| Ann Occup Environ Med. 2019;31(1):7. English. Published online Mar 8, 2019. https://doi.org/10.1186/s40557-019-0287-7 | |
| © The Author(s). 2019 | |
|
Ho Lee,
Seong-yong Cho, | |
| Department of Occupational and Environmental Medicine, Soonchunhyang University Gumi Hospital, 179, 1gongdan-ro, Gumi, Gyeongsangbuk-do Republic of Korea.
| |
| Received Oct 7, 2018; Accepted Feb 10, 2019. | |
|
This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated. | |
|
Abstract
| |
|
Background
The objective of this study was to compare differences in lifestyle diseases, musculoskeletal pain, psychosocial stress, and self-health awareness according to gender in Korean farmers.
Methods
The study population comprised 436 farmers residing in rural areas in Korea. A self-administered questionnaire was used to survey demographic characteristics, health-related behaviors, and musculoskeletal pain. The psychosocial well-being index short form (PWI-SF) was used to survey psychosocial stress, and the 12-item short form health survey (SF-12) was used to survey self-health awareness. In addition, a clinical examination was performed for each participant, and lifestyle diseases were identified through a health checkup.
Results
Among lifestyle diseases, females showed a significantly higher proportion than males for metabolic syndrome (OR: 4.57 [95% CI, 1.67–12.51]). For musculoskeletal pain, females again showed significantly higher proportion than males for hand pain (OR: 16.79 [95% CI, 3.09–91.30]), and pain in at least one body part (OR: 2.34 [95% CI, 1.16–4.70]). For psychosocial stress, females showed a significantly higher proportion than males for high-risk stress (OR: 3.10 [95% CI, 1.17–8.24]). Among the items in self-health awareness, females showed significantly higher proportion than males for mental component score (MCS) (OR: 3.10 [95% CI, 1.52–6.31]) and total score (OR: 2.34 [95% CI, 1.11–4.90]).
Conclusions
For all items that showed significant differences, females showed higher proportion than males, which indicates that female farmers tended to have poorer overall health than male farmers. Therefore, specialized programs will have to be developed to improve the health of female farmers. |
|
Keywords: Farmer; Gender; Health status; Lifestyle diseases; Musculoskeletal pain; Psychosocial stress; Self-health awareness |
|
|
Background
|
The rural population of Korea has declined sharply, from 10.8 million in 1980 to 2.4 million in 2017. During this time, young people from rural areas had relocated to urban areas, creating an aging society in rural regions. This phenomenon has created a shortage of labor in younger age groups, while increasing the intensity of labor for elderly and female farmers [1, 2].
Farming, which is known to be a dangerous occupation for both males and females, has unique characteristics that are different from other occupations due to the characteristics and behaviors of farmers, their working environment, and organizational structure [3]. Moreover, farmers do not properly apply the safety rules, and their financial situation is also unstable [4]. In Korea, occupational injuries within the farming sector have higher-than-average accident rates reported than other occupations [5, 6]. In addition, the basic living conditions of Korean farmers are much poorer than those living in urban areas due to excessive physical labor, increase in the number of female farmers, lack of education, poor hygienic environment, apathy towards health, and low socioeconomic status. They also experience difficulties in the utilization of healthcare facilities. Furthermore, they must also participate in other outdoor and household work due to a shortage of labor in farming areas. The physical and mental functions of farmers tend to deteriorate as a consequence [7, 8, 9].
A study in 2009 compared the proportion of musculoskeletal and chronic diseases between Korean farmers and other occupational groups; it found that both male and female farmers showed a higher proportion of musculoskeletal disease, while female farmers showed a significantly higher proportion of hypertension than other occupational groups [10]. In a study conducted in 2016 on the proportion of musculoskeletal pain and the characteristics of Korean farmers, female farmers showed a significantly higher risk of pain in the shoulders, hands, lower back, and legs compared to male farmers [11]. A study in 2015 examined the health status and related factors of farmers, using the 12-item short form health survey (SF-12) to evaluate self-health awareness; the results showed that females had a lower mental component score (MCS) than males [12].
