1. O'Dell BL, Sunde RA. Handbook of Nutritionally Essential Mineral Elements. Boca Raton (FL): CRC Press;1997.
2. Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Washington, D.C.: National Academies Press;2011.
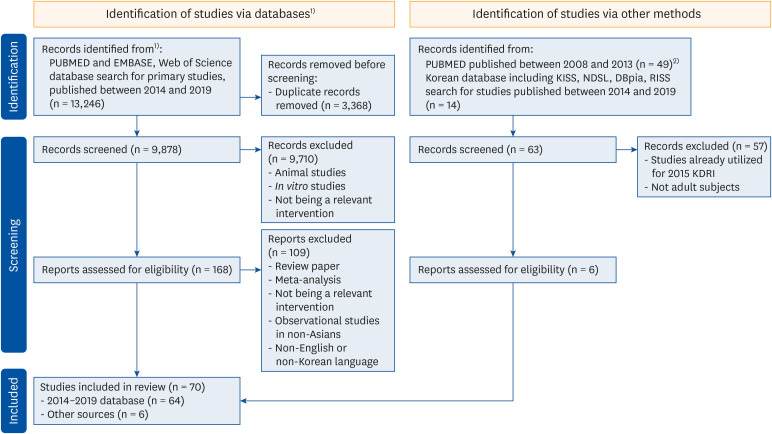
3. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021; 372:n71. PMID:
33782057.
4. Vandenbroucke JP, Von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M; Iniciativa STROBE. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Gac Sanit. 2009; 23:158. PMID:
19249134.
5. Wells G, Shea B, O'connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [Internet]. Ottawa: University of Ottawa;2018. cited 2019 January 5. Available from:
http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
6. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996; 17:1–12. PMID:
8721797.
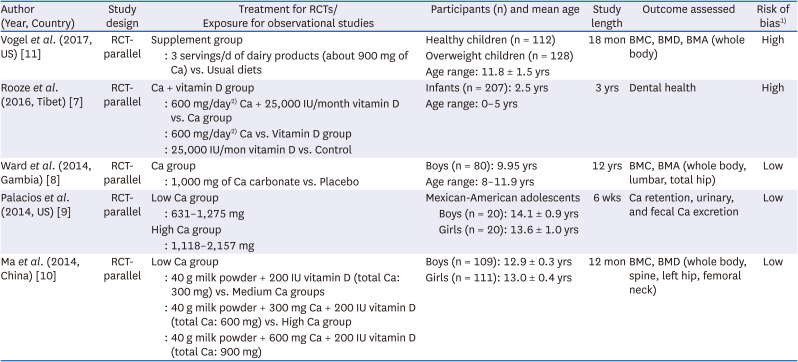
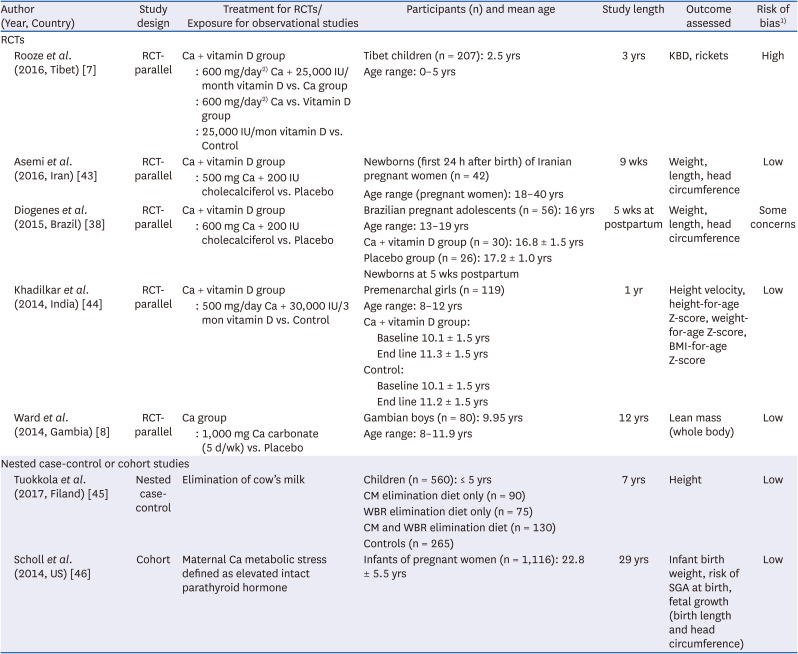
7. Rooze S, Mathieu F, Claus W, Yangzom T, Yangzom D, Goyens P, de Maertelaer V. Effect of calcium and vitamin D on growth, rickets and Kashin-Beck disease in 0- to 5-year-old children in a rural area of central Tibet. Trop Med Int Health. 2016; 21:768–775. PMID:
27102369.
8. Ward KA, Cole TJ, Laskey MA, Ceesay M, Mendy MB, Sawo Y, Prentice A. The effect of prepubertal calcium carbonate supplementation on skeletal development in Gambian boys-a 12-year follow-up study. J Clin Endocrinol Metab. 2014; 99:3169–3176. PMID:
24762110.
