Abstract
Orbital metastasis is a rare event, and metastatic disease affecting the extraocular muscles is an even less frequent complication of solid tumors. Herein, we report an unusual case of ptosis as the initial presentation of an invasive breast cancer. A 68-year-old woman presented with III and VI partial nerve paresis, secondary to a compressive retrobulbar mass. Magnetic resonance imaging revealed an infiltrative lesion involving the extraocular muscles. Tissue biopsy yielded a result compatible with metastasis to the orbit, with immunohistochemistry analysis suggesting breast as the primary organ. Mammography identified an area of architectural distortion; stereotactic wire-guided biopsy confirmed the result of the previous orbital biopsy. A positron emission tomography scan demonstrated disseminated disease. Palliative chemotherapy with bone-modulating agents and subsequent hormonal therapy was proposed. Unfortunately, the patient did not respond to therapy and died 38 months after diagnosis.
Orbital metastasis occurs in 2%–3% of patients with disseminated disease; notably, extraocular muscle (EOM) involvement is an even more uncommon complication of solid tumors [12]. Orbital metastasis is an unusual event in breast cancer and its presentation as an early symptom is exceptional [3]. The clinical picture is frequently nonspecific, posing a diagnostic challenge [4]. Palliative care is offered in this setting, as overall prognosis is generally poor [56]. Our case report describes an atypical presentation of breast cancer, highlighting the importance of its inclusion in the differential diagnosis of an orbital mass, particularly for patients who are middle-aged or elderly women.
A 68-year-old Caucasian woman presented with a 12-month history of horizontal diplopia, progressive unilateral ptosis, and retrobulbar tenderness. During the month prior to presentation, she also experienced fatigue and 8-kg weight loss. Physical examination revealed left ptosis with a vertical eyelid cleft of 6 mm (10 mm in the fellow eye), reduced visual acuity (20/32, Snellen visual acuity chart), and restricted horizontal eye movements, including diplopia in the conjugate look to the left. Her pupils were symmetrical and reactive to light. No relative afferent pupillary defect was noted. Slit lamp examination of the anterior segment, as well as tonometry and fundoscopy of the left eye, were unremarkable. The fellow eye presented no clinically relevant features on examination.
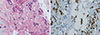
The remaining physical examination, including a breast examination, appeared normal. Complete blood count showed anemia, thrombocytopenia, and increased cancer antigen 15-3 titer (124 U/mL). Computed tomography (CT) and magnetic resonance imaging (MRI) of the orbits revealed a left intraconal infiltrative process involving the upper and lateral rectus muscles, as well as the upper oblique muscle (Figure 1). Biopsy was subsequently performed, revealing connective tissue with extensive infiltration by cords and isolated epithelial neoplastic cells (Figure 2A). Immunohistochemical analysis revealed positivity for GATA-binding protein 3, mouse monoclonal cytokeratin antibody 116, cytokeratin 7, estrogen receptors, progesterone receptors, and E-cadherin; it revealed negativity for human epidermal growth factor receptor 2 (HER2) (Figure 2B-2E). These findings suggested a likely orbital metastasis from a primary breast carcinoma.
Mammography showed an area of architectural distortion within the outer quadrant of the right breast. A stereotactic wire-guided biopsy was performed, enabling a diagnosis of invasive ductal carcinoma not otherwise specified with strong and diffuse positivity for estrogen and progesterone receptors; a 5% proliferative index (as evaluated by Ki-67); and HER2 negativity, subtype luminal A (Figure 3). A staging positron emission tomography scan (PET/CT) demonstrated diffuse lymph node and bone metastases.
Systemic palliative chemotherapy was initiated with docetaxel (75 mg/m2) and epirubicin (75 mg/m2), every 21 days for six cycles, in combination with denosumab (120 mg, monthly). A PET/CT scan after the six cycles demonstrated a favorable response; therefore, chemotherapy was suspended and hormonal therapy with anastrozole 2 mg/day was initiated, combined with denosumab. Due to hepatic metastases, a second-line chemotherapy regimen with capecitabine (1,000 mg/m2 twice per day, days 1 and 14) and vinorelbine (60 mg/m2, days 1 and 8), every 21 days, was proposed at 15 months after diagnosis. Best supportive care was chosen at 16 months after diagnosis, and the patient died at 38 months after diagnosis.
Orbital metastases from breast cancer are an uncommon event, ranging from 0% to 0.2% in the literature [78]. Indeed, the eye is a rare site for disseminated malignancy, comprising 0.07%–4.7% among patients with cancer [39]. Metastases of solid tumors to the orbit occur less often than metastases to the eye, ranging from 2% to 7% in a large series of orbital tumors [2]. Breast cancer is the most common primary tumor, responsible for up to 58% of ocular metastases, followed by the lungs, skin (melanoma), and genitourinary and gastrointestinal tracts [23810].
Metastases to ocular structures occur by hematogenous spread; therefore, the most vascularized parts of the eye are most likely to be affected. Ophthalmic disease tends to be predominately located at the uvea, particularly the choroid, comprising 81% of all ocular metastases [6711]. EOM involvement is a less frequent complication of solid tumors, comprising only 9% of orbital metastases [29]. Typically, only one muscle is affected [12]; the involvement of two or more muscles, as presented in our case, is an even more uncommon manifestation.
Typical signs and symptoms include limited ocular mobility, proptosis, palpable mass, blurred or decreased vision, pain, and chemosis [513]. These have been systematized in the literature into four generalized syndromes: infiltrative, mass, inflammatory, and functional [4]. The infiltrative and inflammatory syndromes are the initial manifestation in nearly 54% of cases [14]. Diplopia and ptosis as a presenting symptom, as reported in this case, are an infrequent event: these are present in only 9% of such patients [13]. Another notable aspect of our case is the fact that ophthalmic symptoms were the presenting manifestation of a non-diagnosed metastatic breast cancer. Typically, orbital metastases develop 20 to 40 months after primary tumor diagnosis and are generally a feature of widespread disease, as shown by further staging procedures in our patient [61011]. Indeed, the majority of orbital metastases of breast cancer occur in patients with a history of breast cancer [8] and are rarely the first sign.
Breast cancer is currently considered a compilation of intrinsic subtypes, each characterized by unique clinicopathol-ogic features, with unique patterns of metastatic spread and a distinct prognosis. Another relevant aspect in this case is the presence of a diffuse metastasis in the presence of a molecular subtype luminal A breast cancer, which typically demonstrates a good prognosis [15].
CT and MRI are the preferred imaging diagnostic methods, which detect more than 95% of orbital tumors [2]. However, careful anamnesis and physical examination are of utmost importance. In this case, breast examination failed to detect the cancer, and mammography identified an architectural distortion. Notably, mammography in the setting of an invasive lobular carcinoma is challenging, due to the infiltrative growth pattern of the neoplasm, resulting in less characteristic mammographic patterns and false negative rates between 8% and 19%. In this patient, previous cancer screening mammography (1 year prior) was negative.
As orbital involvement is a manifestation of disseminated disease, treatment is generally palliative. No data currently support the superiority of any particular chemotherapy regimen, and surgical intervention to the orbit merely serves a diagnostic purpose [5]. Radiotherapy is reserved for symptomatic control. Regardless of multimodal treatment applied in our case, disease progression occurred; the patient died 38 months after diagnosis. This is in agreement with existing literature: the overall prognosis of patients with orbital metastases is poor, with a mean survival of 18 to 24 months [5611].
Here, we have reported a case of atypical presentation of breast cancer, noting the diagnostic importance of the presence of a metastatic orbital tumor, especially in middle-aged and elderly women. Ophthalmic manifestations can play an important role in the detection of metastatic spread of an occult breast cancer.
Figures and Tables
Figure 1
Magnetic resonance imaging of the orbit and brain. (A) T1 coronal without fat suppression revealing an intraorbital infiltrative process with homogeneous signal equal to the upper rectus, lateral and upper oblique muscles (arrow). (B) T1 coronal exposing a left intraconal mass (arrow), after intravenous administration of gadolinium (homogeneous contrast uptake).

