Abstract
BACKGROUND/OBJECTIVES
SUBJECTS/METHODS
RESULTS
CONCLUSIONS
Figures and Tables
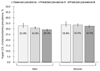 | Fig. 1Observed and predicted estimates of hyper-LDL-cholesterolemia prevalence calculated using the 2016 Korea National Health and Nutrition Examination Survey data.The ‘predicted prevalence A’ indicates an estimate calculated using the final models presented in Table 3. The ‘predicted prevalence B’ indicates an estimate obtained when considering a 2 kg/m2 reduction in the body mass index of obese persons in the given models. The vertical line on the bar indicates the 95% confidence interval. Logistic regression analysis was used.
|
 | Fig. 2Association between % of calories from fat and hyper-LDL-cholesterolemia prevalence in 38394 adults aged 30 years or older.The multivariate odds ratios of hyper-LDL-cholesterolemia prevalence were estimated after adjustment of variables presented in Table 2, except for consumption of high-fat foods. The multivariate odds ratios (number of subjects) are shown inside the bars with the 95% confidence interval depicted as a vertical line on the bar. Logistic regression analysis was used and p-value for trend was obtained when median values of % of calories from fat for each category were fitted.
|
Table 1
1. Comparison of age and age-adjusted values of variables in 41,073 adults aged 30 years or older across survey cycles of the KNHANES data and the KOSIS data

KNHANES, Korea National Health and Nutrition Examination Survey; KOSIS, Korean Statistical Information Service.
Hyper-LDL-cholesterolemia is defined as having serum LDL cholesterol levels ≥130 mg/dL.
1) Based on monthly household income and the number of family members
2) Consumption of an alcoholic beverage at least once a month over the previous year
3) Among women
Number of participants (year): 3,940 (2005), 2,204 (2007), 4,803 (2008), 5,281 (2009), 4,423 (2010), 4,527 (2011), 4,258 (2012), 3,881 (2013), 3,832 (2014), 3,924 (2015)
P for trend was obtained using the Chi-square test for trend (Cochran-Armitage test) and linear trend analysis in ANOVA.
Table 2
Age-adjusted odds ratios for variables in the association with hyper-LDL-cholesterolemia prevalence over a 10-year period in 15,634 male and 22,760 female adults

OR, Odds ratio; CI, confidence interval.
1) The reference of a binary variable is expressed as opposed to the variable itself.
Number of participants (year): 3,882 (2005), 2,144 (2007), 4,616 (2008), 5,041 (2009), 4,149 (2010), 4,182 (2011), 3,917 (2012), 3,550 (2013), 3,467 (2014), 3,446 (2015)
Logistic regression analysis was used.
Table 3
Results of stepwise logistic regression analysis for the association between significant factors and hyper-LDL-cholesterolemia prevalence over a 10-year period in 15,634 male and 22,760 female adults

OR, Odds ratio; CI, confidence interval.
1) Multivariate OR was estimated in the model including variables with a significance level of P < 0.05. The variables were selected based on the results of stepwise logistic analysis including all variables presented in Table 2, except for fat intake.
2) The reference of a binary variable is expressed as opposed to the variable itself.
Number of participants (year): 3,882 (2005), 2,144 (2007), 4,616 (2008), 5,041 (2009), 4,149 (2010), 4,182 (2011), 3,917 (2012), 3,550 (2013), 3,467 (2014), 3,446 (2015)
Logistic regression analysis was used.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download