9. Palacios C, Martin BR, McCabe GP, McCabe L, Peacock M, Weaver CM. Dietary calcium requirements do not differ between Mexican-American boys and girls. J Nutr. 2014; 144:1167–1173. PMID:
24872223.
10. Ma XM, Huang ZW, Yang XG, Su YX. Calcium supplementation and bone mineral accretion in Chinese adolescents aged 12-14 years: a 12-month, dose-response, randomised intervention trial. Br J Nutr. 2014; 112:1510–1520. PMID:
25231730.
11. Vogel KA, Martin BR, McCabe LD, Peacock M, Warden SJ, McCabe GP, Weaver CM. The effect of dairy intake on bone mass and body composition in early pubertal girls and boys: a randomized controlled trial. Am J Clin Nutr. 2017; 105:1214–1229. PMID:
28330908.
12. Ministry of Health and Welfare (KR). The Korean Nutrition Society. Dietary Reference Intakes for Koreans 2015. Sejong: Ministry of Health and Welfare;2015.
13. Silk LN, Greene DA, Baker MK, Jander CB. Tibial bone responses to 6-month calcium and vitamin D supplementation in young male jockeys: a randomised controlled trial. Bone. 2015; 81:554–561. PMID:
26362226.
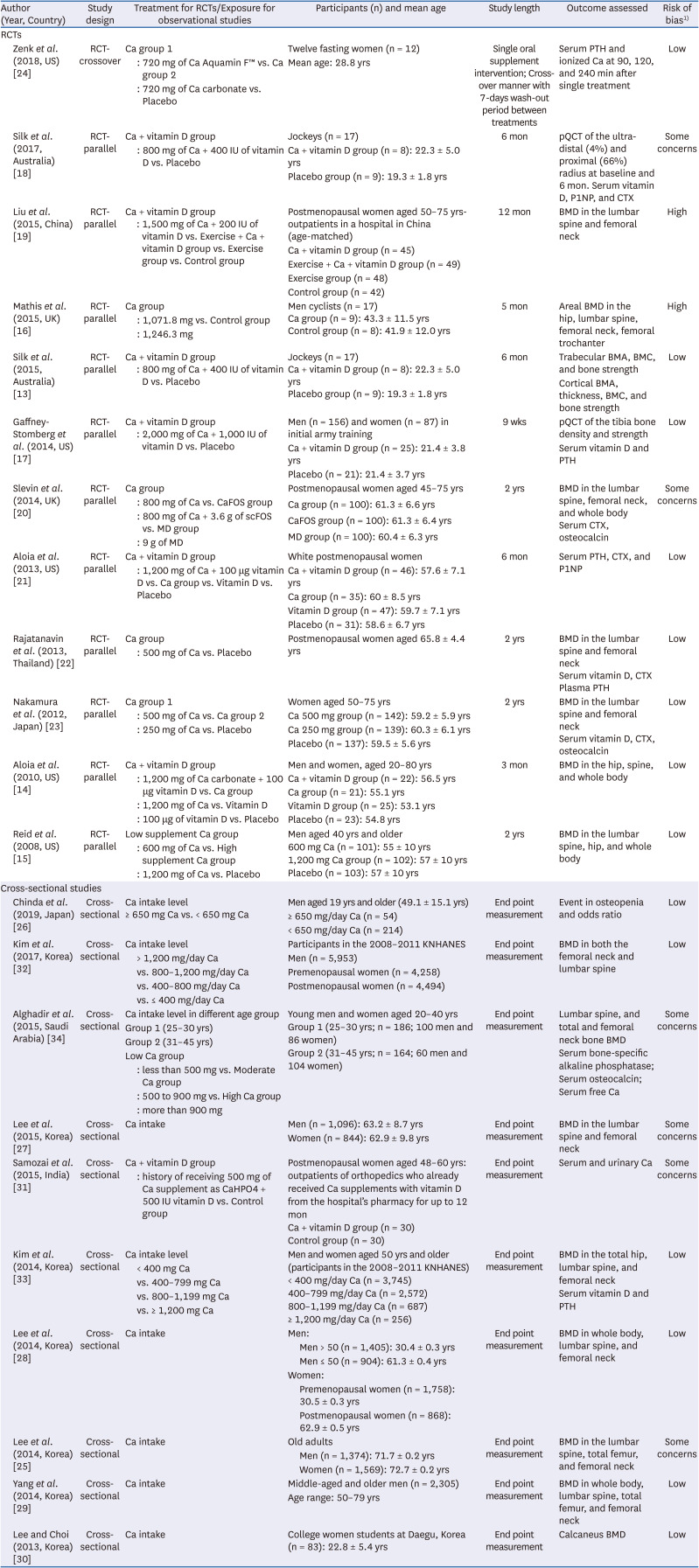
14. Aloia J, Bojadzievski T, Yusupov E, Shahzad G, Pollack S, Mikhail M, Yeh J. The relative influence of calcium intake and vitamin D status on serum parathyroid hormone and bone turnover biomarkers in a double-blind, placebo-controlled parallel group, longitudinal factorial design. J Clin Endocrinol Metab. 2010; 95:3216–3224. PMID:
20463100.
