INTRODUCTION
During the process of providing medical care, adverse events can occur due to both the treatment involved and medical errors.
1 Such events can be defined as patient safety incidents (PSIs), and minimizing PSIs is the primary goal in the field of patient safety. However, addressing the consequences of PSIs that have already occurred is as important as preventing PSIs.
2 This is because, once a PSI occurs, the associated patients, and their caregivers, can incur physical, mental, and financial damage, regardless of whether the incident was preventable.
345 Moreover, PSIs can also cause medical professionals, who provide medical care out of good will, to experience difficulties, such as emotional pain.
67 Medical professionals who are involved in a PSI and experience difficulties as a result are referred to as “second victims.”
6 Symptoms suffered by second victims are known to be similar to post-traumatic stress disorder (PTSD), so they need attention and support.
8
Being a second victim can have detrimental consequences, such as consideration of career change
9 and diminished job satisfaction.
10 In handling the incidents, second victims may also experience resentment to colleagues or superiors, which may adversely affect the patient safety culture.
7 Inappropriate support from peers and healthcare institutions may cause second victims to experience post-traumatic embitterment disorder (PTED).
71112 In particular, continuing to provide patient care before fully recovering from psychological damage experienced as a result of a PSI is known to increase the risk of another PSI occurring.
13 Thus, the implementation of specific and adequate support for second victims is necessary. To this end, examining the current status of second victims and quantifying the gravity of this problem are essential. A previous systematic literature review on second victims reported that the prevalence of second victims ranges from 10.4% to 43.3%.
6 Further, the review also reported that second victims may experience serious physical symptoms and behavioral responses, in addition to psychological difficulties.
6
However, most studies that have examined the prevalence of and/or difficulties experienced by second victims have been performed in western countries, meaning there is a relative scarcity of such studies in Asian countries, including Korea. In fact, no study has investigated the incidence of such adverse events in Korea, or even examined the gravity of the problem of second victims in the country.
14 Based on the findings of foreign literature, it can be speculated that there are numerous second victims in Korea.
6 Therefore, an in-depth examination of the status and gravity of the problem of second victims in Korea is needed. However, the deep-rooted hierarchical organizational culture and blame culture in Korean hospitals means that it is difficult to prevent PSIs, publicly discuss appropriate handling of PSIs, or conduct open research of these experiences.
15
In the present study, we aimed to examine the gravity of the second-victim problem in Korea. Specifically, we quantitatively assessed, among physicians who have been involved in PSIs, the characteristics of their PSI experiences, their consequent difficulties, and the level of PTSD and PTED they developed as a result. This study seeked to highlight the importance of the second-victim issue in Korea and, ultimately, to present evidence supporting the need to provide support for second victims.
METHODS
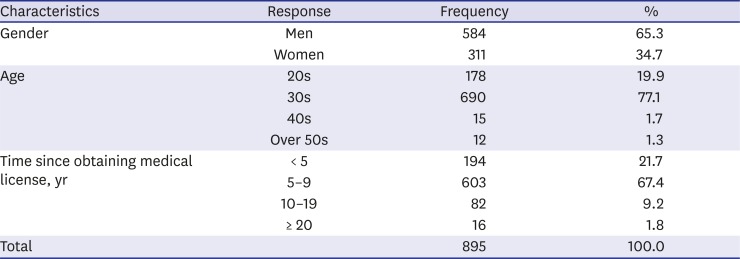
Forming part of our project to investigate PSI experiences and impact among the general public, physicians, and nurses, this study focused on the results of an anonymous self-report online survey conducted on physicians.
Questionnaire development and contents
We developed and structured the questionnaire in a manner that allowed us to compare the results with those of a previous survey of PSI experience and impacts among the general public.
3 The questionnaire items were developed with reference to studies on types of PSIs and their characteristics,
161718 as well as studies on second victims.
67 The research team comprised experts with rich research experience in the field of patient safety (including two physicians and three nurses), and the draft questionnaire was developed based on repeated discussion amongst the researchers. Then, we consulted a nursing professor, the president of a residents' association and the president of a private patient safety organization in regard to the applicability of the questionnaire content, and the questionnaire items and their phrasings were revised based on their opinions.
