INTRODUCTION
Stroke is a highly devastating disease that is the second most common cause of death worldwide.
1 In the United States in 2011, stroke-related deaths accounted for approximately 5% of all deaths and occurred every four minutes, on average.
2 There is ample evidence that some patients with acute stroke who timely receive reperfusion treatment or endovascular thrombectomy earlier have less disability and better survival rates. Therefore, early treatment is highly important for patients with acute stroke.
3
In acute stroke treatment, emergency medical services (EMS) usage associated with a significant reduction in pre-hospital delays and the increased likelihood of patients to receive timely treatment.
4 EMS usage is also associated with a significant reduction in in-hospital delays by facilitating the hospital stroke team’s immediate response, resulting in timely assessment and more rapid neuroimaging.
567 EMS plays an essential role in achieving early reperfusion treatment or endovascular thrombectomy for patients with acute stroke.
However, the sudden outbreak of an infectious disease such as the coronavirus disease 2019 (COVID-19) could adversely affect acute stroke treatment. A significant decline in the number of patients with acute stroke was observed in the emergency departments (ED) of France, Germany, and Italy.
8 According to national stroke data in China, the total number of thrombolysis and thrombectomy cases in February of 2020 decreased by 26.7% and 25.3%, respectively, as compared with February of 2019.
9 Similar trends were also observed in France. In March of 2020, thrombolysis and thrombectomy decreased by 40.9% and 27.6%, respectively, compared to the same period in 2019.
10
Few studies have investigated the impact of the sudden outbreak of COVID-19 on EMS response for acute stroke. This study analyzed the changes in EMS response for acute stroke that occurred in a large metropolitan city during the chaotic period following the sudden outbreak of COVID-19.
METHODS
Study sample
This study was conducted at 25 safety centers of five fire stations in Seoul, Korea, a metropolitan city with a population of 9.99 million. In Korea, firefighting and EMS are provided only by the government and not by private organizations. The safety center is a government agency that is affiliated with the fire stations and performs firefighting, EMS, and related administrative tasks in each area. The fire stations selected were the top five based on the number of dispatches, out of a total of 24 fire stations in Seoul. The total population of the area under the jurisdiction of the five fire stations is 2.36 million, which is 23.1% of the total population of Seoul. In 2019, 25 Safety Centers received a total of 147,112 requests to dispatch an ambulance, which is 27.6% of the total requests in Seoul. Of them, 92,759 (63.1%) were transported to a hospital.
In Korea, an average of about 9,800 patients are treated for acute stroke each year. Of them, ischemic stroke is 76%, intracerebral hemorrhage is 15%, and subarachnoid hemorrhage is 9%. EMS were used in 56% of cases, and the median interval from symptoms onset to hospital arrival was 4.5 hours. The intravenous thrombolysis and endovascular therapy rates were 11% and 4%, respectively. The 26% of patients are admitted to an intensive care unit (ICU).
11
Study design
This was a comparative cross-sectional study of data obtained from the Rescue and Emergency Activities Information System. The Rescue and Emergency Activities Information System is a prospective nationwide data registry operated by the government (National Fire Agency) in accordance with Korean laws (Article 22, Paragraph 2 of the Act on 119 Rescue and Emergency Medical Services and Article 15 of the Emergency Medical Service Act).
The Rescue and Emergency Activities Information System is created by merging data: the Daily Record of the Emergency Medical Services (hereafter referred to as an EMS record), the in-depth EMS report of cardiac arrest, the in-depth EMS report of severe trauma, the in-depth EMS report of suspected acute cardiovascular disease, the in-depth EMS report of suspected acute cerebrovascular disease, diagnosis and clinical outcomes of patients who were transported to the ED using EMS provided by the Ministry of Health and Welfare through the National Emergency Department Information System (NEDIS), and administrative documents.
EMS record, in-depth EMS report of suspected acute cerebrovascular disease, and NEDIS data were used in the study. The in-depth EMS report of suspected acute cerebrovascular disease is an EMS record additionally prepared by the emergency medical technician (EMT) when a patient has one or more of the following symptoms: headache, dizziness, loss of consciousness, convulsions, seizures, syncope, paralysis, and other symptoms related to the cerebrovascular disease (excluding symptoms caused by trauma). The in-depth EMS report of suspected acute cerebrovascular disease additionally records the situation when symptoms onset, the results of the stroke screening test, the history of previous stroke, and any contraindications for the intravenous thrombolysis. NEDIS is a nationwide information network operated by the government (Ministry of Health and Welfare) that includes administrative and clinical data for patients who have visited ED.
12
The study was conducted from February 1 to April 30, 2020. The control period was from February 1 to April 30, 2019. For reference, the first occurrence of a patient with COVID-19 in Seoul was January 24, 2020, and by the end of January, a total of six patients had been diagnosed with COVID-19 in the Seoul metropolitan area. From February 2020 on, all paramedics and medical professionals in Seoul had to comply with new guidelines for COVID-19 outbreak.