15. Reid IR, Ames R, Mason B, Reid HE, Bacon CJ, Bolland MJ, Gamble GD, Grey A, Horne A. Randomized controlled trial of calcium supplementation in healthy, nonosteoporotic, older men. Arch Intern Med. 2008; 168:2276–2282. PMID:
19001206.
16. Mathis S, Farley RS, Fuller DK, Jetton AE, Ishikawa S, Caputo JL. Effects of a calcium supplement on bone mineral density in male cyclists. J Sports Med Phys Fitness. 2015; 55:940–945. PMID:
26470637.
17. Gaffney-Stomberg E, Lutz LJ, Rood JC, Cable SJ, Pasiakos SM, Young AJ, McClung JP. Calcium and vitamin D supplementation maintains parathyroid hormone and improves bone density during initial military training: a randomized, double-blind, placebo controlled trial. Bone. 2014; 68:46–56. PMID:
25118085.
18. Silk LN, Greene DA, Baker MK, Jander CB. The effect of calcium and vitamin D supplementation on bone health of male Jockeys. J Sci Med Sport. 2017; 20:225–229. PMID:
27568072.
19. Liu BX, Chen SP, Li YD, Wang J, Zhang B, Lin Y, Guan JH, Cai YF, Liang Z, Zheng F. The effect of the modified eighth section of eight-section brocade on osteoporosis in postmenopausal women: a prospective randomized trial. Medicine (Baltimore). 2015; 94:e991. PMID:
26107684.
20. Slevin MM, Allsopp PJ, Magee PJ, Bonham MP, Naughton VR, Strain JJ, Duffy ME, Wallace JM, Mc Sorley EM. Supplementation with calcium and short-chain fructo-oligosaccharides affects markers of bone turnover but not bone mineral density in postmenopausal women. J Nutr. 2014; 144:297–304. PMID:
24453130.
21. Aloia JF, Dhaliwal R, Shieh A, Mikhail M, Islam S, Yeh JK. Calcium and vitamin d supplementation in postmenopausal women. J Clin Endocrinol Metab. 2013; 98:E1702–E1709. PMID:
24064695.
22. Rajatanavin R, Chailurkit L, Saetung S, Thakkinstian A, Nimitphong H. The efficacy of calcium supplementation alone in elderly Thai women over a 2-year period: a randomized controlled trial. Osteoporos Int. 2013; 24:2871–2877. PMID:
23681085.
23. Nakamura K, Saito T, Kobayashi R, Oshiki R, Kitamura K, Oyama M, Narisawa S, Nashimoto M, Takahashi S, Takachi R. Effect of low-dose calcium supplements on bone loss in perimenopausal and postmenopausal Asian women: a randomized controlled trial. J Bone Miner Res. 2012; 27:2264–2270. PMID:
22653713.
24. Zenk JL, Frestedt JL, Kuskowski MA. Effect of calcium derived from
Lithothamnion sp. on markers of calcium metabolism in premenopausal women. J Med Food. 2018; 21:154–158. PMID:
29023178.
25. Lee KS, Jang JS, Lee DR, Kim YH, Nam GE, Han BD, Han KD, Cho KH, Kim SM, Choi YS, et al. Serum ferritin levels are positively associated with bone mineral density in elderly Korean men: the 2008-2010 Korea National Health and Nutrition Examination Surveys. J Bone Miner Metab. 2014; 32:683–690. PMID:
24337956.
26. Chinda D, Shimoyama T, Sawada K, Iino C, Sakuraba H, Nakaji S, Fukuda S. Lifestyle factors rather than Helicobacter pylori infection or estradiol level are associated with osteopenia in Japanese men. Am J Men Health. 2019; 13:1557988319848219.
27. Lee KM, Kwon SS, Chung CY, Lee SY, Kim TG, Choi Y, Park MS. Gender- and body-site-specific factors associated with bone mineral density in a non-institutionalized Korean population aged ≥50 years. J Bone Miner Metab. 2015; 33:401–409. PMID:
25001078.
28. Lee KJ, Kim KS, Kim HN, Seo JA, Song SW. Association between dietary calcium and phosphorus intakes, dietary calcium/phosphorus ratio and bone mass in the Korean population. Nutr J. 2014; 13:114. PMID:
25496564.
29. Yang YJ, Kim J. Factors in relation to bone mineral density in Korean middle-aged and older men: 2008-2010 Korea National Health and Nutrition Examination Survey. Ann Nutr Metab. 2014; 64:50–59. PMID:
24851837.
30. Lee JW, Choi MJ. Nutrition, food habit, and bone mineral density in young college females. Osteoporosis. 2013; 11:81–88.
31. Samozai MN, Kulkarni AK. Do calcium supplements increase serum and urine calcium levels in post-menopausal women? J Nutr Health Aging. 2015; 19:537–541. PMID:
25923483.
32. Kim MK, Chon SJ, Noe EB, Roh YH, Yun BH, Cho S, Choi YS, Lee BS, Seo SK. Associations of dietary calcium intake with metabolic syndrome and bone mineral density among the Korean population: KNHANES 2008-2011. Osteoporos Int. 2017; 28:299–308. PMID:
27503170.