As shown, studies have compared differences in the risk or proportion of specific diseases between male and female farmers or differences in disease proportion between farmers and other occupational groups. However, there have been no studies that systematically compare the physical and mental state of farmers according to gender. Accordingly, this study aimed to compare differences in lifestyle diseases, musculoskeletal pain, psychosocial stress, and self-health awareness of Korean farmers according to gender.
|
Methods
|
Subjects
The study area was set as rural areas in Gyeongsangbuk-do Province in Korea. The study population consisted of farmers residing in a total of 11 areas: 3 areas in 2015, 4 in 2016, and 4 in 2017. Among the 458 people who participated in both a questionnaire survey and health checkup conducted by the National Health Insurance Service (NHIS), 436 people were included in the final study population, after excluding 22 people who did not work in farming or provided incomplete responses to the questionnaire.
Survey content
A self-administered questionnaire was used to survey demographic characteristics, health-related behaviors, and musculoskeletal pain. The specific details were as follows:
Demographic characteristics, health-related behaviors, and clinical examination
The demographic characteristics of the subjects included: gender, age, working duration, main crops, presence of family members other than the spouse, spouse, income, and housework time. Main crops were categorized as grains, vegetables, fruits, livestock, and other. Spouse was categorized as “Yes” or “No” (single, divorced, or widowed), and presence of family members other than the spouse was categorized as “Yes” or “No”. Income was categorized as < 10 million won, 10–24 million won, 25–49 million won, and ≥ 50 million won, and housework was categorized as 0, < 2, and ≥ 2 h/day.
Alcohol drinking, smoking, and exercise status were surveyed as health-related behaviors. Alcohol drinking status was categorized as nondrinker, once/week, and two or more times/week. Smoking status was categorized as nonsmoker, ex-smoker, and current smoker. Exercise status was categorized as “Yes,” if the subjects performed moderate to vigorous exercise or walking at least 5 days a week and “No,” if otherwise.
A clinical examination was performed on each participant through a health checkup to measure height, weight, waist circumference, body mass index (BMI), blood pressure, hemoglobin, fasting blood glucose (FBS), serum lipids, and serum liver enzymes. Obesity was defined based using BMI, with BMI < 25 kg/m2 as normal and ≥ 25 kg/m2 as obese [13]. Blood pressure, hemoglobin, FBS, serum lipids, and serum liver enzymes were defined as abnormal when a disease was suspected or diagnosed based on the standards of the NHIS in Korea. The details are as follows. Hypertension was defined as systolic pressure ≥ 140 mmHg or diastolic pressure ≥ 90 mmHg during blood pressure measurement, or being treated for hypertension. Diabetes mellitus was defined as FBS ≥126 mg/dL, or being treated for diabetes mellitus. Dyslipidemia was defined as total cholesterol ≥240 mg/dL, triglyceride ≥200 mg/dL, high-density lipoprotein cholesterol (HDL-C) < 40 mg/dL, low-density lipoprotein cholesterol (LDL-C) ≥160 mg/dL, or being treated for dyslipidemia. Anemia was defined as hemoglobin < 13 mg/dL for males and < 12 mg/dL for females. For serum liver enzymes, aspartate aminotransferase (AST), alanine aminotransferase (ALT), and gamma-glutamyltransferase (γ-GTP) levels were measured, and AST ≥50 IU/L, ALT ≥45 IU/L, or γ-GTP ≥78 IU/L for males and ≥ 46 IU/L for females were considered abnormal [14].
For metabolic syndrome, the National Cholesterol Education Program’s Adult Treatment Panel III (NCEP ATP III) was applied for metabolic syndrome, along with the International Diabetes Federation (IDF) definition in 2009 for waist circumference. Those who satisfied 3 or more of the following conditions were considered to have metabolic syndrome: systolic blood pressure ≥ 130 mmHg, diastolic blood pressure ≥ 85 mmHg, or being treated for hypertension; FBS ≥100 mg/dL or being treated for diabetes mellitus; waist circumference ≥ 90 cm for males and ≥ 80 cm for females; triglyceride ≥150 mg/dL; and HDL-C < 40 mg/dL for males and < 50 mg/dL for females [15, 16, 17].
Lifestyle diseases were identified based on these results. Lifestyle diseases refer to a disease group with onset and progression affected by lifestyle, including diet, exercise, smoking, and drinking [18]. In this study, lifestyle disease was defined as a suspected or confirmed disease in the health checkup or diagnosis with metabolic syndrome. Specifically, hypertension, diabetes mellitus, dyslipidemia, anemia, abnormal serum liver enzymes, and metabolic syndrome were checked as lifestyle diseases.