Patients included in the study requested an EMS dispatch due to neurological symptoms of cerebrovascular disease, were positive on the Los Angeles Prehospital Stroke Screen (LAPSS) as assessed by the EMT, were transported to the ED using EMS, admitted to the general ward or ICU, and had a final diagnosis of acute stroke.
13 A final diagnosis of acute stroke was investigated based on NEDIS data in the Rescue and Emergency Activities Information System.
Patients were excluded if they were refused stroke treatment against medical advice, were transferred to other hospitals before stroke evaluation was complete, or had missing data. Owing to the cross-sectional study design, we included only data from the first visit for patients who made multiple visits within the study period, regardless of the total number of visits.
Patients were divided into two groups, pre-COVID-19 period and early-COVID-19 period, based on EMS records. The variables used for comparative analysis were the clinical characteristics, stroke symptom, characteristics of EMS response, characteristic of stroke treatment, and clinical outcomes.
Clinical characteristics included sex, age, initial vital signs, initial blood sugar levels, final diagnosis, and history of disease. Initial vital signs included systolic blood pressure and heart rate. The final diagnosis was defined as an ischemic stroke or a hemorrhagic stroke with reference to be the patient's diagnosis upon ED discharge. History of disease included hypertension, diabetes mellitus, and previous cerebrovascular disease.
Stroke symptoms included initial mental state, the three signs (facial droop, arm drift, and abnormal speech) used in the prehospital evaluation of stroke, the prehospital evaluation of stroke score, a clear onset time, and occurrence of wake-up strokes. Initial mental states were evaluated based on an alert/verbal/painful/unresponsive responsiveness scale.
14 Pre-hospital evaluation of stroke was performed using the Cincinnati Prehospital Stroke Scale.
15
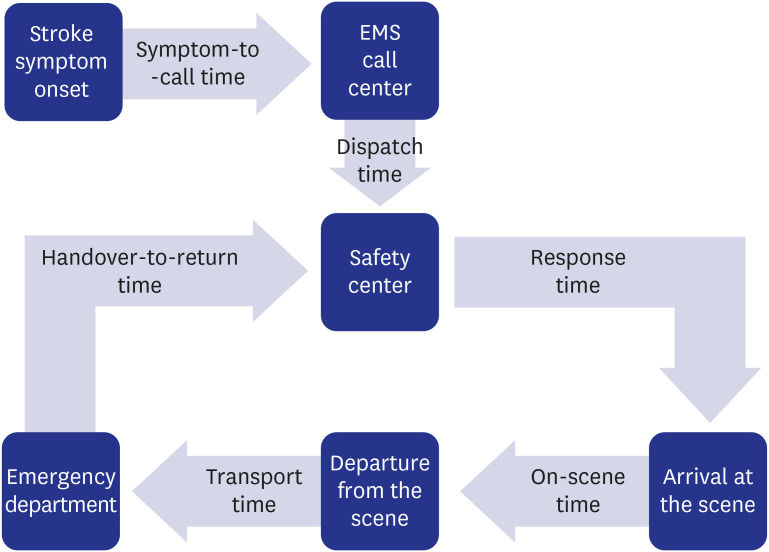
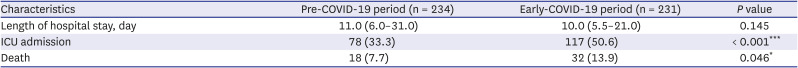
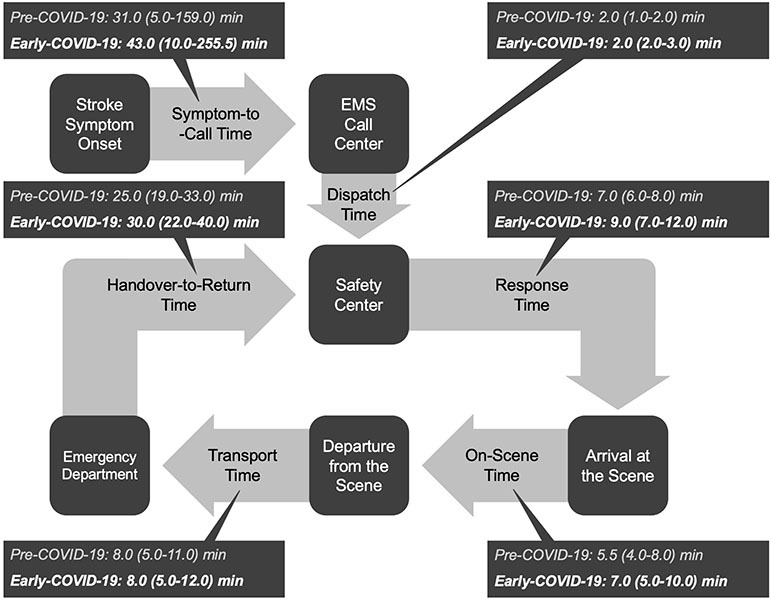
Characteristics of EMS responses were the EMS response time and EMS response distance. We calculated the time between each component of total EMS response time, which was defined as follows (
Fig. 1). When the exact time of symptoms onset was unknown by a patient, it was defined as the time at which the patient first noticed a neurological abnormality. Also, if the patient’s stroke symptoms were recognized by others, that was defined as the time when someone first recognized a patient’s neurological abnormalities. For patients whose symptom onset time was unclear, symptoms-to-call time was calculated according to the above criteria. EMS distance was the distance from the safety center to the scene and the distance from the scene to the hospital.