33. Kim KM, Choi SH, Lim S, Moon JH, Kim JH, Kim SW, Jang HC, Shin CS. Interactions between dietary calcium intake and bone mineral density or bone geometry in a low calcium intake population (KNHANES IV 2008-2010). J Clin Endocrinol Metab. 2014; 99:2409–2417. PMID:
24684465.
34. Alghadir AH, Gabr SA, Al-Eisa E. Physical activity and lifestyle effects on bone mineral density among young adults: sociodemographic and biochemical analysis. J Phys Ther Sci. 2015; 27:2261–2270. PMID:
26311965.
35. Kim KM, Choi HS, Choi MJ, Chung HY. Calcium and vitamin D supplementations: 2015 position statement of the Korean Society for Bone and Mineral Research. J Bone Metab. 2015; 22:143–149. PMID:
26713305.
36. Joo NS, Dawson-Hughes B, Kim YS, Oh K, Yeum KJ. Impact of calcium and vitamin D insufficiencies on serum parathyroid hormone and bone mineral density: analysis of the fourth and fifth Korea National Health and Nutrition Examination Survey (KNHANES IV-3, 2009 and KNHANES V-1, 2010). J Bone Miner Res. 2013; 28:764–770. PMID:
23045165.
37. Uenishi K, Ishida H, Kamei A, Shiraki M, Ezawa I, Goto S, Fukuoka H, Hosoi T, Orimo H. Calcium requirement estimated by balance study in elderly Japanese people. Osteoporos Int. 2001; 12:858–863. PMID:
11716189.
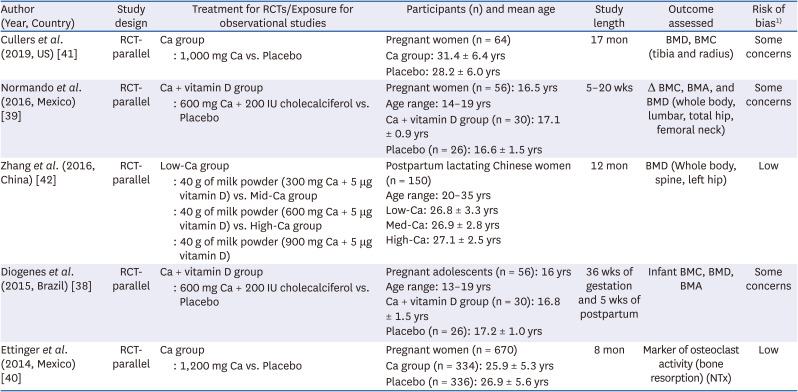
38. Diogenes ME, Bezerra FF, Rezende EP, Donangelo CM. Calcium plus vitamin D supplementation during the third trimester of pregnancy in adolescents accustomed to low calcium diets does not affect infant bone mass at early lactation in a randomized controlled trial. J Nutr. 2015; 145:1515–1523. PMID:
26019245.
39. Normando P, Diogenes ME, Cabello PH, Cabello GM, Donangelo CM, Bezerra FF. Calcium plus vitamin D supplementation during pregnancy interacts with polymorphisms in the promoter region of the VDR gene to affect postpartum bone mass of Brazilian adolescent mothers: a randomized controlled trial. Nutrition. 2016; 32:1068–1074. PMID:
27211082.
40. Ettinger AS, Lamadrid-Figueroa H, Mercado-García A, Kordas K, Wood RJ, Peterson KE, Hu H, Hernández-Avila M, Téllez-Rojo MM. Effect of calcium supplementation on bone resorption in pregnancy and the early postpartum: a randomized controlled trial in Mexican women. Nutr J. 2014; 13:116. PMID:
25511814.
41. Cullers A, King JC, Van Loan M, Gildengorin G, Fung EB. Effect of prenatal calcium supplementation on bone during pregnancy and 1 y postpartum. Am J Clin Nutr. 2019; 109:197–206. PMID:
30649176.
42. Zhang ZQ, Chen YM, Wang RQ, Huang ZW, Yang XG, Su YX. The effects of different levels of calcium supplementation on the bone mineral status of postpartum lactating Chinese women: a 12-month randomised, double-blinded, controlled trial. Br J Nutr. 2016; 115:24–31. PMID:
26522081.
43. Asemi Z, Samimi M, Siavashani MA, Mazloomi M, Tabassi Z, Karamali M, Jamilian M, Esmaillzadeh A. Calcium-vitamin D co-supplementation affects metabolic profiles, but not pregnancy outcomes, in healthy pregnant women. Int J Prev Med. 2016; 7:49. PMID:
27076887.
44. Khadilkar AV, Kadam NS, Chiplonkar SA, Khadilkar VV. Effect of micronutrient supplementation on height velocity of underprivileged girls in comparison with un-supplemented healthy controls. J Pediatr Endocrinol Metab. 2014; 27:245–252. PMID:
24150200.
