1. Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JW, Weir DR. Cohort Profile: the Health and Retirement Study (HRS). Int J Epidemiol. 2014; 43:576–585. PMID:
24671021.

2. Borsch-Supan A, Brandt M, Hunkler C, Kneip T, Korbmacher J, Malter F, et al. Data resource profile: the Survey of Health, Ageing and Retirement in Europe (SHARE). Int J Epidemiol. 2013; 42:992–1001. PMID:
23778574.
3. Steptoe A, Breeze E, Banks J, Nazroo J. Cohort profile: the English longitudinal study of ageing. Int J Epidemiol. 2013; 42:1640–1648. PMID:
23143611.

4. Boo KC, Chang JY. Korean longitudinal study of ageing: research design for international comparative studies. Surv Res. 2006; 7:97–122.
5. Hong KS, Bang OY, Kang DW, Yu KH, Bae HJ, Lee JS, et al. Stroke statistics in Korea: part I. Epidemiology and risk factors: a report from the Korean stroke society and clinical research center for stroke. J Stroke. 2013; 15:2–20. PMID:
24324935.

6. Lim SJ, Kim HJ, Nam CM, Chang HS, Jang YH, Kim S, et al. Socioeconomic costs of stroke in Korea: estimated from the Korea national health insurance claims database. J Prev Med Public Health. 2009; 42:251–260. PMID:
19675402.

7. Hong KS, Bang OY, Kim JS, Heo JH, Yu KH, Bae HJ, et al. Stroke statistics in Korea: part II stroke awareness and acute stroke care, a report from the Korean Stroke Society and Clinical Research Center for Stroke. J Stroke. 2013; 15:67–77. PMID:
24324942.

8. Shih RA, Lee J, Das L. Harmonization of cross-national studies of aging to the health and retirement study: cognition. Santa Monica: RAND Corporation;2012.
9. Buz J, Cortes-Rodriguez M. Measurement of the severity of disability in community-dwelling adults and older adults: interval-level measures for accurate comparisons in large survey data sets. BMJ Open. 2016; 6:e011842.

10. Cieza A, Oberhauser C, Bickenbach J, Jones RN, Ustun TB, Kostanjsek N, et al. The English are healthier than the Americans: really. Int J Epidemiol. 2015; 44:229–238. PMID:
25231371.

11. Grimby G, Andren E, Holmgren E, Wright B, Linacre JM, Sundh V. Structure of a combination of Functional Independence Measure and Instrumental Activity Measure items in community-living persons: a study of individuals with cerebral palsy and spina bifida. Arch Phys Med Rehabil. 1996; 77:1109–1114. PMID:
8931519.

12. Altman BM. Definitions, concepts, and measures of disability. Ann Epidemiol. 2014; 24:2–7. PMID:
24268996.

13. Wright BD, Linacre JM. Observations are always ordinal; measurements, however, must be interval. Arch Phys Med Rehabil. 1989; 70:857–860. PMID:
2818162.
14. Wright BD, Stone MH. Best test design. Chicago, IL: Mesa Press;1979.
15. Chan KS, Kasper JD, Brandt J, Pezzin LE. Measurement equivalence in ADL and IADL difficulty across international surveys of aging: findings from the HRS, SHARE, and ELSA. J Gerontol B Psychol Sci Soc Sci. 2012; 67:121–132. PMID:
22156662.

16. Hong I, Yoo EY, Kazley AS, Lee D, Li CY, Reistetter TA. Development and validation of the activities of daily living short form for community-dwelling Korean stroke survivors. Eval Health Prof. 2018; 41:44–66. PMID:
29179561.

17. Won CW, Rho YG, Kim SY, Cho BR, Lee YS. The validity and reliability of Korean Activities of Daily Living(KADL) Scale. J Korean Geriatr Soc. 2002; 6:98–106.
18. Won CW, Rho YG, SunWoo D, Lee YS. The validity and reliability of Korean Instrumental Activities of Daily Living(K-IADL) Scale. J Korean Geriatr Soc. 2002; 6:273–280.
19. Won CW, Yang KY, Rho YG, Kim SY, Lee EJ, Yoon JL, et al. The development of Korean Activities of Daily Living(K-ADL) and Korean Instrumental Activities of Daily Living(K-IADL) Scale. J Korean Geriatr Soc. 2002; 6:107–120.
20. Reeve BB, Hays RD, Bjorner JB, Cook KF, Crane PK, Teresi JA, et al. Psychometric evaluation and calibration of health-related quality of life item banks: plans for the Patient-Reported Outcomes Measurement Information System (PROMIS). Med Care. 2007; 45(5 Suppl 1):S22–S31. PMID:
17443115.
22. Tabachnick BG, Fidell LS. Using multivariate statistics. 5th ed. Boston: Pearson;2006.
23. Andrich D. A rating formulation for ordered response categories. Psychometrika. 1978; 43:561–573.