Musculoskeletal pain assessment
To evaluate musculoskeletal pain symptoms, this study used the questionnaire “Guidelines for surveys of harmful factors in tasks involving musculoskeletal loads” from the Korea Occupational Safety and Health Agency (KOSHA) CODE H-9-2016 [19]. Items included in the questionnaire were: six specific body parts (neck, shoulder, arm, hand, lower back, and leg), duration of pain, severity of pain, and frequency of symptoms in the last year. Based on the results, musculoskeletal pain was defined as moderate-to-severe pain in one or more areas that persists for at least one week or occurs more than once in a month, in accordance with Standard 2 of the National Institute for Occupational Safety and Health (NIOSH) [20].
Psychosocial stress assessment
The psychosocial well-being index short form (PWI-SF) was used as the tool for assessing psychosocial stress. The form comprised questions about physical and mental state in the past few weeks, with the total score ranging between 0 and 54 points. Higher scores indicated a higher level of psychosocial stress, with ≤8, 9–26, and ≥ 27 points defined as healthy, potential stress, and high-risk stress, respectively [21, 22].
Self-health awareness assessment
The 12-item short form health survey (SF-12) was used as the tool for assessing self-health awareness. SF-12 is an abridged version of SF-36, which can be used to measure physical component score (PCS) and sub-items, mental component score (MCS) and sub-items, and the total score. Sub-items under PCS included physical functioning (PF), role physical (RP), bodily pain (BP), and general health (GH); sub-items under MCS included mental health (MH), role emotional (RE), social functioning (SF), and vitality (VT). A higher score in each item indicated better-perceived health status for that item [23, 24, 25].
Statistical analysis
In this study, t-test and chi-square test were performed to investigate the differences in demographic characteristics, health-related behaviors, clinical examination, musculoskeletal pain, and self-health awareness between male and female farmers. A linear-by-linear association test was performed to investigate differences in psychosocial stress. In addition, multiple logistic regression analysis was performed to investigate the differences in lifestyle disease, musculoskeletal pain, psychosocial stress, and self-health awareness between male and female farmers. For psychosocial stress, healthy and potential stress of PWI-SF was set as low risk and used as the reference. For self-health awareness, the results were divided into high and low based on the median value of SF-12 scores, with the higher score group set as the reference. The adjustment variables included in multiple logistic regression analysis were age, spouse, income, housework time, alcohol drinking, smoking, exercise; they were included in the analysis because showed p-value < 0.15 in univariate analysis. We also included several other variables (i.e., work duration, main crops, presence of family members other than the spouse) associated with lifestyle disease, musculoskeletal pain, psychosocial stress, and self-health awareness in previous study [26, 27, 28, 29, 30]. All statistical analyses were performed using SPSS version 14.0 (SPSS, Inc., Chicago, IL, USA).
|
Results
|
Among demographic characteristics, the mean ages of males and females were 62.7 ± 9.21 and 60.9 ± 9.67 years, respectively. The proportion of males and females without a spouse was 8.8 and 19.0%, respectively. The proportion of males and females who did no housework was 49.0 and 1.3%, respectively, while 37.3% of males and 36.6% of females spent < 2 h/day on housework, and 13.7% of males and 62.1% of females spent ≥2 h/per day on housework. There were no differences in working duration, main crops, presence of family members other than the spouse, and income between males and females.
Among health-related behaviors, the proportion of male and female nondrinkers was 38.2 and 81.0%, respectively, while 16.7% of males and 12.9% of females drank once a week, and 45.1% of males and 6.0% of females drank two or more times a week. The proportion of male and female nonsmokers was 36.3 and 97.4%, respectively, while 31.9% of males and 1.7% of females were ex-smokers, and 31.9% of males and 0.9% of females were current smokers. There was no difference in exercise level between males and females (p < 0.05) (Table 1).
|
When comparing lifestyle diseases between males and females, proportion of diabetes mellitus was significantly lower in females (9.1%) than in males (17.2%); anemia was significantly higher in females (15.5%) than in males (6.4%); abnormal serum liver enzymes were significantly lower in females (7.8%) than in males (23.5%); and metabolic syndrome was significantly higher in females (32.6%) than in males (21.6%). Meanwhile, there were no differences in hypertension, dyslipidemia, and obesity between males and females (p < 0.05) (Table 2).
