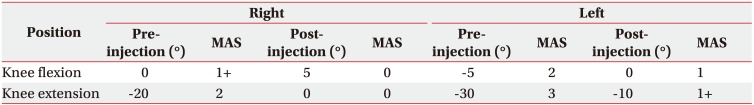
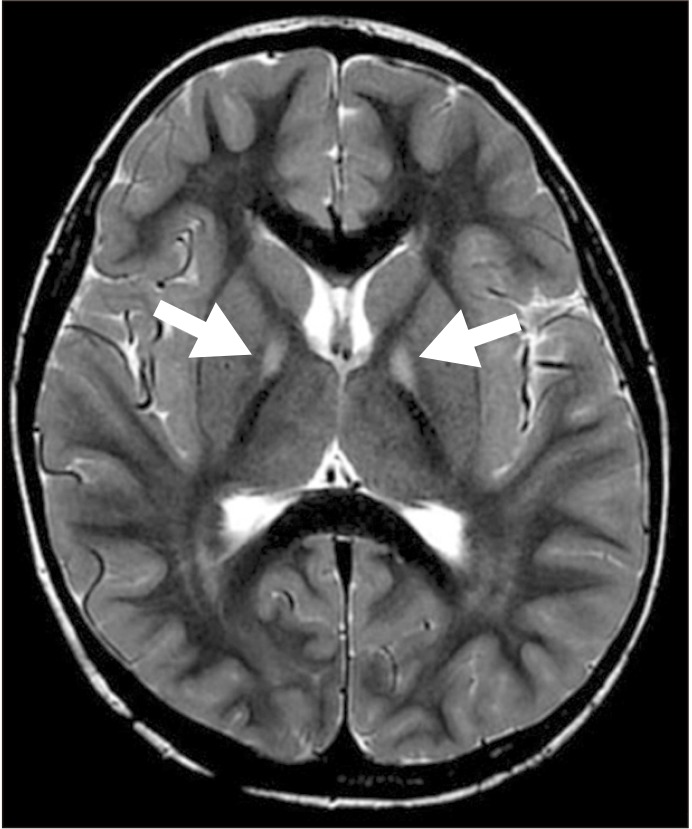
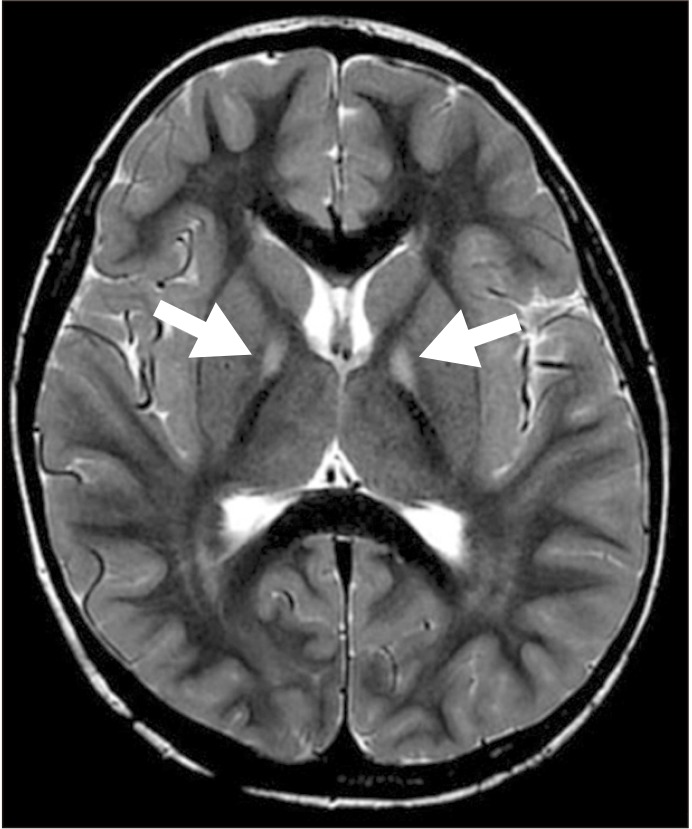
A 33-month-old boy was admitted to the rehabilitation department with complaints of gait disturbances. The patient had a normal birth history with history of two febrile seizures at 4 and 7 months of age. The patient had severe contraction of both calf muscles and inversion of both feet, resulting in equinovarus in both lower extremities, more evident on the left side. Ankle plantarflexor spasticity measured by the Modified Ashworth Scale (MAS), was 2 on the right and 3 on the left during knee extension. Tip-toe walking and waddling gait were observed, which was found to be aggravating on standing, and it was noted that the patient had an inability to walk in a straight line with repetitive falling due to trunk imbalance. An inability of the patient to communicate with incomprehensible verbal output was confirmed as speech and language retardation by the Sequenced Language Scale for Infants (SELSI) test, and Korean version of Bayley Scale of Infant Development second edition (BSID-II) assessment was revealed moderate development retardation in both cognitive and motor domains. The characteristic dystonia symptom was obscured, and accompanied by sleeping problems. An ophthalmic examination was conducted to discard any ocular problems, but it could not be completed due to the patient's poor cooperation. The biochemical assessments indicated normal levels in serum electrolyte, ammonia, amino acid, liver function test, cerebrospinal fluid examinations, and metabolic disorder studies. The brain magnetic resonance imaging (MRI) demonstrated high bilateral T2 signal intensity on the anteromedial region of both GP (
Fig. 1). The NBIA was suspected and a diagnostic exome sequencing test was conducted. The NBIA type 1 (PKAN) was confirmed by detection of two mutations, p.Arg440Pro and c.524delT, in
PANK2 (
Table 1). A comprehensive ophthalmic examination was conducted, but it could not be completed due to patient's poor cooperation. At that time, daily rehabilitation therapy was conducted to improve the balance, postural stability, and spasticity. Because the parents of the patient were against invasive treatment at first, the baclofen 20 mg/day was started for spasticity control and the