1. Després JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006; 444:881–887. PMID:
17167477.

2. Després JP, Lemieux I, Bergeron J, Pibarot P, Mathieu P, Larose E, Rodés-Cabau J, Bertrand OF, Poirier P. Abdominal obesity and the metabolic syndrome: contribution to global cardiometabolic risk. Arterioscler Thromb Vasc Biol. 2008; 28:1039–1049. PMID:
18356555.

3. Grundy SM. Obesity, metabolic syndrome, and cardiovascular disease. J Clin Endocrinol Metab. 2004; 89:2595–2600. PMID:
15181029.


4. Korean Society for the Study of Obesity. 2017 Obesity Fact Sheet. Seoul: Korean Society for the Study of Obesity;2017.
5. Korean Society for the Study of Obesity. 2018 Obesity Fact Sheet. Seoul: Korean Society for the Study of Obesity;2018.
6. Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM. Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002; 346:393–403. PMID:
11832527.

7. Gill JM, Malkova D. Physical activity, fitness and cardiovascular disease risk in adults: interactions with insulin resistance and obesity. Clin Sci (Lond). 2006; 110:409–425. PMID:
16526946.

8. Ziccardi P, Nappo F, Giugliano G, Esposito K, Marfella R, Cioffi M, D'Andrea F, Molinari AM, Giugliano D. Reduction of inflammatory cytokine concentrations and improvement of endothelial functions in obese women after weight loss over one year. Circulation. 2002; 105:804–809. PMID:
11854119.


9. Cornier MA, Dabelea D, Hernandez TL, Lindstrom RC, Steig AJ, Stob NR, Van Pelt RE, Wang H, Eckel RH. The metabolic syndrome. Endocr Rev. 2008; 29:777–822. PMID:
18971485.



10. Dunkley AJ, Charles K, Gray LJ, Camosso-Stefinovic J, Davies MJ, Khunti K. Effectiveness of interventions for reducing diabetes and cardiovascular disease risk in people with metabolic syndrome: systematic review and mixed treatment comparison meta-analysis. Diabetes Obes Metab. 2012; 14:616–625. PMID:
22284386.


11. Oh EG, Bang SY, Hyun SS, Kim SH, Chu SH, Jeon JY, Im JA, Lee MK, Lee JE. Effects of a 6-month lifestyle modification intervention on the cardiometabolic risk factors and health-related qualities of life in women with metabolic syndrome. Metabolism. 2010; 59:1035–1043. PMID:
20045151.


12. Yamaoka K, Tango T. Effects of lifestyle modification on metabolic syndrome: a systematic review and meta-analysis. BMC Med. 2012; 10:138. PMID:
23151238.



13. Hays NP, Bathalon GP, McCrory MA, Roubenoff R, Lipman R, Roberts SB. Eating behavior correlates of adult weight gain and obesity in healthy women aged 55–65 y. Am J Clin Nutr. 2002; 75:476–483. PMID:
11864852.


14. Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, McManus K, Champagne CM, Bishop LM, Laranjo N, Leboff MS, Rood JC, de Jonge L, Greenway FL, Loria CM, Obarzanek E, Williamson DA. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med. 2009; 360:859–873. PMID:
19246357.

15. Livingston E, Zylke JW. JAMA obesity theme issue: call for papers. JAMA. 2012; 307:970–971.
16. Roberto CA, Kawachi I. Behavioral Economics and Public Health. New York (NY): Oxford University Press;2015. p. 133–160.
17. Pontzer H, Raichlen DA, Wood BM, Mabulla AZ, Racette SB, Marlowe FW. Hunter-gatherer energetics and human obesity. PLoS One. 2012; 7:e40503. PMID:
22848382.

18. Fock KM, Khoo J. Diet and exercise in management of obesity and overweight. J Gastroenterol Hepatol. 2013; 28 Suppl 4:59–63. PMID:
24251706.


19. American College of Cardiology/American Heart Association Task Force on Practice Guidelines, Obesity Expert Panel, 2013. Executive summary: Guidelines (2013) for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Obesity Society published by the Obesity Society and American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Based on a systematic review from the The Obesity Expert Panel, 2013. Obesity (Silver Spring). 2014; 22 Suppl 2:S5–S39. PMID:
24961825.
20. Ryan DH, Kahan S. Guideline recommendations for obesity management. Med Clin North Am. 2018; 102:49–63. PMID:
29156187.


21. Strychar I. Diet in the management of weight loss. CMAJ. 2006; 174:56–63. PMID:
16389240.



22. Astrup A, Ryan L, Grunwald GK, Storgaard M, Saris W, Melanson E, Hill JO. The role of dietary fat in body fatness: evidence from a preliminary meta-analysis of ad libitum low-fat dietary intervention studies. Br J Nutr. 2000; 83 Suppl 1:S25–S32. PMID:
10889789.