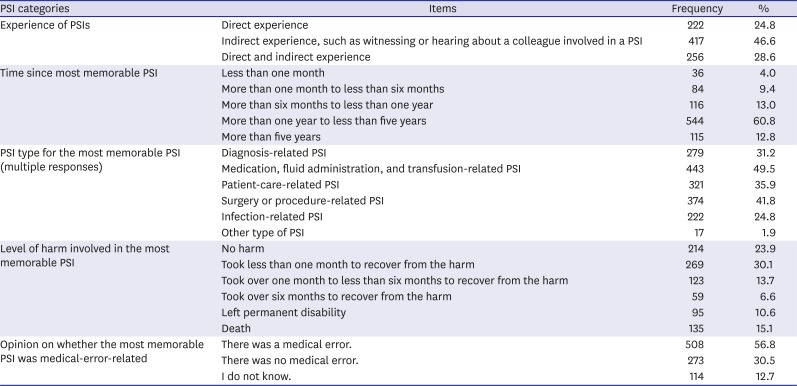
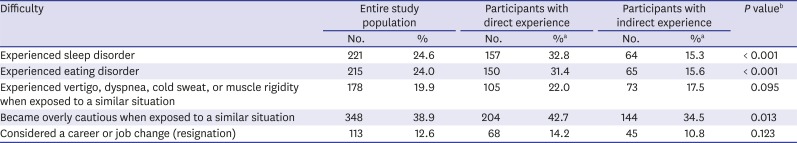
The final questionnaire comprised the following categories: PSI characteristics, PSI impacts, and socio-demographics. More specifically, PSI characteristics included items regarding the type(s) of PSI(s) experienced (e.g., direct exposure or indirect exposure; the latter concerns witnessing or hearing about a colleague's PSI experience); time since the most memorable PSI; the type of PSI in question (for the most memorable PSI; e.g., diagnosis-related, patient-care-related); the severity of harm caused by the most memorable PSI; and opinion on whether medical error was involved in the most memorable PSI. Second, analysis of PSI impacts comprised items regarding five types of difficulties associated with PSI experience: “sleep disorder,” “eating disorder,” “experiencing vertigo, dyspnea, cold sweat, or muscle rigidity when similar situations arise,” “being overly cautious in similar situations,” and “consideration of a career change or job change.” Further, to quantitatively assess PSI impacts, PTSD and PTED scale scores (see the following section for details) were also collected. Finally, for socio-demographic information, participants' gender, age group, and career level (time since obtaining their medical license) were collected. The full questionnaire is included in the Supplementary Materials (under
Supplementary Data 1).
PTSD and PTED scales
We used a PTSD scale designed to assess past and current impacts of PSI-related trauma.
19 This scale comprises 30 items, and each item is rated using a six-point scale (1 = “strongly disagree,” 2 = “disagree,” 3 = “slightly disagree,” 4 = “slightly agree,” 5 = “agree,” and 6 = “strongly agree”). For PTED, a scale based on an existing 19-item PTED scale that was originally designed to assess the occurrence of serious adverse events in life
20 was used, to which we added items to assess the impact of the most memorable PSI. Each item was rated using a five-point scale (1 = “strongly disagree,” 2 = “disagree,” 3 = “slightly disagree,” 4 = “agree,” and 5 = “strongly agree”).
Administration of the survey
An anonymous, self-report online survey was conducted for approximately five months, from October 2018 to February 2019. To ensure that the participants would have an appropriate understanding of the terms beforehand, we presented definitions of patient-safety-related terms prior to the survey.
162122 To promote the survey, we posted a promotional article on an online blog, and participants were recruited via snowball sampling, which involved encouraging the study participants to recruit future participants from among their acquaintances. To prevent duplicate participation, which can occur in online surveys, only one participation was allowed per IP address.
Analysis
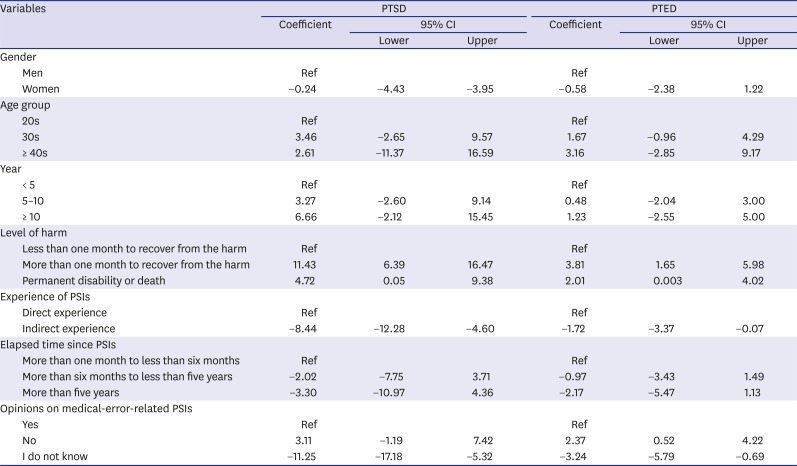
To measure socio-demographic factors and the characteristics of the PSIs experienced by physicians, frequency analysis was performed on the corresponding responses. A chi-square test was used to determine whether there were differences between direct and indirect PSI experience in regard to the PSI-induced difficulties reported. Meanwhile, to analyze the PTSD and PTED scale results, for each scale the items were summed and converted into a respective total score. The differences in PTSD and PTED scores for both direct and indirect experience of PSI were then analyzed using independent t-tests. Furthermore, the factors related to PTSD and PTED scores were identified using linear regression. In the linear regression analysis, the PTSD and PTED scores were set as the dependent variables, and participants’ demographic factors (gender, age group, career), type(s) of PSI(s) experienced (direct or multiple experience, indirect experience), severity of harm involved regarding most memorable PSI, time since most memorable PSI, and opinion regarding whether medical error was involved were set as the independent variables.