45. Tuokkola J, Luukkainen P, Nevalainen J, Ahonen S, Toppari J, Ilonen J, Veijola R, Knip M, Virtanen SM, Kaila M. Eliminating cows’ milk, but not wheat, barley or rye, increases the risk of growth deceleration and nutritional inadequacies. Acta Paediatr. 2017; 106:1142–1149. PMID:
28345135.
46. Scholl TO, Chen X, Stein TP. Maternal calcium metabolic stress and fetal growth. Am J Clin Nutr. 2014; 99:918–925. PMID:
24500145.
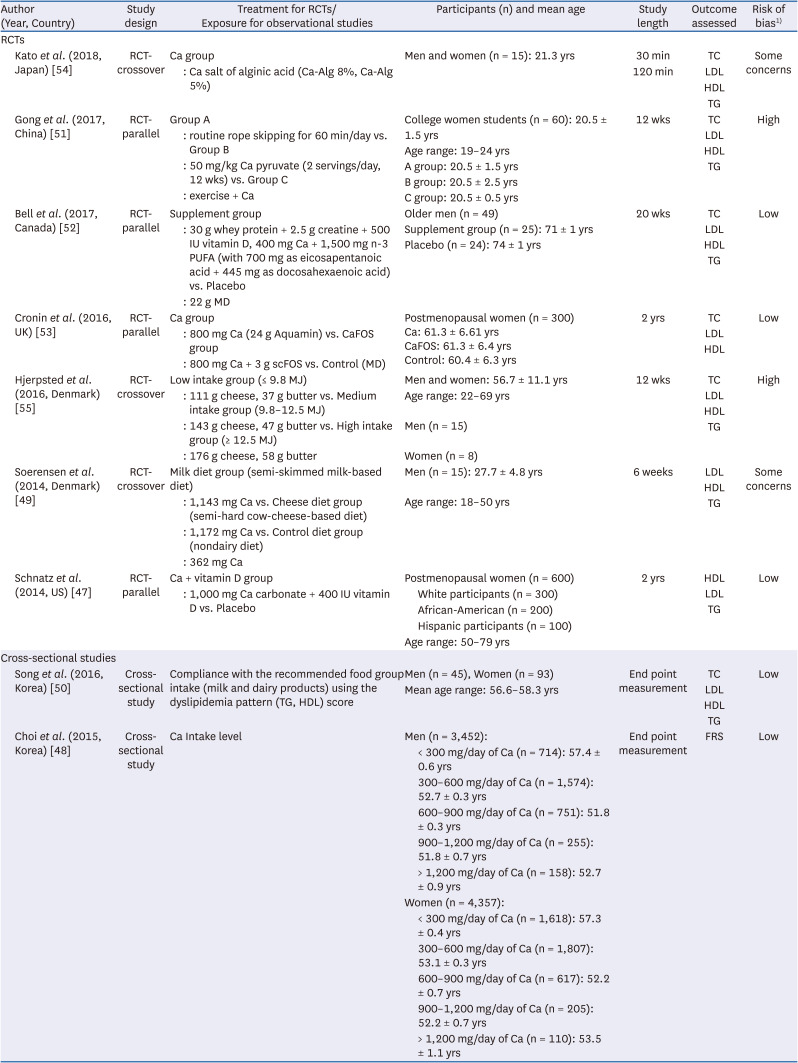
47. Schnatz PF, Jiang X, Vila-Wright S, Aragaki AK, Nudy M, O’Sullivan DM, Jackson R, LeBlanc E, Robinson JG, Shikany JM, et al. Calcium/vitamin D supplementation, serum 25-hydroxyvitamin D concentrations, and cholesterol profiles in the Women’s Health Initiative calcium/vitamin D randomized trial. Menopause. 2014; 21:823–833. PMID:
24594863.
48. Choi SJ, Yeum KJ, Park SJ, Choi B, Joo NS. Dietary calcium and Framingham Risk Score in vitamin D deficient male (KNHANES 2009-2011). Yonsei Med J. 2015; 56:845–852. PMID:
25837195.
49. Soerensen KV, Thorning TK, Astrup A, Kristensen M, Lorenzen JK. Effect of dairy calcium from cheese and milk on fecal fat excretion, blood lipids, and appetite in young men. Am J Clin Nutr. 2014; 99:984–991. PMID:
24622806.
50. Song S, Paik HY, Park M, Song Y. Dyslipidemia patterns are differentially associated with dietary factors. Clin Nutr. 2016; 35:885–891. PMID:
26140958.