Fig. 1
Definition of the time between each prehospital time component.
EMS = emergency medical services.

Characteristic of stroke treatment included onset-to-door time, ED length of stay, surgery, and endovascular treatment. Onset-to-door time was classified as within 4.5 hours or later. The criteria for the 4.5 hours classifications were the same as guidelines for the early management of acute ischemic stroke.
3 Clinical outcomes of acute stroke included length of hospital stay, admission to ICU, and death. Death was defined as in-hospital mortality after occurrence of stroke event.
Statistical analysis
Statistical analyses were performed with SPSS Statistics for Windows, Version 18.0 (IBM Corp., Armonk, NY, USA). Patients were divided into two groups, pre-COVID-19 period and early-COVID-19 period, and previously collected patient data were analyzed. We performed comparative analyses of EMS response and clinical outcomes between the groups. We used the χ2 test, independent variable t-test, and Mann-Whitney U test to analyze the difference between the two groups. Statistical significance was defined for P values of less than 0.05.
We performed a subgroup analysis of patients with pre-hospital delay. Pre-hospital delay was classified based on total EMS response time. For each period, patients above the 75th percentile of total EMS response time were included in subgroup analysis. We used the Mann-Whitney U test to analyze the difference between the two groups. Statistical significance was defined for P values of less than 0.05.
We performed logistic regression analyses to evaluate factors associated with ICU admission for patients with acute stroke. COVID-19 outbreak and risk factors for stroke (age, sex, type of stroke, history of disease, initial mental state) were compared between patients admitted to ICU and patients admitted to general wards. Factors with significant differences between the two groups were used as variables in the regression model. We also performed logistic regression analyses to evaluate factors associated with in-hospital mortality for patients with acute stroke. Factors with significant differences between patients who were discharged alive and patients who experienced in-hospital mortality were used as variables in the regression model. Statistical significance was defined for P values of less than 0.05.
Ethics statement
The data collected were used for study purposes only. This study was approved by the Institutional Review Board of The Catholic University of Korea Catholic Medical Center, where the study was conducted (approval number was OC21EASI0004). Because this study was a retrospective chart review, informed consent was waived by the review board.
RESULTS
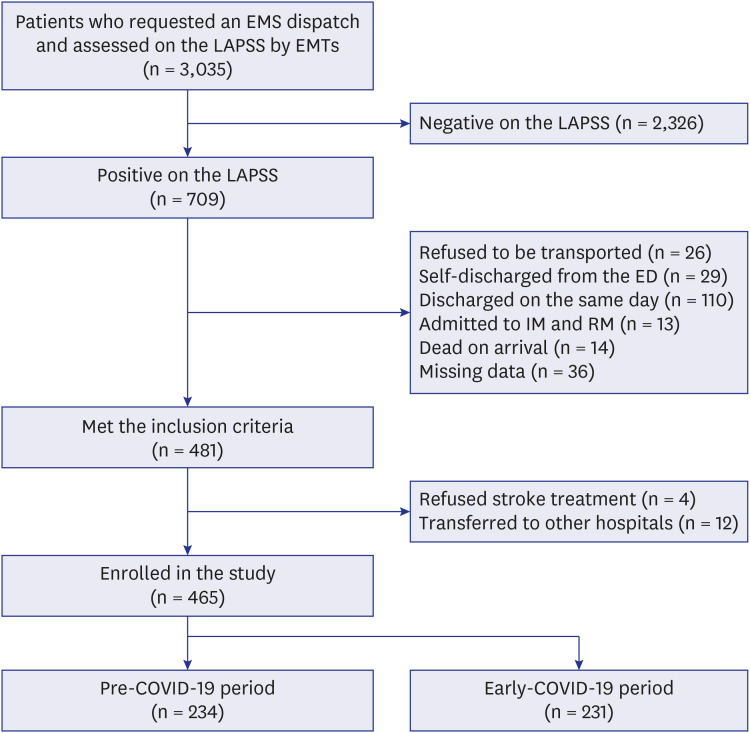
A total of 3,035 patients were assessed on the LAPSS by EMTs, of which 709 (23.4%) were positive. Of the 709 LAPSS-positive patients, 495 met the inclusion criteria, excluding 26 patients who refused to be transported to the ED, 29 patients who were self-discharged from the ED against medical advice, 110 patients who were discharged from the ED on the same day with spontaneous improvement of symptoms, 13 patients who were admitted to departments other than neurology and neurosurgery, 14 patients who were dead on arrival, and 36 patients with missing data. Of the 481 patients who met the inclusion criteria, four patients refused stroke treatment against medical advice, and 12 patients were transferred to other hospitals before stroke evaluation was complete. Thus, 465 patients were enrolled in the study (
Fig. 2).
Fig. 2
Flow diagram of included patients.