Figure 2
Histopathologic examination of the left orbital biopsy. (A) Connective tissue with diffuse and cordonal infiltrate of round and plasmacytoid neoplastic cells (H&E stain, ×200). (B) Epithelial nature confirmed by positivity for pankeratin mouse monoclonal cytokeratin antibody 116 (MNF116) (immunohistochemistry [IHC] for MNF116, ×100). (C) Neoplastic cells expressing E-cadherin (IHC for E-cadherin, ×200). (D) Strong and diffuse positivity for estrogen receptors (ER) (IHC for ER, ×200). (E) Neoplastic cells expressing GATA-binding protein 3 (GATA3) (IHC for GATA3, ×200).

References
1. Capone A Jr, Slamovits TL. Discrete metastasis of solid tumors to extraocular muscles. Arch Ophthalmol. 1990; 108:237–243.

2. Weiss R, Grisold W, Jellinger K, Mühlbauer J, Scheiner W, Vesely M. Metastasis of solid tumors in extraocular muscles. Acta Neuropathol. 1984; 65:168–171.

4. Goldberg RA, Rootman J. Clinical characteristics of metastatic orbital tumors. Ophthalmology. 1990; 97:620–624.

5. Eckardt AM, Rana M, Essig H, Gellrich NC. Orbital metastases as first sign of metastatic spread in breast cancer: case report and review of the literature. Head Neck Oncol. 2011; 3:37.

6. Park YM, Park JH, Lee SU, Lee JS. Metastatic breast cancer presenting as a subconjunctival mass. J Breast Cancer. 2014; 17:88–90.

7. Tamura M, Tada T, Tsuji H, Tamura M, Yoshimoto M, Takahashi K, et al. Clinical study on the metastasis to the eyes from breast cancer. Breast Cancer. 2004; 11:65–68.

8. Gupta S, Bhatt VR, Varma S. Unilateral orbital pain and eyelid swelling in a 46-year-old woman: orbital metastasis of occult invasive lobular carcinoma of breast masquerading orbital pseudotumour. BMJ Case Rep. 2011; 2011:pii: bcr1220103580.

9. Souayah N, Krivitskaya N, Lee HJ. Lateral rectus muscle metastasis as the initial manifestation of gastric cancer. J Neuroophthalmol. 2008; 28:240–241.

10. Ferry AP, Font RL. Carcinoma metastatic to the eye and orbit. I. A clinicopathologic study of 227 cases. Arch Ophthalmol. 1974; 92:276–286.
11. Shah RK, Lamichhane S. Ocular metastasis from breast carcinoma simulating anterior scleritis: a case report. J Med Case Rep. 2017; 11:249.

12. Leung V, Wei M, Roberts TV. Metastasis to the extraocular muscles: a case report, literature review and pooled data analysis. Clin Exp Ophthalmol. 2018; 46:687–694.

13. Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions. The 2002 Montgomery Lecture, part 1. Ophthalmology. 2004; 111:997–1008.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download