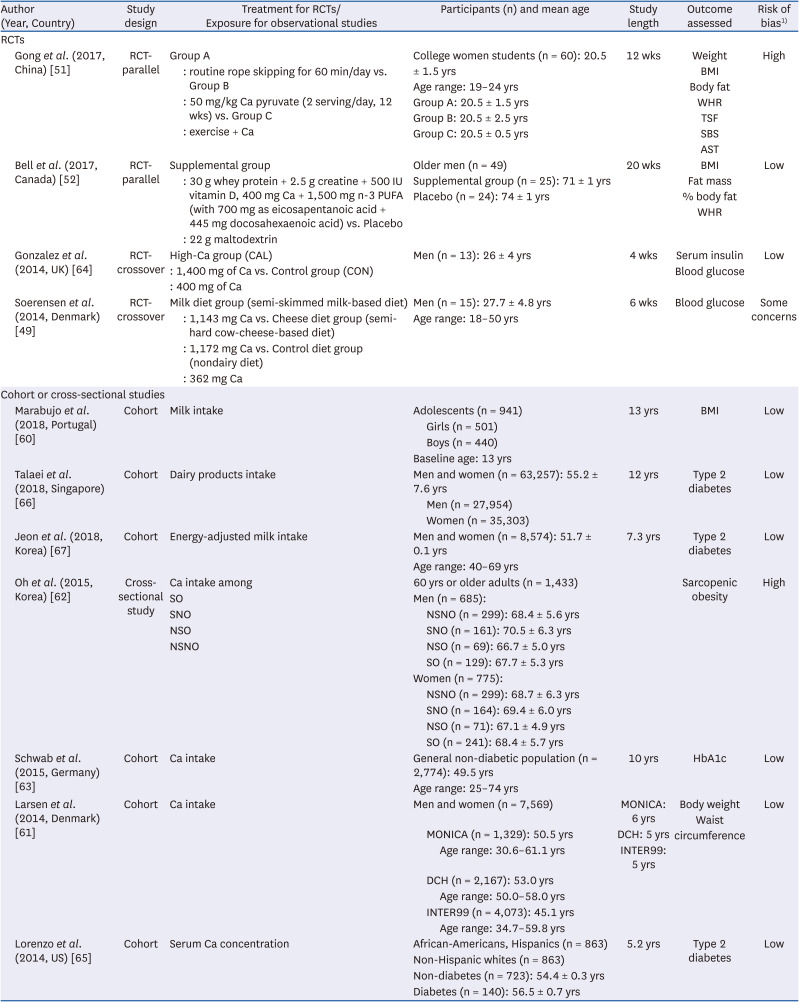
51. Gong W, Jiang J. Effect of rope skipping combining calcium pyruvate on fat metabolism of female college students. Biomed Res (Aligarh). 2018; S333–S336.
52. Bell KE, Snijders T, Zulyniak M, Kumbhare D, Parise G, Chabowski A, Phillips SM. A whey protein-based multi-ingredient nutritional supplement stimulates gains in lean body mass and strength in healthy older men: a randomized controlled trial. PLoS One. 2017; 12:e0181387. PMID:
28719669.
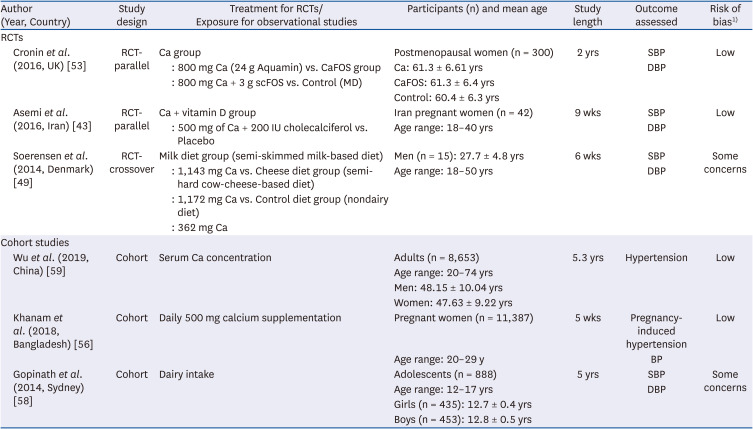
53. Cronin BE, Allsopp PJ, Slevin MM, Magee PJ, Livingstone MB, Strain JJ, McSorley EM. Effects of supplementation with a calcium-rich marine-derived multi-mineral supplement and short-chain fructo-oligosaccharides on serum lipids in postmenopausal women. Br J Nutr. 2016; 115:658–665. PMID:
26669430.
54. Kato T, Idota Y, Shiragami K, Koike M, Nishibori F, Tomokane M, Seki T, Itabashi K, Hakoda K, Takahashi H, et al. Randomized, double-blind, crossover clinical trial of the effect of calcium alginate in noodles on postprandial blood glucose level. Biol Pharm Bull. 2018; 41:1367–1371. PMID:
29973437.
55. Hjerpsted JB, Dragsted LO, Tholstrup T. Cheese intake lowers plasma cholesterol concentrations without increasing bile acid excretion. J Nutr Intermed Metab. 2016; 3:12–17.
56. Khanam F, Hossain B, Mistry SK, Mitra DK, Raza WA, Rifat M, Afsana K, Rahman M. The association between daily 500 mg calcium supplementation and lower pregnancy-induced hypertension risk in Bangladesh. BMC Pregnancy Childbirth. 2018; 18:406. PMID:
30332997.
57. Liu Z, Fang A, He J, Shen X, Gao R, Zhao X, Li K. Association of habitually low intake of dietary calcium with blood pressure and hypertension in a population with predominantly plant-based diets. Nutrients. 2018; 10:603.
58. Gopinath B, Flood VM, Burlutsky G, Louie JC, Baur LA, Mitchell P. Dairy food consumption, blood pressure and retinal microcirculation in adolescents. Nutr Metab Cardiovasc Dis. 2014; 24:1221–1227. PMID:
24996501.