|
When comparing the complaint rate of males and females experiencing musculoskeletal pain, 5.4% of males and 12.1% of females had neck pain; 4.0% of males and 19.0% of females had hand pain; 24.8% of males and 40.1% of females had lower back pain; and 25.7% of males and 37.9% of females had leg pain. These results show a significantly higher proportion of females having neck, hand, lower back, and leg pain. Moreover, the proportion of those with pain in at least one body part was significantly higher in females (67.2%) than in males (47.0%). Meanwhile, there were no differences in the shoulder and arm pain between males and females (p < 0.05) (Table 3).
|
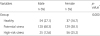
When comparing psychosocial stress between males and females using the PWI-SF, 27.1% of males and 16.7% of females belonged to the healthy group; 60.3% of males and 58.1% of females belonged to the potential stress group; and 12.6% of males and 25.2% of females belonged to the high-risk stress group (p < 0.05) (Table 4).
|
When comparing self-health awareness between males and females using the SF-12, PCS was 68.6 ± 23.5 in males and 58.3 ± 26.0 in females. MCS was 77.5 ± 18.8 in males and 67.8 ± 22.5 in females. The total score was 73.1 ± 18.9 in males and 63.1 ± 22.6 in females. Females showed significantly lower PCS, MCS, individual sub-item (PF, RP, BP, GH, MH, RE, SF, or VT) scores, and total score in the SF-12, compared to males (p < 0.05) (Table 5).
|
Multiple logistic regression analysis was performed to investigate the differences in lifestyle diseases, musculoskeletal pain, psychosocial stress, and self-health awareness between males and females, after adjusting for demographic characteristics and health-related behaviors. Among lifestyle diseases, the risk for metabolic syndrome was significantly higher in females than males (OR: 4.57 [95% CI, 1.67–12.51]). For musculoskeletal pain, females showed significantly higher risk than males for hand pain (OR: 16.79 [95% CI, 3.09–91.30]), and pain in at least one body part (OR: 2.34 [95% CI, 1.16–4.70]). For psychosocial stress, females had a significantly higher risk for high-risk stress than males (OR: 3.10 [95% CI, 1.17–8.24]). Among the items in self-health awareness, females showed significantly higher risk than males for MCS (OR: 3.10 [95% CI, 1.52–6.31]) and total score (OR: 2.34 [95% CI, 1.11–4.90]) (Table 6).
|
|
Discussion
|
In this study, the proportion of metabolic syndrome was significantly higher in females (32.6%) than in males (21.6%), and the risk of metabolic syndrome in females was 4.57 [95% CI, 1.67–12.51] times higher than in males. In a study that followed up 1095 rural residents for 5 years to measure the proportion of metabolic syndrome, females showed a significantly higher proportion of 46.4/1000 person-years, compared to 30.0/1000 person-years for males, which is consistent with the present study [31]. A previous study of 91 farmers found that the proportion of metabolic syndrome was lower in females (42.9%) than in males (51.4%), which is contradictory to the present study [32]. The previous study did not include people being treated for hypertension and diabetes mellitus in the criteria for metabolic syndrome. This is postulated to be the reason for the difference from the present study. Another study that followed up 460 rural residents for 5 years also found the proportion of metabolic syndrome to be 37.9/1000 person-years in males and 18.9/1000 person-years in females [33]. The present study included only farmers, whereas the previous study included all rural residents; it is presumed that the different findings may be attributable to 47.4% of the subjects in the previous study being unemployed. The reason why females showed a higher risk of metabolic syndrome in the present study may be attributed to several factors. First, pregnancy and childbirth have been reported to cause metabolic disorders accompanied by weight gain, increased abdominal obesity, and postpartum depression [34, 35, 36]. Since the females who participated in the present study had an average age in their 60s, the fact that most have experienced pregnancy and childbirth may have influenced the results. Second, previous studies have reported a statistically significant positive correlation between BMI and risk of metabolic syndrome [37, 38], and other studies have presented obesity as the most sensitive indicator of metabolic syndrome [39, 40]. It is presumed that females having significantly higher risk of obesity than males in in the present study may have influenced the results.