EMS = emergency medical services, LAPSS = Los Angeles Prehospital Stroke Screen, EMT = emergency medical technician, ED = emergency departments, IM = internal medicine, RM = rehabilitation medicine, COVID-19 = coronavirus disease 2019.
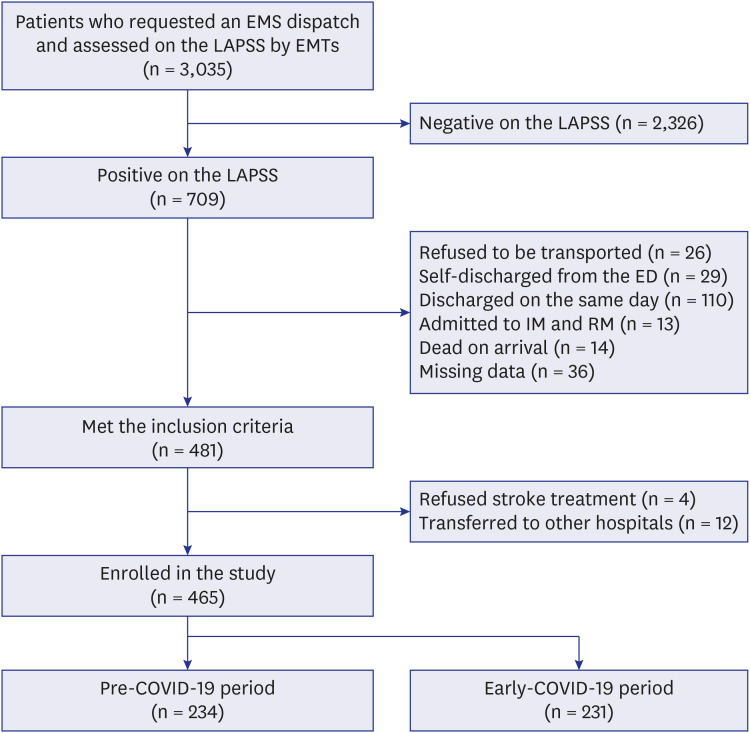

Of the 465 enrolled patients, 231 (49.7%) were in the early-COVID-19 period, and 234 (50.3%) were in the pre-COVID-19 period. Despite the COVID-19 outbreak, there was no significant difference in the number of patients with acute stroke who used EMS. Also, none of the patients included in this study had the COVID-19. Based on frequency, the top 10 hospitals to which patients were transferred did not differ between the two periods. The proportion of patients transferred to these top 10 hospitals also did not differ between the two periods (pre-COVID-19 period: 73.9% vs. early-COVID-19 period: 77.1%, P value = 0.451).
The characteristics of EMS activation also did not show a significant difference between the two periods. The most frequent site of EMS activation was the patient’s home. There was no significant difference between the groups (pre-COVID-19 period: 77.4% vs. early-COVID-19 period: 83.1%, P value = 0.131). The most frequent time for EMS activation was between 6 AM and 12 PM (pre-COVID-19 period: 32.9% vs. early-COVID-19 period: 36.4%). The least frequent time for EMS activation was between 0 AM and 6 AM (pre-COVID-19 period: 10.3% vs. early-COVID-19 period: 13.9%). There was no significant difference between the groups (P value = 0.326).
The mean age of the enrolled patients was 69.5 ± 11.8 years old, and 293 (63%) were male. The most frequently reported symptom patients complained about when calling EMS was arm drift (73.8%). The patients’ initial mental state as evaluated by the EMT was 293 (63%) alert, 87 (18.7%) verbally responsive, 70 (15.1%) painfully responsive, and 15 (3.2%) unresponsive. The final diagnosis of the enrolled patients was 161 (34.6%) for hemorrhagic stroke and 304 (65.4%) for ischemic stroke.