59. Wu X, Han T, Gao J, Zhang Y, Zhao S, Sun R, Sun C, Niu Y, Li Y. Association of serum calcium and insulin resistance with hypertension risk: a prospective population-based study. J Am Heart Assoc. 2019; 8:e009585. PMID:
30596304.
60. Marabujo T, Ramos E, Lopes C. Dairy products and total calcium intake at 13 years of age and its association with obesity at 21 years of age. Eur J Clin Nutr. 2018; 72:541–547. PMID:
29371641.
61. Larsen SC, Ängquist L, Ahluwalia TS, Skaaby T, Roswall N, Tjønneland A, Halkjær J, Overvad K, Pedersen O, Hansen T, et al. Interaction between genetic predisposition to obesity and dietary calcium in relation to subsequent change in body weight and waist circumference. Am J Clin Nutr. 2014; 99:957–965. PMID:
24500147.
62. Oh C, Jho S, No JK, Kim HS. Body composition changes were related to nutrient intakes in elderly men but elderly women had a higher prevalence of sarcopenic obesity in a population of Korean adults. Nutr Res. 2015; 35:1–6. PMID:
25524331.
63. Schwab S, Zierer A, Heier M, Fischer B, Huth C, Baumert J, Meisinger C, Peters A, Thorand B. Intake of vitamin and mineral supplements and longitudinal association with HbA1c levels in the general non-diabetic population--results from the MONICA/KORA S3/F3 study. PLoS One. 2015; 10:e0139244. PMID:
26473975.
64. Gonzalez JT, Green BP, Campbell MD, Rumbold PL, Stevenson EJ. The influence of calcium supplementation on substrate metabolism during exercise in humans: a randomized controlled trial. Eur J Clin Nutr. 2014; 68:712–718. PMID:
24642785.
65. Lorenzo C, Hanley AJ, Rewers MJ, Haffner SM. Calcium and phosphate concentrations and future development of type 2 diabetes: the Insulin Resistance Atherosclerosis Study. Diabetologia. 2014; 57:1366–1374. PMID:
24763850.
66. Talaei M, Pan A, Yuan JM, Koh WP. Dairy intake and risk of type 2 diabetes. Clin Nutr. 2018; 37:712–718. PMID:
28318689.
67. Jeon J, Jang J, Park K. Effects of consuming calcium-rich foods on the incidence of type 2 diabetes mellitus. Nutrients. 2018; 11:31.
68. Korea Centers for Disease Control and Prevention. Report Presentation of the Korea National Health and Nutrition Examination Survey (KNHANES) VI: 2013–2015. Sejong: Korea Centers for Disease Control and Prevention;2015.
69. Korea Centers for Disease Control and Prevention. Report Presentation of the Korea National Health and Nutrition Examination Survey (KNHANES) VII: 2016–2017. Sejong: Korea Centers for Disease Control and Prevention;2017.
70. Calvo MS, Moshfegh AJ, Tucker KL. Assessing the health impact of phosphorus in the food supply: issues and considerations. Adv Nutr. 2014; 5:104–113. PMID:
24425729.
71. Kim M, Yoon J. Estimation of usual intake and assessment of nutrient intake for Korean adolescents: analysis of the 2010-2012 Korea National Health and Nutrition Examination Survey. Fam Environ Res. 2017; 55:385–397.
72. Park JH, Hong IY, Chung JW, Choi HS. Vitamin D status in South Korean population: seven-year trend from the KNHANES. Medicine (Baltimore). 2018; 97:e11032. PMID:
29952942.
73. Vatanparast H, Bailey DA, Baxter-Jones AD, Whiting SJ. Calcium requirements for bone growth in Canadian boys and girls during adolescence. Br J Nutr. 2010; 103:575–580. PMID:
19852873.
74. Wu L, Martin BR, Braun MM, Wastney ME, McCabe GP, McCabe LD, DiMeglio LA, Peacock M, Weaver CM. Calcium requirements and metabolism in Chinese-American boys and girls. J Bone Miner Res. 2010; 25:1842–1849. PMID:
20205166.
75. Diogenes ME, Bezerra FF, Rezende EP, Taveira MF, Pinhal I, Donangelo CM. Effect of calcium plus vitamin D supplementation during pregnancy in Brazilian adolescent mothers: a randomized, placebo-controlled trial. Am J Clin Nutr. 2013; 98:82–91. PMID:
23719547.
76. Ward KA, Jarjou L, Prentice A. Long-term effects of maternal calcium supplementation on childhood growth differ between males and females in a population accustomed to a low calcium intake. Bone. 2017; 103:31–38. PMID:
28583879.
77. Abdel-Aleem H, Merialdi M, Elsnosy ED, Elsedfy GO, Abdel-Aleem MA, Villar J. The effect of calcium supplementation during pregnancy on fetal and infant growth: a nested randomized controlled trial within WHO calcium supplementation trial. J Matern Fetal Neonatal Med. 2009; 22:94–100. PMID:
19085634.