Chi-square test results for musculoskeletal pain showed that a significantly higher proportion of females had neck, hand, lower back, and leg pain compared to males. Multiple logistic regression analysis results also showed that females had a higher risk of pain than males; specifically, the odds ratios were 16.79 [95% CI, 3.09–91.30] for hand pain, and 2.34 [95% CI, 1.16–4.70] for pain in at least one body part. A previous study that investigated the risk and characteristics of musculoskeletal pain in 1013 Korean farmers found that females had a significantly higher risk of pain than males, with odds ratios of 1.77 [95% CI, 1.18–2.64] for shoulder pain, 3.88 [95% CI, 2.35–6.42] for hand pain, 2.13 [95% CI, 1.39–3.24] for lower back pain, and 1.92 [95% CI, 1.29–2.86] for leg pain [11]. The higher overall risk of pain in females shown in the previous study is similar to the present study, but the pain areas were different. This difference is postulated to be due to the present study applying NIOSH Standard 2, whereas the previous study applied NIOSH Standard 1. In a study of musculoskeletal pain in 220 Indian rice farmers, the risk of pain in females was significantly higher than that of males for shoulder, hand, lower back, and knee pain [41]. For the farmers in the present study, fruits were the main crop, while the main crop in the previous study was rice. Farming different crops is predicted to lead to differences in posture while farming, which would, in turn, lead to differences in the location of pain. In the present study, female farmers showed higher risk than males for hand pain. This may be because female Korean farmers often perform tasks that require repetitive use of the hands and fingers [27, 28]. Moreover, females in the present study showed significantly higher time spent on housework than males and, as a result, the working time, including housework, may be higher in female farmers than in male farmers. In a study that investigated the difference in musculoskeletal disorders according to gender among 358 Korean farmers, the average daily working time for female farmers (9.6 h) was longer than that of male farmers (9.2 h). Since the female farmers also tended to be solely responsible for housework, they had a greater burden [27, 28]. It is postulated that female farmers showed a higher risk of hand pain than males because housework mostly involves the use of the hands.
For psychosocial stress assessed using the PWI-SF, the chi-square tests results showed that a higher proportion of females had potential stress and high-risk stress than males. Further, females had a higher risk for high-risk stress than males (OR: 3.10 [95% CI, 1.17–8.24]). In a 2017 study that used the PWI-SF to analyze psychosocial stress factors in 3631 rural residents, females had a significantly higher risk for high-risk stress than males (OR: 2.34 [95% CI, 1.88–2.92]), which is similar to the present study [42]. In a 2011 study on 1737 rural residents, psychosocial stress was significantly higher in females than in males, which was also similar to the present study [43]. These results are postulated to reflect the characteristics associated with cultural differences regarding gender roles in Korean society and the patriarchal characteristics of Korean rural areas [44, 45]. The relatively longer working hours for female farmers are also presumed to act as a burden, resulting in increased stress [28].
For self-health awareness assessed using the SF-12, females showed significantly lower scores than males for PCS, MCS, total score, and 8 sub-items, indicating that females tended to perceive their health to be poor compared to males. Previous studies also showed similar results, where females showed lower perception of their overall self-health than males did [25, 46, 47]. Nettleton explained that performing the dual task of work and housework has a negative effect on the health of females [48]. Meanwhile, MacIntyre explained that symptoms are more readily noticed in females since they tend to be well aware of their own health, whereas males do not accept the fact that they may be ill and perceive their health to be better than it actually is [49]. In such cases, males may show relatively better scores than their actual health status, which may be the reason for the lower perception of their self-health in females than males. In other words, itis presumed that the responses to the questions might contain over- or under-estimations.
The present study has several limitations. First, the study population consisted of people from 11 rural areas in Gyeongsangbuk-do Province but, because of the small sample size from each area, it is difficult to generalize the findings for all farmers. Second, there was no investigation of the life expectancy of male and female farmers in Korea. The life expectancy of females in the general population in Korea was found to be 85.6 years in 2017, which was longer than the 79.5 years for males [2]. In a previous study conducted in the United States, the life expectancy of females in rural areas in 2005–2009 was 79.7 years, which was longer than that of males aged 74.1 years [50]. In the present study, the health status of female farmers was poorer than was that of males, but we could not confirm if they had a longer life expectancy than did males despite their poorer health status.
