Abstract
Background
Methods
Results
Conclusion
Notes
References
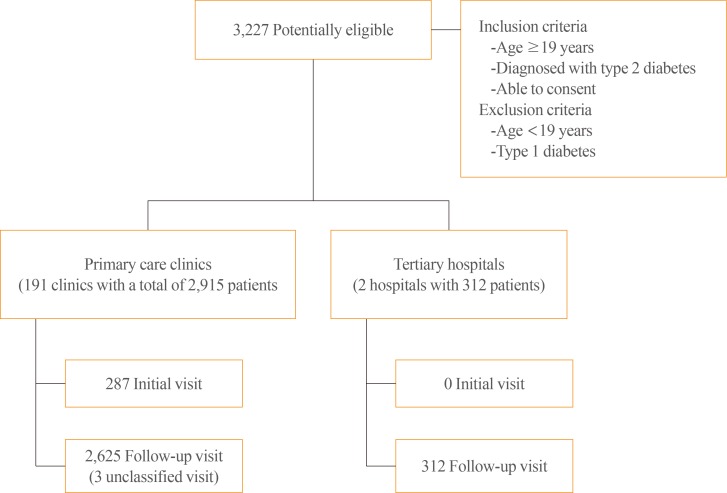
Fig. 2
Comparison of the screening done for microvascular complications at primary care clinics versus the tertiary hospitals. aReferral for screening tests within 24 months.
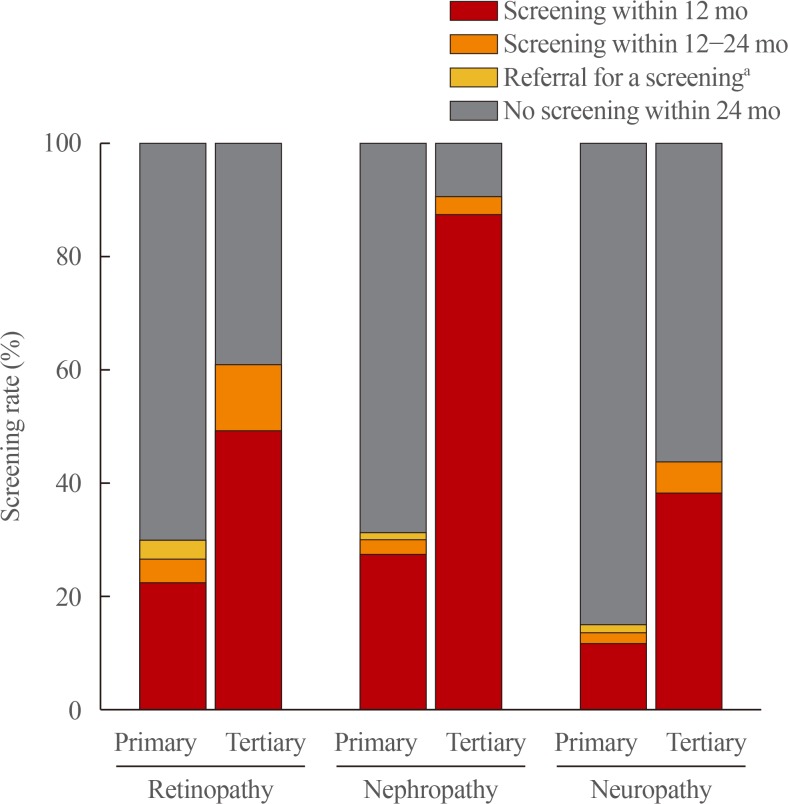
Table 1
General Characteristics of the Study Population
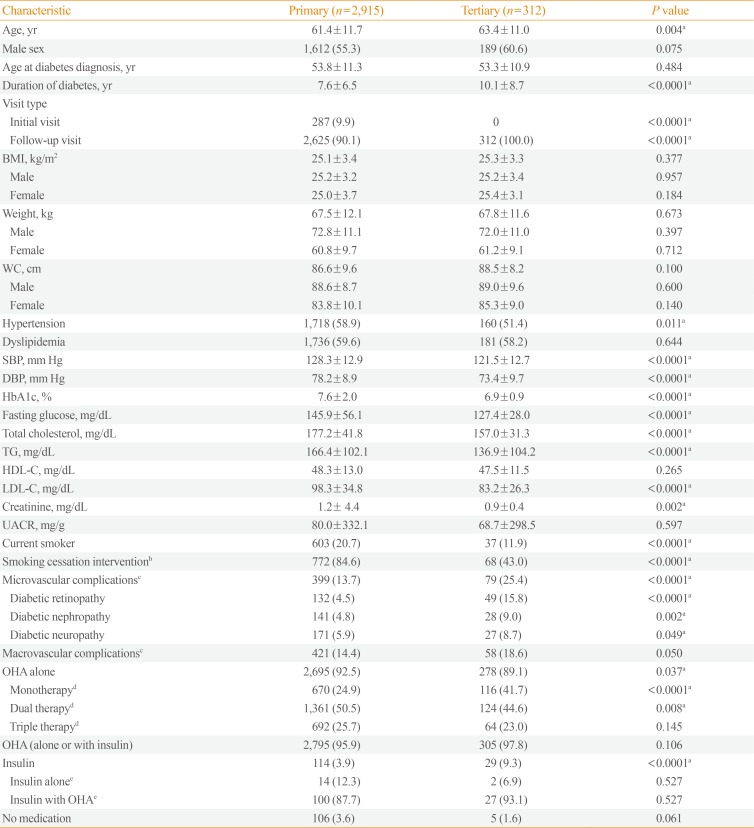
Values are expressed as mean±standard deviation or number (%). P values refer to the unpaired t test or the chi-square test.
BMI, body mass index; WC, waist circumference; SBP, systolic blood pressure; DBP, diastolic blood pressure; HbA1c; hemoglobin A1c; TG, triglyceride; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; UACR, urinary albumin-to-creatinine ratio; OHA, oral hypoglycemic agent.
aValues with statistical significance; bThe denominator is the total number of current smokers and those who had a history of smoking after the diagnosis of diabetes; cExcludes those with multiple choices/answers; dThe denominator is the number of people taking OHAs only; eThe denominator is the total number of people taking insulin with or without OHAs.