Stata/SE13.1 (StataCorp, College Station, TX, USA) was used for all analyses. Statistical significance was set at P < 0.05.
Ethics statement
This study was approved by the Institutional Review Board (IRB) of the University of Ulsan Hospital (IRB No. 2018-07-003). Participants were informed about the purpose of the study, and only those individuals who provided informed consent joined this study.
DISCUSSION
In this study, we sought to examine the problem of second victims of PSIs in Korea by conducting an anonymous, self-report online survey on physicians who had experienced PSIs. Specifically, using data for 895 physicians, we analyzed PSI characteristics, such as types of PSIs experienced, levels of harm involved, and difficulties caused by PSIs, and quantitatively analyzed such difficulties based on PTSD and PTED scores. This study is the first to highlight the current status of the second-victim problem among physicians in Korea, and our findings are meaningful in that they underline the need for support for second victims, and also because they draw societal attention to second victims. In particular, this study is significant, as it is the first large-scale study of second victims of PSIs to be conducted in an Asian country.
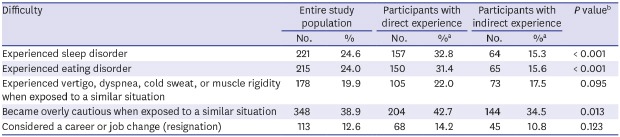
A considerable number of the physicians who responded to this study experienced PSI-induced difficulties. Of our participants, 24.6% and 24.0% experienced a sleep disorder and eating disorder, respectively, as a result of a PSI. Further, 12.6% considered changing their career or job (resignation). Although there is limited comparability, a previous study reported that approximately 7%–10% of adults in Korea have insomnia
23; thus, we can infer that physicians who experience a PSI encounter substantial psychological difficulties due to the incident. Our findings support those of the abovementioned systematic review, which reported that second victims experience psychological difficulties, such as guilt, fear, and anxiety; physical difficulties, such as fatigue, insomnia, reduced appetite, and headaches; and deviant behaviors, such as drinking and smoking.
6 As the adage “time heals all wounds” suggests, people may feel that, as the memories of an incident fade over time, the trauma also dissipates; however, our linear regression analysis showed that the participants’ PTSD and PTED scores did not significantly lower over time. In other words, it should be noted that the PSI-related difficulties experienced by second victims are not simply resolved with the passage of time. In addition, our linear regression results regarding PTSD and PTED scores showed that it should not be assumed that physicians with longer careers have fewer difficulties.
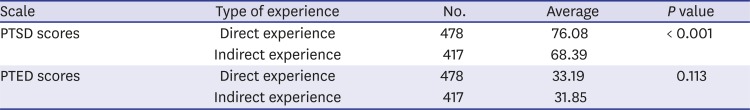
In particular, this study confirmed that physicians' difficulties can differ depending on the type of PSI they experience. For example, whereas 32.8% of participants who were directly exposed to a PSI developed a sleep disorder, only 15.3% of those who were indirectly exposed to a PSI developed a sleep disorder, showing a statistically significant difference between the two groups. In addition, other difficulties, such as developing an eating disorder or seeking to change career or job (resignation), significantly differed depending on the type of PSI exposure. More specifically, participants who had direct exposure to PSIs had significantly higher PTSD scores (76.08) than did participants who had indirect exposure to PSIs (68.39; P < 0.001). Meanwhile, although statistically insignificant, the mean PTED score was also 1.37 higher in the former group (33.19) than in the latter group.