Despite these limitations, this study was able to compare lifestyle diseases, musculoskeletal pain, psychosocial stress, and self-health awareness to identify differences in the physical and mental health status of farmers according to gender. It also demonstrated that female farmers had higher health risks than male farmers, indicating that female farmers tend to have poorer health than male farmers. In addition, this study is significant in recognizing these differences and thus it can be used as basic data for the development of a specialized health promotion program for female farmers.
|
Conclusions
|
While there have been many studies on the specific health issues of farmers, there have been almost no studies to date that have examined the overall difference in the health of farmers according to gender. This study was conducted to investigate the differences in health status between male and female farmers. The items that showed differences in the health status of farmers according to gender were metabolic syndrome, musculoskeletal pain, psychosocial stress, and self-health awareness. For all items that showed significant differences, female farmers showed higher risk than male farmers; thus, female farmers tended to have poorer overall health than male farmers. Therefore, when developing health promotion programs for farmers in the future, specialized programs will have to be developed to improve the health of female farmers.
|
Abbreviations
|
| ALT | Alanine aminotransferase |
| AST | Aspartate aminotransferase |
| BMI | Body mass index |
| BP | Bodily pain |
| CI | Confidence interval |
| FBS | Fasting blood sugar |
| GH | General health |
| HDL-C | High-density lipoprotein cholesterol |
| IDF | International Diabetes Federation |
| KOSHA | Korea Occupational Safety and Health Agency |
| KRW | South Korean won |
| LDL-C | Low-density lipoprotein cholesterol |
| MCS | Mental component score |
| MH | Mental health |
| NCEP ATP III | National Cholesterol Education Program’s Adult Treatment Panel III |
| NHIS | National Health Insurance Service |
| NIOSH | National Institute for Occupational Safety and Health |
| OR | Odds ratio |
| PCS | Physical component score |
| PF | Physical functioning |
| PWI-SF | Psychosocial well-being index short form |
| RE | Role emotional |
| RP | Role physical |
| SF | Social functioning |
| SF-12 | 12-item short form health survey |
| γ-GTP | Gamma-glutamyltransferase |
|
Acknowledgements
|
Not applicable.
Funding
This work was supported by the Soonchunhyang University Research Fund.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
|
Authors’ contributions
|
HL was responsible for the study design, data analysis, interpretation of the data, and drafting of this manuscript. SYC played a key role in the data collection, study design, interpretation of the data, and revision of the manuscript. JSK helped to collect and analyze the data. SYY and BIK helped to collect and interpret the data. JMA and KBK performed data interpretation and revised the manuscript. All the authors have read and approved the final manuscript.
Ethics approval and consent to participate
Written informed consent was obtained from participants.
Ethical approval was obtained from the Institutional Review Board (IRB) of Soonchunhyang University Hospital in Seoul (IRB number: Medicine 2018–06).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
|
References
|
| 1.. | Park JS, Oh YJ. The effect of health promotion program on self efficacy, health problems, farmers syndrome and quality of life of the rural elderly. J Korean Acad Adult Nurs 2006;18(1):10–21. |
| 2.. | Korean statistical information service. http://kosis.kr/statisticsList/statisticsListIndex.do?menuId=M_ |
| 3.. | Cordes DH, Rea DF. Farming: a hazardous occupation. Occup Med 1991;6(3):327–334. [pmid: 1948522] |
| 4.. | Habib RR, Hojeij S, Elzein K. Gender in occupational health research of farmworkers: a systematic review. Am J Ind Med 2014;57(12):1344–1367. [pmid: 25227724] |