Table 2
Screening for Diabetic Microvascular Complications
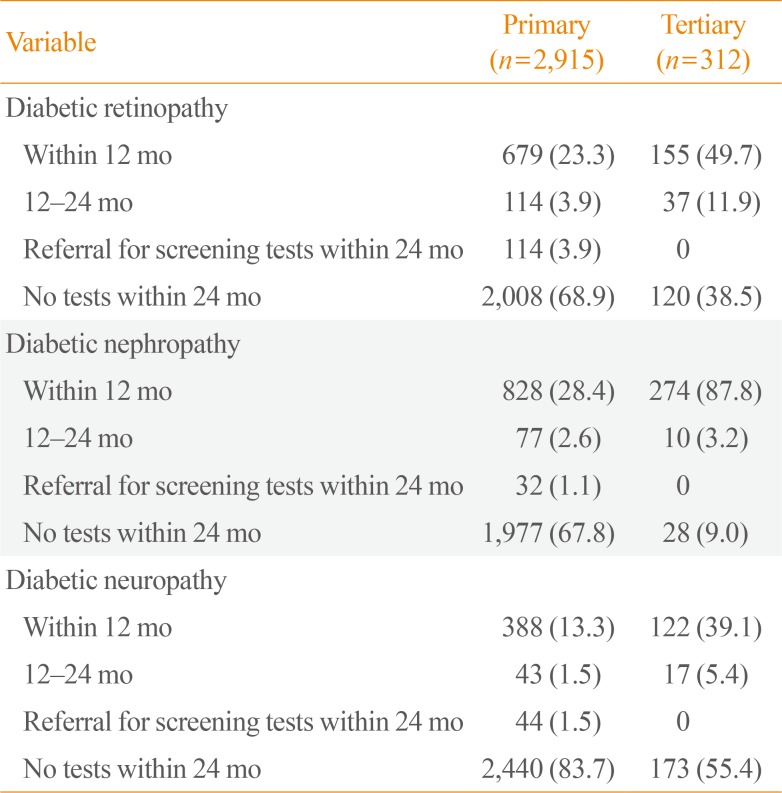
Table 3
Metabolic Target Achievement Rate
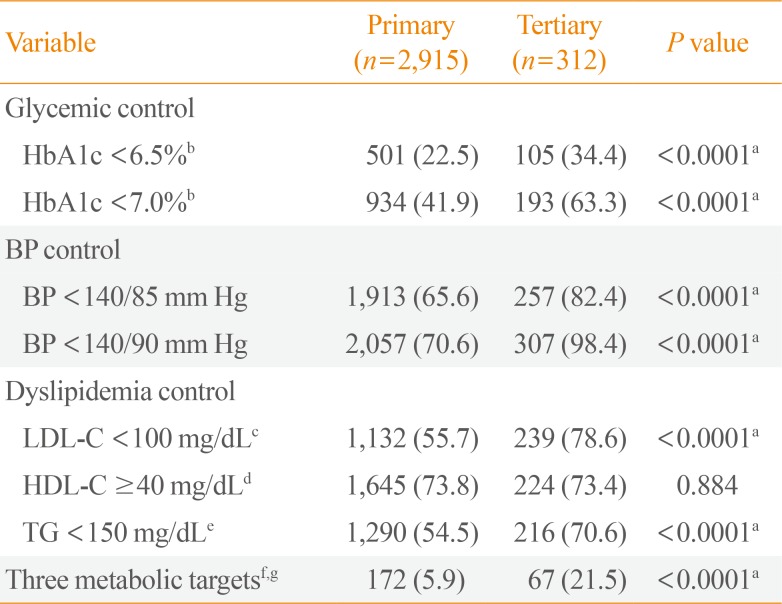
Values are expressed as number (%). P values refer to the chi-square test.
HbA1c, hemoglobin A1c; BP, blood pressure; LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol; TG, triglyceride.
aValues with statistical significance; bThe denominator is the number of people who had HbA1c testing within 3 months prior to enrollment (n=2,224); cThe denominator is the number of people who had LDL-C testing within 12 months prior to enrollment (n=2,031); dThe denominator is the number of people who had HDL-C testing within 12 months prior to enrollment (n=2,228); eThe denominator is the number of people who had TG testing within 12 months prior to enrollment (n=2,366); fThe denominator is the total number of subjects in each group; gThree metabolic targets: HbA1c <6.5%, BP <140/85 mm Hg, and LDL-C <100 mg/dL.
Table 4
Frequency and Method of Tests for Diabetes Management
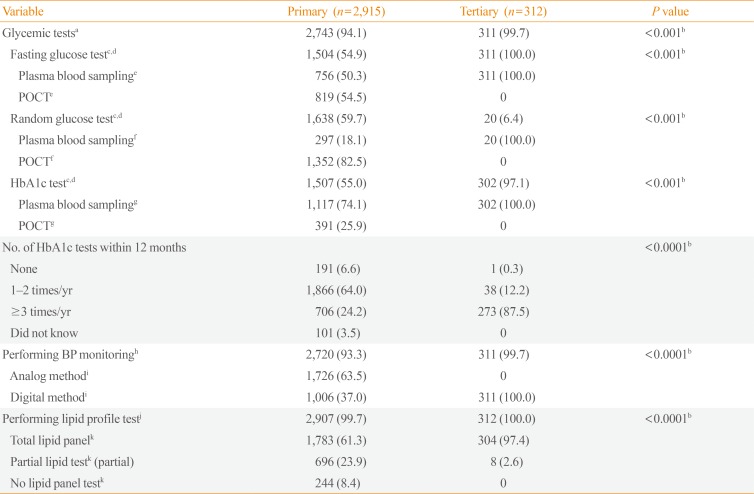
Values are expressed as number (%). P values refer to the chi-square test.
POCT, point of care test; HbA1c, hemoglobin A1c; BP, blood pressure.
aFor glycemic control, patients were asked if they had blood tests on the day of the visit; bValues with statistical significance; cThe denominator is the number of subjects who received a fasting glucose test; dIncludes those with multiple choices/answers; eThe denominator is the number of subjects who received a fasting glucose test; fThe denominator is the number of subjects who received a random glucose test; gThe denominator is the number of subjects who received a HbA1c test; hFor BP monitoring, patients were asked if they had a BP measurement on the day of the visit; iThe denominator is the number of subjects who received BP monitoring on the day of visit; jFor the lipid profile test, patients attending an initial visit were asked if they had a blood test for their lipid profile on the day of the visit and patients attending a follow-up visit were asked if they had a blood test for their lipid profile within 12 months; kThe denominator is the number of subjects who received lipid profile tests within 12 months.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download