Caputo M, Solito A, Archero F, Bellone S, Prodam F. A systematic review of the association of skipping breakfast with weight and cardiometabolic risk factors in children and adolescents. What should we better investigate in the future? Nutrients. 2019; 11:387.

23. O'Neil CE, Byrd-Bredbenner C, Hayes D, Jana L, Klinger SE, Stephenson-Martin S. The role of breakfast in health: definition and criteria for a quality breakfast. J Acad Nutr Diet. 2014; 114:S8–26.
24. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985; 28:412–419. PMID:
3899825.

25. Armstrong T, Bull F. Development of the World Health Organization global physical activity questionnaire. J Public Health. 2006; 14:66–70.

26. Kang MH, Choi MK, Kim MH. Evaluation of energy and nutrient intake as well as dietary behaviors in elementary school and middle school students residing in Chungnam according to breakfast eating status. J Korean Diet Assoc. 2011; 17:18–31.
27. Baek HI, Jung SY, Ha KC, Kim HM, Choi EK, Jung SJ, Park EO, Shin SW, Kim MG, Yun SK, et al. Effect of Chongkukjang on histamine-induced skin wheal response: a randomized, double-blind, placebo-controlled trial. J Ethn Foods. 2015; 2:52–57.

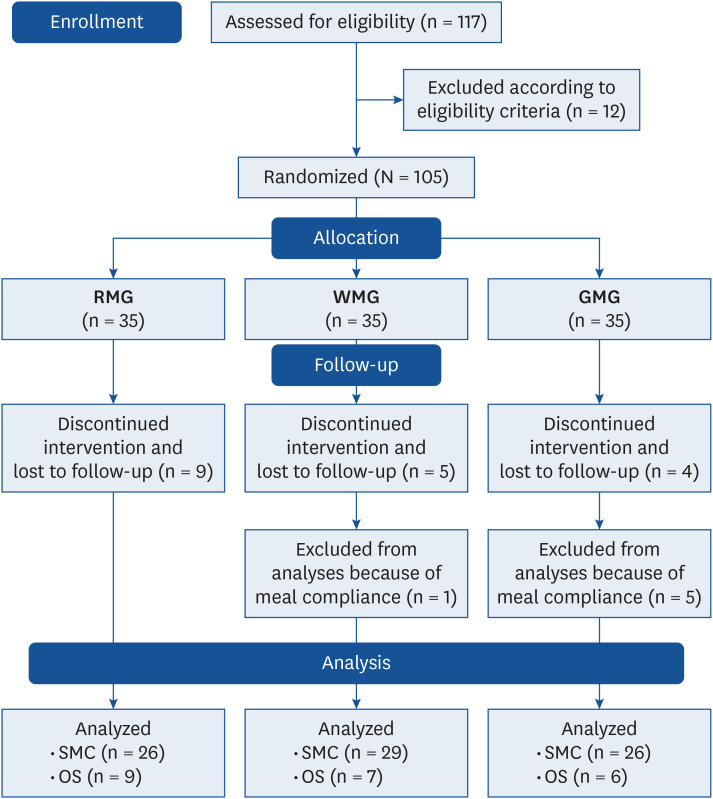
28. Kim HS, Jung SJ, Mun EG, Kim MS, Cho SM, Cha YS. Effects of a rice-based diet in Korean adolescents who habitually skip breakfast: a randomized, parallel group clinical trial. Nutrients. 2021; 13:853. PMID:
33807703.

29. Timlin MT, Pereira MA, Story M, Neumark-Sztainer D. Breakfast eating and weight change in a 5-year prospective analysis of adolescents: Project EAT (Eating Among Teens). Pediatrics. 2008; 121:e638–e645. PMID:
18310183.

30. Esmaillzadeh A, Kimiagar M, Mehrabi Y, Azadbakht L, Hu FB, Willett WC. Dietary patterns, insulin resistance, and prevalence of the metabolic syndrome in women. Am J Clin Nutr. 2007; 85:910–918. PMID:
17344515.

31. Livingstone MB, Prentice AM, Coward WA, Strain JJ, Black AE, Davies PS, Stewart CM, McKenna PG, Whitehead RG. Validation of estimates of energy intake by weighed dietary record and diet history in children and adolescents. Am J Clin Nutr. 1992; 56:29–35. PMID:
1609757.

32. Kowalkowska J, Slowinska MA, Slowinski D, Dlugosz A, Niedzwiedzka E, Wadolowska L. Comparison of a full food-frequency questionnaire with the three-day unweighted food records in young Polish adult women: implications for dietary assessment. Nutrients. 2013; 5:2747–2776. PMID:
23877089.

33. Park JH, Mun S, Choi DP, Lee JY, Kim HC. Association between changes in anthropometric indices and in fasting insulin levels among Healthy Korean adolescents: the JS High School Study. Diabetes Metab J. 2019; 43:183–191. PMID:
30688051.