| 5.. | Hope A, Kelleher C, Holmes L, Hennessy T. Health and safety practices among farmers and other workers: a needs assessment. Occup Med 1999;49(4):231–235. |
| 6.. | Chae HS, Min KD, Park JW, Kim KR, Kim HC, Lee KS. Estimated rate of agricultural injury: the Korean farmers’ occupational disease and injury survey. Ann Occup Environ Med. 2014;26(1):8. [pmid: 24808945] |
| 7.. | Lee K, Lim HS. Work-related injuries and diseases of farmers in Korea. Ind Health 2008;46(5):424–434. [pmid: 18840931] |
| 8.. | Song JY, Lee YK, Lee SG, Lee TY, Cho YC, Lee DB. Farmers syndrome and their related factors of rural residents in Chungnam Province. Korean J of Rural Med 1998;23(1):3–14. |
| 9.. | Joo AR. A study on health promotion lifestyle, farmers' syndrome and related factors of workers in agricultural industry. Korean J Occup Health Nurs. 2012;21(1):37–45. |
| 10.. | Cha ES, Kong KA, Moon EK, Lee WJ. Prevalence and changes in chronic diseases among south Korean farmers: 1998 to 2005. BMC Public Health 2009;9:268. [pmid: 19638244] |
| 11.. | Min D, Baek SR, Park HW, Lee SA, Moon JY, Yang JE, et al. Prevalence and characteristics of musculoskeletal pain in Korean farmers. Ann Rehabil Med 2016;40(1):1–13. [pmid: 26949663] |
| 12.. | Park KG, Roh SY, Lee JH, Kwon SC, Jeong MH, Lee SJ. Health status and related factors in farmers by SF-12. Ann Occup Environ Med 2015;27:2. [pmid: 25750743] |
| 13.. | Kim MK, Lee WY, Kang JH, Kang JH, Kim BT, Kim SM, et al. 2014 Clinical practice guidelines for overweight and obesity in Korea. Endocrinol Metab. 2014;29(4):405–9.. |
| 14.. | Ministry of Health and Welfare of Korea. Health examination implementation guidelines. No. 2016–252. http://www.takehealth.or.kr/bbs/board.php?board=TB_ |
| 15.. | Shim JY, Kang HT, Kim SY, Kim JS, Kim JW, Kim JY. Prevention and treatment of metabolic syndrome in Korean adults. Korean J Fam Pract. 2015;5(3):375–420. |
| 16.. | Ok JH, Kim EJ, Kim SJ, Jeong SY. The relationship between metabolic syndrome components, metabolic syndrome and depression in Korean adults. Korean J Fam Pract 2017;7(6):800–806. |
| 17.. | International Diabetes InstituteIn: The Asia-Pacific perspective: redefining obesity and its treatment. Sydney: Health Communications Australia; 2000. |
| 18.. | Kang JK. Lifestyle disease. J Korean Med Assoc. 2004;47(3):188–194. |
| 19.. | Korea Occupational Safety and Health Agency. Guideline of harmful factors survey for musculoskeletal overloading works. 2016. http://kosha.or.kr/kosha/business/musculoskeletalPreventionData_ |
| 20.. | Bernard BP. National Institute for Occupational Safety and Health (NIOSH) In: Musculoskeletal disorders and workplace factors: a critical review of epidemiologic evidence for work-related musculoskeletal disorders of the neck, upper extremity, and low back. 1997. https://www.cdc.gov/niosh/docs/97- |
| 21.. | Chang SJ. Standardization of health statistical data and measurement. Seoul: the Korean society for. Prev Med. 2000.. |
| 22.. | Park JS, Kim JH. Job stress assessment methods. Seoul: Korea Medical Book; 2004.. |
| 23.. | Song JS, Park WS, Choi HS, Seo JC, Kwak YH, Kim SA, et al. Pesticide exposure of alpine agricultural workers in Gangwon-do and the measurement of their health status measured by SF-12. The Korean Journal of Pesticide Science 2005;9(4):287–291. |
| 24.. | Wang X, Guo G, Zhou L, Zheng J, Liang X, Li Z, et al. Health-related quality of life in pregnant women living with HIV: a comparison of EQ-5D and SF-12. Health Qual Life Outcomes 2017;15(1):158. [pmid: 28851384] |
| 25.. | Cha BS, Koh SB, Chang SJ, Park JK, Kang MG. The assessment of worker’s health status by SF-36. Korean J Occup Med 1998;10(1):9–19. |
| 26.. | Lee YK, Jung HS, Jhang WG. The relationship between working time and job stress. Korean J Occup Health Nurs 2006;15(2):115–125. |
| 27.. | Lee CG. Work-related musculoskeletal disorders in Korean farmers. J Korean Med Assoc 2012;55(11):1054–1062. |