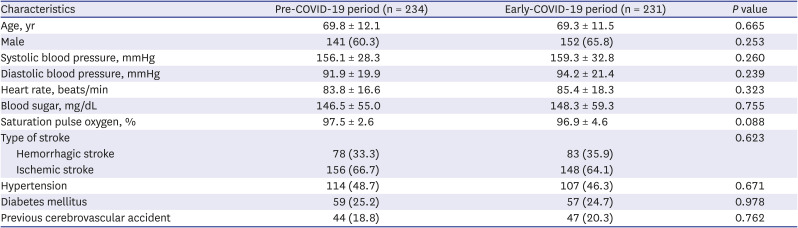
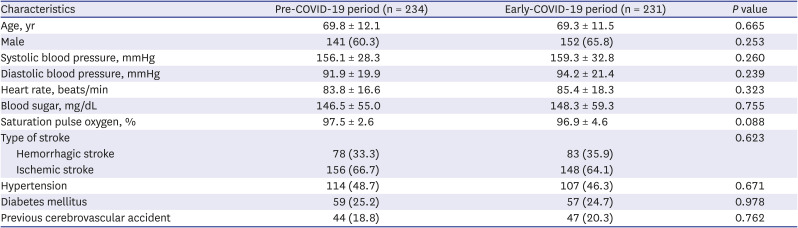
Clinical characteristics of patients in the pre-COVID-19 period group and early-COVID-19 period group were as follows (
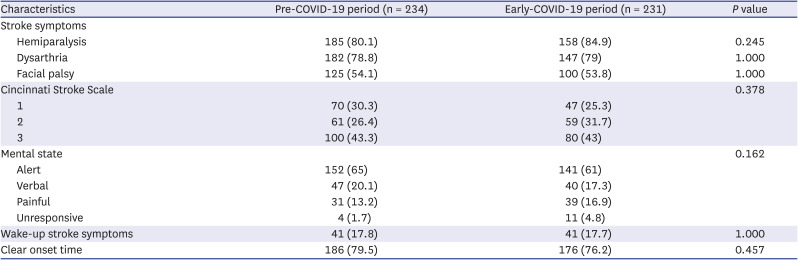
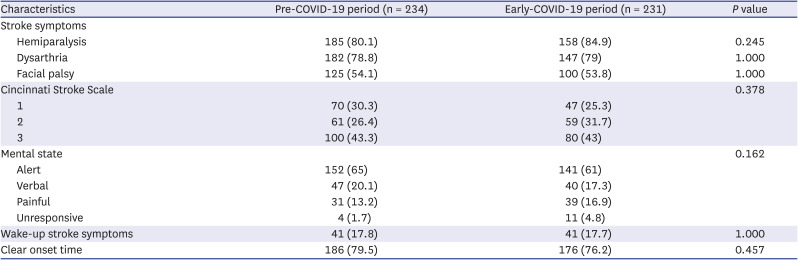
Table 1). All factors included in the study did not significantly differ between the groups. Stroke symptoms in the pre-COVID-19 period group and early-COVID-19 period group were as follows (
Table 2). All symptoms included in the study did not significantly differ between the groups, also.
Table 1
Clinical characteristics of patients in the pre-COVID-19 period and early-COVID-19 period groups
|
Characteristics |
Pre-COVID-19 period (n = 234) |
Early-COVID-19 period (n = 231) |
P value |
|
Age, yr |
69.8 ± 12.1 |
69.3 ± 11.5 |
0.665 |
|
Male |
141 (60.3) |
152 (65.8) |
0.253 |
|
Systolic blood pressure, mmHg |
156.1 ± 28.3 |
159.3 ± 32.8 |
0.260 |
|
Diastolic blood pressure, mmHg |
91.9 ± 19.9 |
94.2 ± 21.4 |
0.239 |
|
Heart rate, beats/min |
83.8 ± 16.6 |
85.4 ± 18.3 |
0.323 |
|
Blood sugar, mg/dL |
146.5 ± 55.0 |
148.3 ± 59.3 |
0.755 |
|
Saturation pulse oxygen, % |
97.5 ± 2.6 |
96.9 ± 4.6 |
0.088 |
|
Type of stroke |
|
|
0.623 |
|
Hemorrhagic stroke |
78 (33.3) |
83 (35.9) |
|
Ischemic stroke |
156 (66.7) |
148 (64.1) |
|
Hypertension |
114 (48.7) |
107 (46.3) |
0.671 |
|
Diabetes mellitus |
59 (25.2) |
57 (24.7) |
0.978 |
|
Previous cerebrovascular accident |
44 (18.8) |
47 (20.3) |
0.762 |

Table 2
Stroke symptoms of patients in the pre-COVID-19 period and early-COVID-19 period groups
|
Characteristics |
Pre-COVID-19 period (n = 234) |
Early-COVID-19 period (n = 231) |
P value |
|
Stroke symptoms |
|
|
|
|
Hemiparalysis |
185 (80.1) |
158 (84.9) |
0.245 |
|
Dysarthria |
182 (78.8) |
147 (79) |
1.000 |
|
Facial palsy |
125 (54.1) |
100 (53.8) |
1.000 |
|
Cincinnati Stroke Scale |
|
|
0.378 |
|
1 |
70 (30.3) |
47 (25.3) |
|
2 |
61 (26.4) |
59 (31.7) |
|
3 |
100 (43.3) |
80 (43) |
|
Mental state |
|
|
0.162 |
|
Alert |
152 (65) |
141 (61) |
|
Verbal |
47 (20.1) |
40 (17.3) |
|
Painful |
31 (13.2) |
39 (16.9) |
|
Unresponsive |
4 (1.7) |
11 (4.8) |
|
Wake-up stroke symptoms |
41 (17.8) |
41 (17.7) |
1.000 |
|
Clear onset time |
186 (79.5) |
176 (76.2) |
0.457 |

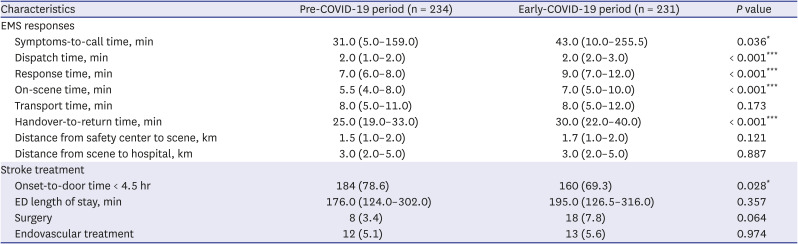
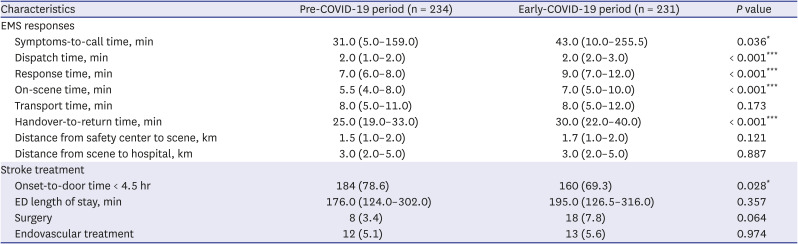
Characteristics of EMS responses in the pre-COVID-19 period group and early-COVID-19 period group were as follows (
Table 3). In the early-COVID-19 period group, symptom-to-call time, dispatch time, response time, on-scene time, and handover-to-return time were significantly longer than in the pre-COVID-19 period group. Only transport time did not significantly differ between the two groups. EMS response distance did not significantly differ between the groups. Characteristics of stroke treatment in the pre-COVID-19 period group and early-COVID-19 period group were as follows (
Table 3). The early-COVID-19 period group had significantly fewer patients whose call-to-door time within 4.5 hours. Other factors included in the study did not significantly differ between the groups.