78. Koo WW, Walters JC, Esterlitz J, Levine RJ, Bush AJ, Sibai B. Maternal calcium supplementation and fetal bone mineralization. Obstet Gynecol. 1999; 94:577–582. PMID:
10511362.
79. Young BE, McNanley TJ, Cooper EM, McIntyre AW, Witter F, Harris ZL, O’Brien KO. Maternal vitamin D status and calcium intake interact to affect fetal skeletal growth in utero in pregnant adolescents. Am J Clin Nutr. 2012; 95:1103–1112. PMID:
22492380.
80. Hwang IR, Choi YK, Lee WK, Kim JG, Lee IK, Kim SW, Park KG. Association between prolonged breastfeeding and bone mineral density and osteoporosis in postmenopausal women: KNHANES 2010-2011. Osteoporos Int. 2016; 27:257–265. PMID:
26373982.
81. Jarjou LM, Laskey MA, Sawo Y, Goldberg GR, Cole TJ, Prentice A. Effect of calcium supplementation in pregnancy on maternal bone outcomes in women with a low calcium intake. Am J Clin Nutr. 2010; 92:450–457. PMID:
20554790.
82. Jarjou LM, Sawo Y, Goldberg GR, Laskey MA, Cole TJ, Prentice A. Unexpected long-term effects of calcium supplementation in pregnancy on maternal bone outcomes in women with a low calcium intake: a follow-up study. Am J Clin Nutr. 2013; 98:723–730. PMID:
23902782.
83. Liu Z, Qiu L, Chen YM, Su YX. Effect of milk and calcium supplementation on bone density and bone turnover in pregnant Chinese women: a randomized controlled trail. Arch Gynecol Obstet. 2011; 283:205–211. PMID:
20044757.
84. Bjørnerem Å, Ghasem-Zadeh A, Wang X, Bui M, Walker SP, Zebaze R, Seeman E. Irreversible deterioration of cortical and trabecular microstructure associated with breastfeeding. J Bone Miner Res. 2017; 32:681–687. PMID:
27736021.
85. National Institutes of Health (US). All of Us Research Program [Internet]. Bethesda (MD): National Institutes of Health;2021. cited 2021 October 7. Available from:
https://allofus.nih.gov/.
86. Lee KH, Choi IS, Oh SH. A study on intake/excretion of sodium and calcium in Korean children. Korean J Nutr. 1995; 28:749–758.
87. Park CY, Hill KM, Elble AE, Martin BR, DiMeglio LA, Peacock M, McCabe GP, Weaver CM. Daily supplementation with 25 μg cholecalciferol does not increase calcium absorption or skeletal retention in adolescent girls with low serum 25-hydroxyvitamin D. J Nutr. 2010; 140:2139–2144. PMID:
20962148.
88. Shin JH, Bauer S, Yoon YS, Jeong HC, Rhie YJ, Lee JH, Woo CW, Choi BM, Kim HJ, Park SH, et al. Obstetric and neonatal outcomes of the teenage pregnancy. J Korean Soc Neonatol. 2010; 17:94–101.
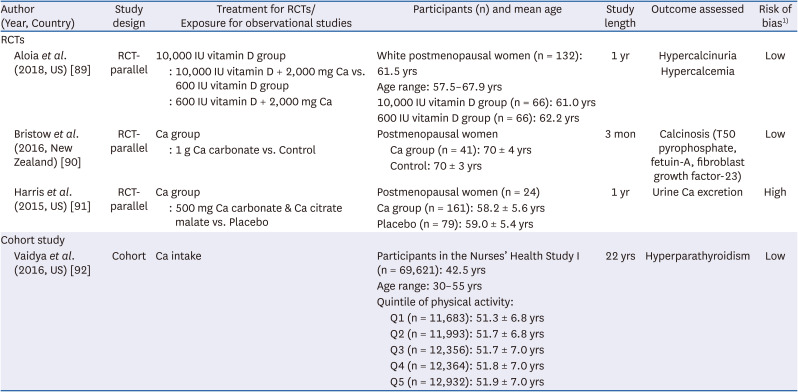
89. Aloia JF, Katumuluwa S, Stolberg A, Usera G, Mikhail M, Hoofnagle AN, Islam S. Safety of calcium and vitamin D supplements, a randomized controlled trial. Clin Endocrinol (Oxf). 2018; 89:742–749. PMID:
30180273.
90. Bristow SM, Gamble GD, Pasch A, O’Neill WC, Stewart A, Horne AM, Reid IR. Acute and 3-month effects of calcium carbonate on the calcification propensity of serum and regulators of vascular calcification: secondary analysis of a randomized controlled trial. Osteoporos Int. 2016; 27:1209–1216. PMID:
26493812.
91. Harris SS, Dawson-Hughes B. Effects of hydration and calcium supplementation on urine calcium concentration in healthy postmenopausal women. J Am Coll Nutr. 2015; 34:340–346. PMID:
25856469.
92. Vaidya A, Curhan GC, Paik JM, Wang M, Taylor EN. Physical activity and the risk of primary hyperparathyroidism. J Clin Endocrinol Metab. 2016; 101:1590–1597. PMID:
26812691.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download