34. Nguyen QM, Srinivasan SR, Xu JH, Chen W, Berenson GS. Changes in risk variables of metabolic syndrome since childhood in pre-diabetic and type 2 diabetic subjects: the Bogalusa Heart Study. Diabetes Care. 2008; 31:2044–2049. PMID:
18628566.

35. Srinivasan SR, Myers L, Berenson GS. Changes in metabolic syndrome variables since childhood in prehypertensive and hypertensive subjects: the Bogalusa Heart Study. Hypertension. 2006; 48:33–39. PMID:
16769996.

36. Pereira MA, Erickson E, McKee P, Schrankler K, Raatz SK, Lytle LA, Pellegrini AD. Breakfast frequency and quality may affect glycemia and appetite in adults and children. J Nutr. 2011; 141:163–168. PMID:
21123469.

37. Soriguer F, Colomo N, Olveira G, García-Fuentes E, Esteva I, Ruiz de Adana MS, Morcillo S, Porras N, Valdés S, Rojo-Martínez G. White rice consumption and risk of type 2 diabetes. Clin Nutr. 2013; 32:481–484. PMID:
23200927.

38. Kim EK, An SY, Lee MS, Kim TH, Lee HK, Hwang WS, Choe SJ, Kim TY, Han SJ, Kim HJ, et al. Fermented kimchi reduces body weight and improves metabolic parameters in overweight and obese patients. Nutr Res. 2011; 31:436–443. PMID:
21745625.

39. Cui M, Kim HY, Lee KH, Jeong JK, Hwang JH, Yeo KY, Ryu BH, Choi JH, Park KY. Antiobesity effects of kimchi in diet-induced obese mice. J Ethn Foods. 2015; 2:137–144.

40. Islam MS, Choi H. Antidiabetic effect of Korean traditional Baechu (Chinese cabbage) kimchi in a type 2 diabetes model of rats. J Med Food. 2009; 12:292–297. PMID:
19459728.

41. Rave K, Roggen K, Dellweg S, Heise T, tom Dieck H. Improvement of insulin resistance after diet with a whole-grain based dietary product: results of a randomized, controlled cross-over study in obese subjects with elevated fasting blood glucose. Br J Nutr. 2007; 98:929–936. PMID:
17562226.

42. Stancáková A, Civelek M, Saleem NK, Soininen P, Kangas AJ, Cederberg H, Paananen J, Pihlajamäki J, Bonnycastle LL, Morken MA, et al. Hyperglycemia and a common variant of GCKR are associated with the levels of eight amino acids in 9,369 Finnish men. Diabetes. 2012; 61:1895–1902. PMID:
22553379.
43. Butte NF, Liu Y, Zakeri IF, Mohney RP, Mehta N, Voruganti VS, Göring H, Cole SA, Comuzzie AG. Global metabolomic profiling targeting childhood obesity in the Hispanic population. Am J Clin Nutr. 2015; 102:256–267. PMID:
26085512.

44. Newgard CB, An J, Bain JR, Muehlbauer MJ, Stevens RD, Lien LF, Haqq AM, Shah SH, Arlotto M, Slentz CA, et al. A branched-chain amino acid-related metabolic signature that differentiates obese and lean humans and contributes to insulin resistance. Cell Metab. 2009; 9:311–326. PMID:
19356713.

45. Shaham O, Wei R, Wang TJ, Ricciardi C, Lewis GD, Vasan RS, Carr SA, Thadhani R, Gerszten RE, Mootha VK. Metabolic profiling of the human response to a glucose challenge reveals distinct axes of insulin sensitivity. Mol Syst Biol. 2008; 4:214. PMID:
18682704.

46. Huffman KM, Shah SH, Stevens RD, Bain JR, Muehlbauer M, Slentz CA, Tanner CJ, Kuchibhatla M, Houmard JA, Newgard CB, et al. Relationships between circulating metabolic intermediates and insulin action in overweight to obese, inactive men and women. Diabetes Care. 2009; 32:1678–1683. PMID:
19502541.

47. Levitan I, Volkov S, Subbaiah PV. Oxidized LDL: diversity, patterns of recognition, and pathophysiology. Antioxid Redox Signal. 2010; 13:39–75. PMID:
19888833.

48. Yea K, Kim J, Yoon JH, Kwon T, Kim JH, Lee BD, Lee HJ, Lee SJ, Kim JI, Lee TG, et al. Lysophosphatidylcholine activates adipocyte glucose uptake and lowers blood glucose levels in murine models of diabetes. J Biol Chem. 2009; 284:33833–33840. PMID:
19815546.

49. Zhao X, Fritsche J, Wang J, Chen J, Rittig K, Schmitt-Kopplin P, Fritsche A, Häring HU, Schleicher ED, Xu G, et al. Metabonomic fingerprints of fasting plasma and spot urine reveal human pre-diabetic metabolic traits. Metabolomics. 2010; 6:362–374. PMID:
20676218.

50. Tanaka N, Matsubara T, Krausz KW, Patterson AD, Gonzalez FJ. Disruption of phospholipid and bile acid homeostasis in mice with nonalcoholic steatohepatitis. Hepatology. 2012; 56:118–129. PMID:
22290395.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download