23. Slentz CA, Duscha BD, Johnson JL, Ketchum K, Aiken LB, Samsa GP, Houmard JA, Bales CW, Kraus WE. Effects of the amount of exercise on body weight, body composition, and measures of central obesity: STRRIDE--a randomized controlled study. Arch Intern Med. 2004; 164:31–39. PMID:
14718319.

24. Franz MJ, VanWormer JJ, Crain AL, Boucher JL, Histon T, Caplan W, Bowman JD, Pronk NP. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007; 107:1755–1767. PMID:
17904936.


25. Park J, Kim H. Short-term effects of a lifestyle intervention program on eating behaviors, physical activity and cardiovascular risks in Korean adults. Korean J Health Educ Promot. 2014; 31:37–49.

26. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program. Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation. 2002; 106:3143–3421. PMID:
12485966.

27. Oh SW. Obesity and metabolic syndrome in Korea. Diabetes Metab J. 2011; 35:561–566. PMID:
22247896.



28. Park J, Kim H, Cho S, Cho HI. The effects of “Healthy Life Plan” program on the management of obesity for Korean adults: a pilot study. Korean J Health Educ Promot. 2012; 29:89–101.
29. Yoo S, Kim H, Cho HI. Improvements in the metabolic syndrome and stages of change for lifestyle behaviors in Korean older adults. Osong Public Health Res Perspect. 2012; 3:85–93. PMID:
24159496.



30. Clark MM, Abrams DB, Niaura RS, Eaton CA, Rossi JS. Self-efficacy in weight management. J Consult Clin Psychol. 1991; 59:739–744. PMID:
1955608.


31. Kim WY, Cho MS, Lee HS. Development and validation of mini dietary assessment index for Koreans. Korean J Nutr. 2003; 36:83–92.
32. Van Strien T, Frijters JE, Bergers GP, Defares PB. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int J Eat Disord. 1986; 5:295–315.

33. Michels N, Sioen I, Braet C, Eiben G, Hebestreit A, Huybrechts I, Vanaelst B, Vyncke K, De Henauw S. Stress, emotional eating behaviour and dietary patterns in children. Appetite. 2012; 59:762–769. PMID:
22918173.


34. Striegel-Moore RH, Morrison JA, Schreiber G, Schumann BC, Crawford PB, Obarzanek E. Emotion-induced eating and sucrose intake in children: the NHLBI Growth and Health Study. Int J Eat Disord. 1999; 25:389–398. PMID:
10202649.


35. Braet C, Van Strien T. Assessment of emotional, externally induced and restrained eating behaviour in nine to twelve-year-old obese and non-obese children. Behav Res Ther. 1997; 35:863–873. PMID:
9299807.


36. Nguyen-Michel ST, Unger JB, Spruijt-Metz D. Dietary correlates of emotional eating in adolescence. Appetite. 2007; 49:494–499. PMID:
17466408.



37. Moens E, Braet C. Predictors of disinhibited eating in children with and without overweight. Behav Res Ther. 2007; 45:1357–1368. PMID:
17101117.


38. Macht M. How emotions affect eating: a five-way model. Appetite. 2008; 50:1–11. PMID:
17707947.

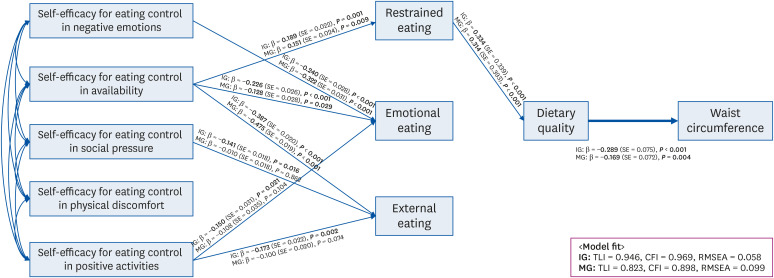
39. Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999; 6:1–55.

40. MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychol Methods. 1996; 1:130–149.

41. Duncan O. Introduction to Structural Equation Models. New York (NY): Academic Press;1975. p. 149–168.
42. Fagan J, Barnett M. The relationship between maternal gatekeeping, paternal competence, mothers' attitudes about the father role, and father involvement. J Fam Issues. 2003; 24:1020–1043.

43. Roach JB, Yadrick MK, Johnson JT, Boudreaux LJ, Forsythe WA 3rd, Billon W. Using self-efficacy to predict weight loss among young adults. J Am Diet Assoc. 2003; 103:1357–1359. PMID:
14520258.


44. Pells JJ, Shelby RA, Keefe FJ, Dixon KE, Blumenthal JA, Lacaille L, Tucker JM, Schmitt D, Caldwell DS, Kraus VB. Arthritis self-efficacy and self-efficacy for resisting eating: relationships to pain, disability, and eating behavior in overweight and obese individuals with osteoarthritic knee pain. Pain. 2008; 136:340–347. PMID:
17764844.