dose was increased to 45 mg/day after 5 days. After 4 weeks, clinical symptoms remained unchanged, and the parents were persuaded to trial of botulinum toxin injection using Botox (onabotulinumtoxinA; Allergan Inc., Irvine, CA, USA) to both calf muscles while maintaining the baclofen administration. The patient's weight was 14 kg. Twenty-five units of botulinum toxin were injected into both tibialis posterior muscles to improve the ankle inversion. The plantarflexor spasticity was more severe on the left side than the right. We thus decided to inject botulinum toxin into the left plantarflexor muscles (60 units into medial gastrocnemius and 30 units into soleus) only, considering the total maximum body dose (12 units per kg total body weight) [
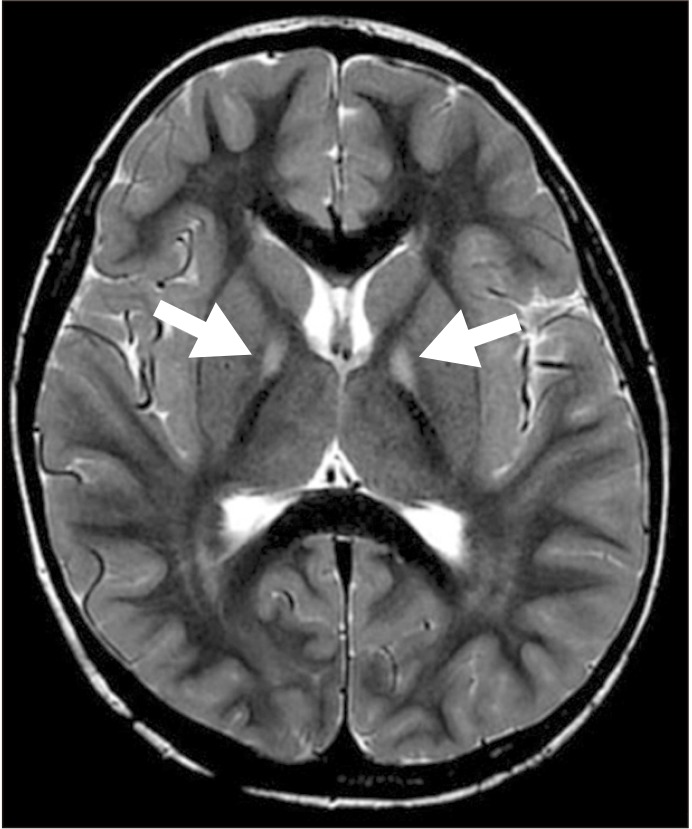
6]. The procedure was performed under ultrasonography guidance by an experienced physiatrist. After 2 weeks, the passive range of motion (PROM) of ankle dorsiflexion during knee extension improved from −20° to 0° in the right, and −30° to −10° in the left. The PROM of the ankle dorsiflexion during knee flexion, demonstrated an improvement from 0° to 5° in the right and from −5° to 0° in the left. Further, the ankle plantarflexor spasticity reduced to MAS 0 on the right and MAS 1+ on the left in knee extension, and to MAS 0 on the right, and MAS 1 on the left in knee flexion (
Table 2). In comparison with the pre-injection state, both heels touched the ground, and the patient was able to walk independently for up to 10 m in a straight-line without falling or stumbling. The solid plastic ankle foot orthosis (AFO) for the patient were prescribed, and the rehabilitation therapy was continued. The patient was discharged after the 4 weeks of the botulinum toxin injection, and was consequently followed up by the out-patient department. The anti-spasticity medication was discontinued after 8 weeks of the botulinum toxin injection on the observing of an improvement in ankle plantarflexor spasticity, which persisted without deterioration.
 | Fig. 1T2-weighted brain magnetic resonance imaging. Arrows indicate bilateral T2 high signal intensity in anteromedial portion of both globus pallidus.
|
Table 1
Type of detected gene mutation
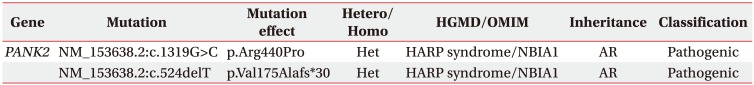

Table 2
Improvement of range of motion on ankle dorsiflexion