Table 3
Characteristics of EMS responses and stroke treatment in the pre-COVID-19 period and early-COVID-19 period groups
|
Characteristics |
Pre-COVID-19 period (n = 234) |
Early-COVID-19 period (n = 231) |
P value |
|
EMS responses |
|
|
|
|
Symptoms-to-call time, min |
31.0 (5.0–159.0) |
43.0 (10.0–255.5) |
0.036*
|
|
Dispatch time, min |
2.0 (1.0–2.0) |
2.0 (2.0–3.0) |
< 0.001***
|
|
Response time, min |
7.0 (6.0–8.0) |
9.0 (7.0–12.0) |
< 0.001***
|
|
On-scene time, min |
5.5 (4.0–8.0) |
7.0 (5.0–10.0) |
< 0.001***
|
|
Transport time, min |
8.0 (5.0–11.0) |
8.0 (5.0–12.0) |
0.173 |
|
Handover-to-return time, min |
25.0 (19.0–33.0) |
30.0 (22.0–40.0) |
< 0.001***
|
|
Distance from safety center to scene, km |
1.5 (1.0–2.0) |
1.7 (1.0–2.0) |
0.121 |
|
Distance from scene to hospital, km |
3.0 (2.0–5.0) |
3.0 (2.0–5.0) |
0.887 |
|
Stroke treatment |
|
|
|
|
Onset-to-door time < 4.5 hr |
184 (78.6) |
160 (69.3) |
0.028*
|
|
ED length of stay, min |
176.0 (124.0–302.0) |
195.0 (126.5–316.0) |
0.357 |
|
Surgery |
8 (3.4) |
18 (7.8) |
0.064 |
|
Endovascular treatment |
12 (5.1) |
13 (5.6) |
0.974 |

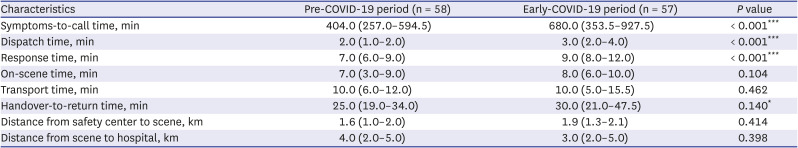
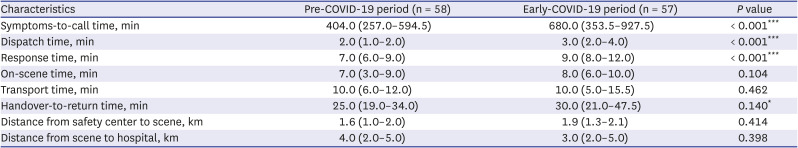
For EMS responses, a subgroup analysis was performed for patients above the 75th percentile of total EMS response time (
Table 4). In the early-COVID-19 period group, symptom-to-call time, dispatch time, response time, and handover-to-return time was longer than in the pre-COVID-19 period group. Symptom-to-call time showed a more significant difference compared to the overall group analysis. There was no significant difference in on-scene time and transport time, which significantly differ in the overall group analysis. EMS response distance also did not significantly differ between the groups.