25. Wright BD. Despair and hope for educational measurement. Contemp Educ Rev. 1984; 3:281–288.
26. Bond TG, Fox CM. Applying the Rasch model fundamental measurement in the human sciences. Mahwah: Psychology Press;2001.
27. Linacre JM. What do infit and outfit, mean-square and standardization mean. Rasch Meas Trans. 2002; 16:878.
28. Wright BD, Linacre JM, Gustafson JE, Martin-Lof P. Reasonable mean-square fit values. Rasch Meas Trans. 1994; 8:370.
29. Linacre JM. When to stop removing items and persons in Rasch misfit analysis. Rasch Meas Trans. 2010; 23:1241.
30. Fisher WP. Reliability, separation, strata statistics. Rasch Meas Trans. 1992; 6:238.
31. Fisher W. Rating scale instrument quality criteria. Rasch Meas Trans. 2007; 21:1095.
32. Wright BD, Masters GN. Rating scale analysis. Chicago: Mesa Press;1982.
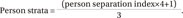
33. Harvill LM. Standard error of measurement. Educ Meas. 1991; 10:33–41.
34. Mallinson T, Stelmack J, Velozo C. A comparison of the separation ratio and coefficient alpha in the creation of minimum item sets. Med Care. 2004; 42(1 Suppl):I17–I24. PMID:
14707752.
35. Linacre JM. Sample size and item calibration stability. Rasch Meas Trans. 1994; 7:328.
36. Wang WC, Chen CT. Item parameter recovery, standard error estimates, and fit statistics of the WINSTEPS program for the family of Rasch models. Educ Psychol Meas. 2005; 65:376–404.

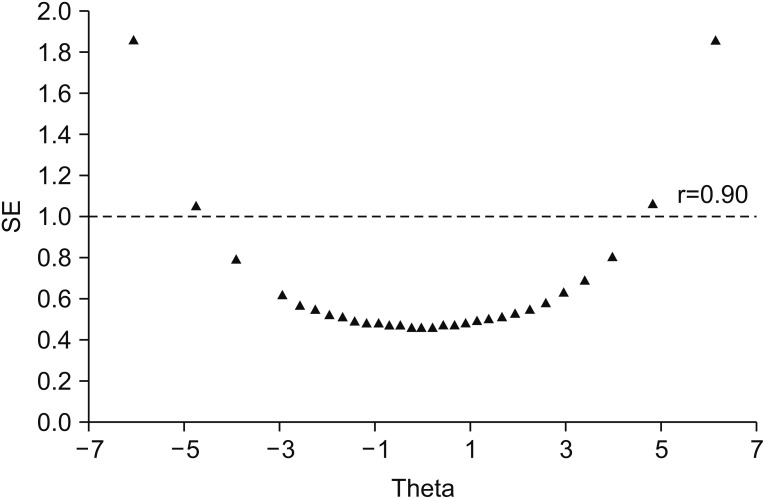
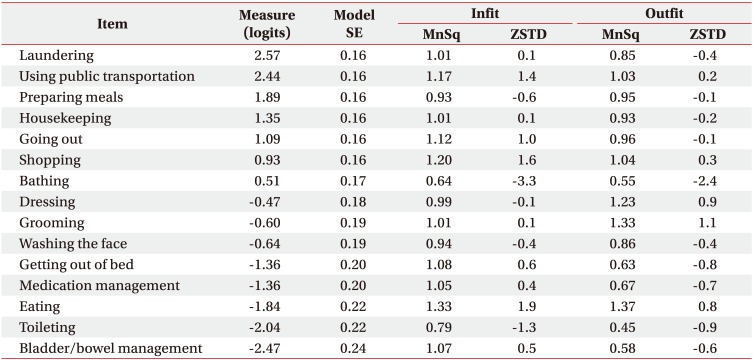
 ) with the standardized loadings of each item on the dominant factor structure. Factor loadings greater than 0.70 were considered adequate [22]. We also examined local independence, one of the IRT core assumptions, using the residual correlation coefficient extracted from the dominant factor. We considered test items having a residual correlation value greater than or equal to 0.2 as problematic items [2021].
) with the standardized loadings of each item on the dominant factor structure. Factor loadings greater than 0.70 were considered adequate [22]. We also examined local independence, one of the IRT core assumptions, using the residual correlation coefficient extracted from the dominant factor. We considered test items having a residual correlation value greater than or equal to 0.2 as problematic items [2021]. =0.944) in observed summative scores across the 17 ADL items. These findings indicate that the ADL instrument met the unidimensionality assumption and measures a single construct. There was no violation of the local independence assumption, and all the residual correlations ranged from 0.000 to 0.118 (<0.20). Since these findings supported a unidimensional ADL instrument, Rasch analysis was subsequently performed.
=0.944) in observed summative scores across the 17 ADL items. These findings indicate that the ADL instrument met the unidimensionality assumption and measures a single construct. There was no violation of the local independence assumption, and all the residual correlations ranged from 0.000 to 0.118 (<0.20). Since these findings supported a unidimensional ADL instrument, Rasch analysis was subsequently performed.



 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download