45. Glasofer DR, Haaga DA, Hannallah L, Field SE, Kozlosky M, Reynolds J, Yanovski JA, Tanofsky-Kraff M. Self-efficacy beliefs and eating behavior in adolescent girls at-risk for excess weight gain and binge eating disorder. Int J Eat Disord. 2013; 46:663–668. PMID:
23881587.



46. Mansyur CL, Pavlik VN, Hyman DJ, Taylor WC, Goodrick GK. Self-efficacy and barriers to multiple behavior change in low-income African Americans with hypertension. J Behav Med. 2013; 36:75–85. PMID:
22322910.


47. Doerksen SE, McAuley E. Social cognitive determinants of dietary behavior change in university employes. Front Public Health. 2014; 2:23. PMID:
24765620.



48. Nothwehr F. Self-efficacy and its association with use of diet-related behavioral strategies and reported dietary intake. Health Educ Behav. 2008; 35:698–706. PMID:
17602101.


49. Deutekom M, Vansenne F, McCaffery K, Essink-Bot ML, Stronks K, Bossuyt PM. The effects of screening on health behaviour: a summary of the results of randomized controlled trials. J Public Health (Oxf). 2011; 33:71–79. PMID:
20667898.


50. Imperial Cancer Research Fund OXCHECK Study Group. Effectiveness of health checks conducted by nurses in primary care: final results of the OXCHECK study. BMJ. 1995; 310:1099–1104. PMID:
7742676.
51. Wood D, Kinmonth A, Davies G, Yarwood J, Thompson S, Pyke S, Kok Y, Cramb R, Le Guen C, Marteau T, Durrington PN. Family Heart Study Group. Randomised controlled trial evaluating cardiovascular screening and intervention in general practice: principal results of British family heart study. BMJ. 1994; 308:313–320. PMID:
8124121.

52. Hutchison B, Birch S, Evans CE, Goldsmith LJ, Markham BA, Frank J, Paterson M. Screening for hypercholesterolaemia in primary care: randomised controlled trial of postal questionnaire appraising risk of coronary heart disease. BMJ. 1998; 316:1208–1213. PMID:
9552998.

53. Hwang WJ, Hong O, Kim MJ. Factors associated with blue-collar workers' risk perception of cardiovascular disease. J Korean Acad Nurs. 2012; 42:1095–1104. PMID:
23377606.


54. Kaufman DJ, Bollinger JM, Dvoskin RL, Scott JA. Risky business: risk perception and the use of medical services among customers of DTC personal genetic testing. J Genet Couns. 2012; 21:413–422. PMID:
22278220.


55. Sheeran P, Harris PR, Epton T. Does heightening risk appraisals change people’s intentions and behavior? A meta-analysis of experimental studies. Psychol Bull. 2014; 140:511–543. PMID:
23731175.


56. Kromhout D, Bosschieter EB, de Lezenne Coulander C. The inverse relation between fish consumption and 20-year mortality from coronary heart disease. N Engl J Med. 1985; 312:1205–1209. PMID:
3990713.

57. Mensink RP, Zock PL, Kester AD, Katan MB. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr. 2003; 77:1146–1155. PMID:
12716665.


58. Singh IM, Shishehbor MH, Ansell BJ. High-density lipoprotein as a therapeutic target: a systematic review. JAMA. 2007; 298:786–798. PMID:
17699012.
59. Webb TL, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res. 2010; 12:e4. PMID:
20164043.

60. Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009; 28:690–701. PMID:
19916637.

61. Hill JO, Peters JC. Environmental contributions to the obesity epidemic. Science. 1998; 280:1371–1374. PMID:
9603719.

62. Gupta SK. Intention-to-treat concept: a review. Perspect Clin Res. 2011; 2:109–112. PMID:
21897887.



63. Courtenay WH, McCreary DR, Merighi JR. Gender and ethnic differences in health beliefs and behaviors. J Health Psychol. 2002; 7:219–231. PMID:
22114246.


64. Furnham A, Kirkcaldy B. Age and sex differences in health beliefs and behaviours. Psychol Rep. 1997; 80:63–66. PMID:
9122353.


65. Wardle J, Steptoe A, Bellisle F, Davou B, Reschke K, Lappalainen R, Fredrikson M. Healthy dietary practices among European students. Health Psychol. 1997; 16:443–450. PMID:
9302541.

66. Deeks A, Lombard C, Michelmore J, Teede H. The effects of gender and age on health related behaviors. BMC Public Health. 2009; 9:213. PMID:
19563685.



67. Son HJ, Lee KE. The influence of health concern, health anxiety, and communication with healthcare providers on health information seeking behavior on the internet. J Health Inform Stat. 2019; 44:73–82.

68. Kim NJ. A study on the relation of health concern, health behavior, and subjective health status between the aged and the preliminary aged group. J Korea Soc Health Educ Promot. 2000; 17:99–110.
69. Yoon CK. The study on the relationship between health concern, health behavior, and subjective health cognition. J Korean Soc Health Inform Health Stat. 2004; 29:37–46.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download