Table 4
Characteristics of EMS responses for patients above the 75th percentile of total EMS response time in the pre-COVID-19 period and early-COVID-19 period groups
|
Characteristics |
Pre-COVID-19 period (n = 58) |
Early-COVID-19 period (n = 57) |
P value |
|
Symptoms-to-call time, min |
404.0 (257.0–594.5) |
680.0 (353.5–927.5) |
< 0.001***
|
|
Dispatch time, min |
2.0 (1.0–2.0) |
3.0 (2.0–4.0) |
< 0.001***
|
|
Response time, min |
7.0 (6.0–9.0) |
9.0 (8.0–12.0) |
< 0.001***
|
|
On-scene time, min |
7.0 (3.0–9.0) |
8.0 (6.0–10.0) |
0.104 |
|
Transport time, min |
10.0 (6.0–12.0) |
10.0 (5.0–15.5) |
0.462 |
|
Handover-to-return time, min |
25.0 (19.0–34.0) |
30.0 (21.0–47.5) |
0.140*
|
|
Distance from safety center to scene, km |
1.6 (1.0–2.0) |
1.9 (1.3–2.1) |
0.414 |
|
Distance from scene to hospital, km |
4.0 (2.0–5.0) |
3.0 (2.0–5.0) |
0.398 |

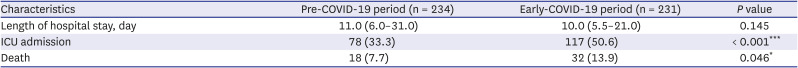
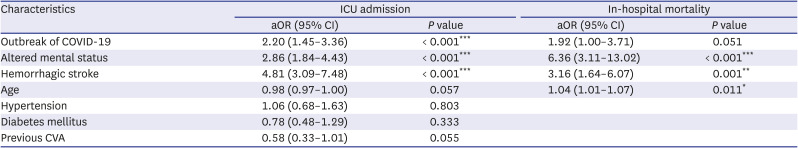
Clinical outcomes of acute stroke in the early-COVID-19 period group and pre-COVID-19 period group were as follows (
Table 5). The early-COVID-19 period group had significantly more patients who were admitted to the ICU or died. Length of hospital stay did not significantly differ between the groups.
Table 5
Clinical outcomes of acute stroke in the pre-COVID-19 period and early-COVID-19 period groups
|
Characteristics |
Pre-COVID-19 period (n = 234) |
Early-COVID-19 period (n = 231) |
P value |
|
Length of hospital stay, day |
11.0 (6.0–31.0) |
10.0 (5.5–21.0) |
0.145 |
|
ICU admission |
78 (33.3) |
117 (50.6) |
< 0.001***
|
|
Death |
18 (7.7) |
32 (13.9) |
0.046*
|

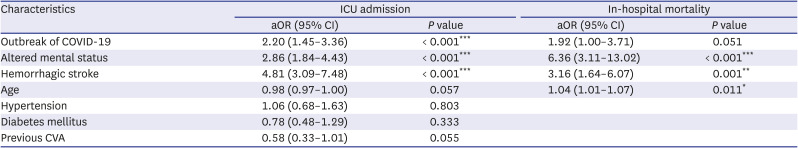
The results of the logistical regression analysis were as follows (
Table 6). Outbreak of COVID-19, altered mental status, hemorrhagic stroke were independent factors associated with ICU admission for patients with acute stroke. Altered mental status, hemorrhagic stroke, age were independent factors associated with in-hospital mortality for patients with acute stroke.
Table 6
Results of logistic regression analyses
|
Characteristics |
ICU admission |
In-hospital mortality |
|
aOR (95% CI) |
P value |
aOR (95% CI) |
P value |
|
Outbreak of COVID-19 |
2.20 (1.45–3.36) |
< 0.001***
|
1.92 (1.00–3.71) |
0.051 |
|
Altered mental status |
2.86 (1.84–4.43) |
< 0.001***
|
6.36 (3.11–13.02) |
< 0.001***
|
|
Hemorrhagic stroke |
4.81 (3.09–7.48) |
< 0.001***
|
3.16 (1.64–6.07) |
0.001**
|
|
Age |
0.98 (0.97–1.00) |
0.057 |
1.04 (1.01–1.07) |
0.011*
|
|
Hypertension |
1.06 (0.68–1.63) |
0.803 |
|
|
|
Diabetes mellitus |
0.78 (0.48–1.29) |
0.333 |
|
|
|
Previous CVA |
0.58 (0.33–1.01) |
0.055 |
|
|

DISCUSSION
We observed that pre-hospital time for acute stroke were significantly delayed during the sudden outbreak of COVID-19. During the same period, the clinical outcomes of patients with acute stroke were also significantly deteriorated. Considering the results of previous studies that demonstrated that earlier treatment has a significant impact on the good prognosis of patients with acute stroke, the deteriorating prognosis of this population was expected to be associated with pre-hospital delay for acute stroke.
The management of acute stroke is rapidly changing based on evidence of thrombectomy’s effectiveness. There is currently a great emphasis on rapidly transferring patients with stroke symptoms to a thrombectomy-capable center. As a result, there are continuous efforts to reduce pre-hospital delays. Several recent studies are also focusing on pre-hospital settings.
16
There have been some studies on factors associated with pre-hospital delays. Waiting for spontaneous recovery, caused by a lack of knowledge regarding stroke symptoms, was approximately 15 times more likely to result in a pre-hospital delay.
17 In addition, stroke patients who visited their family doctors instead of making EMS calls had approximately four times the odds, and situations in which it was difficult to recognize stroke symptoms, such as in cases of a patient with an alert mental state, had about three times the odds.