| 28.. | Kim YC, Shin YS. Gender differences in work-related musculoskeletal disorders among agricultural workers. J Ergon Soc Korea 2011;30(4):535–540. |
| 29.. | Park SY. The effects of health-related factors and social networks on depressive symptoms in elderly men and women: focusing on the moderating effects of gender. Health and Social Welfare Review 2018;38(1):154–190. |
| 30.. | Hung M, Bounsanga J, Voss MW, Crum AB, Chen W, Birmingham WC. The relationship between family support; pain and depression in elderly with arthritis. Psychol Health Med 2017;22(1):75–86. [pmid: 27427504] |
| 31.. | Hwang JH, Kam S, Shin JY, Kim JY, Lee KE, Kwon GH, et al. Incidence of metabolic syndrome and relative importance of five components as a predictor of metabolic syndrome: 5-year follow-up study in Korea. J Korean Med Sci 2013;28(12):1768–1773. [pmid: 24339707] |
| 32.. | Lim S, Kwon KH, Kim EJ, Lim DS, Lim HJ, Cho SI, et al. Characteristics of metabolic syndrome and its relationship with the factors related to obesity in rural area. J Lipid Atheroscler 2004;12(4):370–380. |
| 33.. | Yoon HJ, Lee SK. The incidence and risk factors of metabolic syndrome in rural area. Journal of the Korea Academia-Industrial cooperation Society 2015;16(6):3934–3943. |
| 34.. | Loucks EB, Rehkopf DH, Thurston RC, Kawachi I. Socioeconomic disparities in metabolic syndrome differ by gender: evidence from NHANES III. Ann Epidemiol 2007;17(1):19–26. [pmid: 17140811] |
| 35.. | Seo JM, Lim NK, Lim JY, Park HY. Gender difference in association with socioeconomic status and incidence of metabolic syndrome in Korean adults. Korean J Obes 2016;25(4):247–254. |
| 36.. | Han MS. Metabolic syndrome emerging from menopause. J Korean Soc Menopause 2011;17(3):127–135. |
| 37.. | Ford ES, Giles WH, Mokdad AH. Increasing prevalence of the metabolic syndrome among U.S. adults. Diabetes Care 2004;27(10):2444–2449. [pmid: 15451914] |
| 38.. | Kim SH, Choi HS, Ji SH, Park YM, Cho KH. The relationship of the prevalence metabolic syndrome and the difference of life style in Korean adult. Korean J Fam Med. 2015;5(3):500–509. |
| 39.. | Hong WK, Kim JS, Jung JG, Kim SS, Park CI, Kim KB, et al. Alcohol and the metabolic syndrome in Korean women. J Korean Acad Fam Med 2007;28(2):120–126. |
| 40.. | Oh JD, Lee SY, Lee JG, Kim YJ, Kim YJ, Cho BM. Health behavior and metabolic syndrome. Korean J Fam Med 2009;30(2):120–128. |
| 41.. | Das B. Gender differences in prevalence of musculoskeletal disorders among the rice farmers of West Bengal. India Work 2015;50(2):229–240. [pmid: 24004755] |
| 42.. | Nam JH, Lim MS, Choi HK, Kim JY, Kim SK, Oh SS, et al. Factors increasing the risk for psychosocial stress among Korean adults living in rural areas: using generalized estimating equations and mixed models. Ann Occup Environ Med. 2017;29(1):53. [pmid: 29118991] |
| 43.. | Choi JK, Kim YA, Kim SH, Kim SH, Park JK, Koh SB, et al. The impact of social support on stress among residents in a rural area. Korean J Health Educ Promot 2011;28(1):103–113. |
| 44.. | Cho OL. Modernity and conservatism in rural families. Korean Society for Cultural Anthropology 1998;31(2):377–405. |
| 45.. | Oh GJ, Lee JM, Kil SS, Kwon KS. Community based study for stress and its related factors. Korean J Prev Med 2003;36(2):125–130. |
| 46.. | Jenkinson C, Coulter A, Wright L. Short form 36 (SF36) health survey questionnaire: normative data for adults of working age. BMJ 1993;306(6890):1437–1440. [pmid: 8518639] |
| 47.. | Park KH, Cho WH, Suh I, Park JK. Factors related to self-perceived health of young adults. Korean J Prev Med. 2000;33(4):415–425. |
| 48.. | Nettleton S. In: The sociology of health and ilness. Cambridge: Polity; 2006. |
| 49.. | Macintyre S. Gender differences in the perceptions of common cold symptoms. Soc Sci Med 1993;36(1):15–20. [pmid: 8424180] |
| 50.. | Singh GK, Siahpush M. Widening rural-urban disparities in life expectancy, U.S., 1969–2009. Am J Prev Med. 2014;46(2):e19–29.. |




 Citation
Citation Print
Print