Linear regression analysis of PTSD and PTED scores also showed that the PTSD scores were lower (by 8.44; 95% CI, −12.28 to −4.60) in those with an indirect exposure to PSIs compared to those with direct exposure. Moreover, PTED score was statistically significantly lower (by 1.72; 95% CI, −3.37 to −0.07) among those with indirect exposure when compared to those with direct exposure. These results show that physicians who directly experience a PSI encounter substantial difficulties. Further, as the linear regression results suggest that the level of difficulties increases as the severity of harm caused by the PSI increases, devising support measures for second victims is a priority. However, the fact that the linear regression results show no clear volume-outcome relationship where the greater the level of harm due to PSIs, the higher the PTSD and PTED scores, will need to be discussed further. It is possible to hypothesize that participants who experienced PSIs that caused permanent disability or death might have less impact because it was an indirect experience rather than a direct experience. However, there was more direct experience than indirect experience, when looking at the types of experience of participants who experienced PSIs that resulted in permanent disability or death (not included in the result table). Future studies will need to look more closely at differences in symptoms depending on the types of PSIs experience and the level of harm.
Despite this, support from health-care institutions, as well as from coworkers, for second victims remains low.
71011 In particular, as second victims' acceptance of and coping with a PSI can be influenced by their coworkers' attitude toward the incident,
7 it is important for healthcare institutions to introduce guidelines for medical professionals regarding means of treating a coworker who has directly experienced a PSI. In recent years, healthcare institutions in several countries, particularly the United States, have developed and implemented programs that aim to help second victims overcome psychological difficulties.
242526 For instance, the “Resilience in Stressful Events” second victim support program at the Johns Hopkins Hospital recruits and trains peer supporters, who then contact second victims to provide emotional support.
24 There is a need for similar programs in Korea, and our findings, along with the results of a prior qualitative study on second victims,
7 could be utilized to inform the development of such programs. If such programs are implemented, medical professionals who have directly experienced a PSI, and those who have indirectly experienced a PSI that led to severe harm, could be prioritized as participants.
Among the various potential measures for mitigating the psychological difficulties experienced by second victims, more attention should be paid to actions to be taken after a PSI. One possible method in this regard is “disclosure of patient safety incidents,” which is a recommended series of actions for addressing a PSI that has already occurred. Such disclosure has been defined as follows: “when a patient safety incident occurs, medical professionals preemptively explain the incident to the patients and their caregivers, express sympathy and regret for the incident, deliver an apology and compensation appropriately, if needed, and promise to prevent its recurrence.”
27 One of the benefits of disclosing PSIs is that this can reduce medical professionals' sense of guilt
27; thus, implementing disclosure of PSIs as a policy in healthcare institutions would be helpful for alleviating the psychological impact of PSIs on second victims. This underlines the importance of educating and training medical professionals regarding disclosure of PSIs, in addition to providing support programs for second victims.
28
This study has some limitations. First, the participants' PSI-related experience and difficulties were examined through a cross-sectional survey, so we could not observe how PSI impacts change over time. Moreover, recall bias may have occurred. In the future, PSI experience and impacts should be continuously investigated, and medical professionals who have serious symptoms and difficulties as a result of PSIs should be followed-up.
29 Second, the participants were recruited through an online survey, so there may be an issue regarding the representativeness of the sample. Furthermore, the collection of participants' socio-demographic information was minimized only by gender, age, and time since obtaining medical license in order to obtain candid responses from survey participants. It would be meaningful to conduct similar studies with more representative and diverse participants, considering physicians' positions and roles. Third, a systematic review of the second victims reported more diverse symptoms,
6 this study focused mainly on the five representative difficulties of the second victims. In future studies, it is necessary to identify more diverse symptoms of second victims, such as guilt feelings and deviant behaviors. Fourth, we could not obtain opinions regarding the specific contents of support programs for second victims. As this study highlighted the need for support programs for second victims, subsequent studies should investigate needs regarding the structure and management of such programs for second victims. In particular, it is necessary to further highlight the need for the supporting program by collecting information about variables that may be related to the impact of the PSIs, such as the appropriateness of the response of colleagues, superiors, and medical institutions to the PSIs.
Despite the limitations listed above, the novelty of this study is that it quantitatively assessed the PSI-related experience and difficulties of physicians in Korea using a large-scale survey. This study found that a considerable number of physicians are experiencing PSI-induced physical symptoms and behavioral responses, and that the severity of their conditions worsens depending on the type of incident and level of harm involved. We hope that this study initiates active discussion regarding support programs for second victims, and also fuels consideration of the development of a system for addressing PSIs that have already occurred,
30 such as the disclosure of PSI policy.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download