1819
Studies show that the COVID-19 pandemic could be associated with delays in managing acute stroke. However, compared to the research on in-hospital delays, it was difficult to find a study on pre-hospital delays. The only study we found showed that stroke onset-to-door time was delayed by about an hour after COVID-19 was contained in Hong Kong.
20 We conducted this study to identify the impact of the sudden outbreak of COVID-19 on pre-hospital delays of stroke management and the clinical outcomes of acute stroke.
This study was conducted at the top five fire stations selected based on the number of dispatches among a total of 24 fire stations in Seoul, Korea. The locations of the five fire stations are one in the northeast region, one in the northwest region, one in the southeast region, and two in the southwest region (
Supplementary Fig. 1). During the early-COVID-19 period, a total of 18,104 patients activated EMS due to neurological abnormalities. Of these, 5,043 (27.9%) were assigned to the five fire stations included in the study. This proportion was not significantly different from the proportion (29.2%) assigned to the five fire stations during the pre-COVID-19 period.
Of the 465 enrolled patients, 231 (49.7%) were in the early-COVID-19 period group and 234 (50.3%) in the pre-COVID-19 period group. There were no significant differences among the patients in each group. The clinical characteristics and stroke symptoms did not differ significantly between the groups. Our analysis allowed us to observe similarities between the groups suitable for a comparative cross-sectional study.
Among the EMS response characteristics, the variables that significantly differed included symptom-to-call time, dispatch time, response time, on-scene time, and handover-to-return time. The difference in symptom-to-call time is likely because patients were waiting for spontaneous recovery due to fear of COVID-19. The difference in dispatch time is likely the result of a lack of general ambulances because many ambulances were dedicated to patients suspected of having COVID-19. The differences observed in response and on-scene time are likely a result of EMT taking time to wear protective equipment and adhering to precautionary COVID-19 guidelines. The difference in handover-to-return time may be a result of delayed handover due to overcrowding in ED.
In subgroup analysis, the difference in symptom-to-call time was more prominent. The median symptom-to-call time, which was 12 minutes in the overall group analysis, increased to 276 minutes in the subgroup analysis. In contrast, each component of the EMS response time did not show a significant difference compared to the overall group analysis. The dramatic delay in symptom-to-call time may be closely associated with the deteriorating prognosis in patients with acute stroke during the early-COVID-19 period.
Among the characteristics of stroke treatment, the variable that significantly differed was call-to-door time. The difference in call-to-door time may be a result of pre-hospital delay for acute stroke. ED length of stay, surgery, and endovascular treatment did not significantly differ between the groups. These results are inconsistent with those of previous studies showing that the total number of thrombolysis and thrombectomy decreased during COVID-19 outbreak.
910 It may be explained by the fact that the scale of COVID-19 outbreak in Korea was smaller than in other countries. Further research will be needed to identify the factors influencing these associations.
Among the clinical outcomes of acute stroke, the dependent variables with significant differences were admission to ICU and death. These variables were highly correlated with severity. However, some factors that affect clinical outcomes, such as delayed diagnosis and treatment of acute stroke, may be associated with pre-hospital delays. These results are consistent with those of previous studies showing that patients with acute stroke who receive reperfusion treatment or endovascular thrombectomy earlier have less disability and better survival rates.
3
The significant variables in the logistical analysis of ICU admission were outbreak of COVID-19, altered mental status, and hemorrhagic stroke. The odds ratios of variables related to risk factors were relatively larger, but the odds ratio of COVID-19 outbreak was also large at 2.20. The significant variables in the logistical analysis of in-hospital mortality were altered mental status, hemorrhagic stroke, and age. There were more patients who experienced in-hospital mortality during the early-COVID-19 period, but it was not statistically significant (P value = 0.051).
This study had several limitations. First, the data were collected from EMS data registry, not from individual medical records. It was difficult to objectively and accurately evaluate information associated with acute stroke management in the hospital, e.g., intravenous thrombolysis. This influence may have been underestimated. Second, because of the above reasons, the severity of acute stroke was analyzed using the LAPSS scale assessed by EMTs at the scene. In order to more objectively analyze the severity of acute stroke, the National Institutes of Health Stroke Scale should be used, but it could not be used due to limitations of the data. Third, the subjects in this study were assessed by EMTs as positive on the LAPSS scale. It was not possible to analyze patients who were scored negatively. To more accurately evaluate the impact of the sudden outbreak of infectious disease on EMS for acute stroke, research should include patients whose final diagnosis is acute stroke in the hospital, including those who were negative on the LAPSS scale. Fourth, this was a retrospective study based on EMS registry data and special EMS records for cardio-cerebrovascular disease, and so the statistical analysis can`t completely control for confounders.
In conclusion, after the sudden COVID-19 outbreak, pre-hospital time, especially symptom-to-call time, was delayed in patients with acute stoke and the clinical outcomes of these patients deteriorated. This suggests that the deteriorating prognosis in patients with acute stroke was associated with the pre-hospital delay caused by the burden on EMS. These results provide a theoretical foundation for the development of additional guidelines to provide adequate EMS for acute stroke, even during a sudden outbreak of infectious disease. Health authorities should establish these guidelines in preparation for similar situations in the future.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download