Abstract
Objective
To determine whether complications related to surgery increase with increasing number of cesarean sections (CSs) in upper segment placenta. To compare the complications in urgent and elective high order (4-6) repeat CSs.
Methods
A retrospective analysis of 519 women who underwent repeat CS was performed from January to December 2012. Women were divided into 3 groups: group 1 with previous 3 CS (n=325), group 2 with previous 4 CS (n=139), and group 3 with previous ≥5 CS (n=55).
Results
Statistically significant differences (P < 0.001) were observed among 3 groups, regarding mean gravidity, type of CS, midline incision and bilateral tubal ligation performed. The risks of severe intra-peritoneal adhesions, thin out lower uterine segment and bladder injury were significantly increased (P < 0.001) with increasing number of CS deliveries. Only one cesarean hysterectomy was done in group 1 due to post partum hemorrhage. No significant differences were found in blood loss, duration of surgery, post operative hospital stay as well as birth weight and Apgar scores of newborns. The elective and emergency CS groups of high order repeat CS had no remarkable differences in operative, post operative complications and fetal outcome.
Conclusion
Women with repeat CS are at increased risk of having multiple intra-operative surgical complications which increase with each subsequent CS. Pregnant women must be informed of the related risks which may affect counselling regarding possible tubal ligation.Women with repeat CS are at increased risk of having multiple intra-operative surgical complications which increase with each subsequent CS. Pregnant women must be informed of the related risks which may affect counselling regarding possible tubal ligation.
Globally, cesarean births have increased dramatically, over the past two decade. It has led to increase rate of repeated cesarean section (CS) also, and debatable its risks and benefits. Although CS is now safe in terms of sophistication in anesthesia and surgery [1]. One of the main indications for cesarean delivery is repeat CS. According to one of the largest studies, serious maternal morbidity increases with increasing number of cesarean deliveries specifically from the triad placenta previa, placenta accreta and cesarean hysterectomy [2,3,4]. However several studies found no association between multiple repeat cesarean section (MRCS) and maternal complications [1,5]. Until now, none has recommended a definite upper limit for the number of CS in a woman [2]. It is also reported that complication rate is higher in emergency CS than in elective ones [4,6]. In countries like Saudi Arabia, where large families are encouraged by social and cultural factors, any attempt to limit the CS number is likely to be rejected. Recent studies indicate that abnormal placentation (placenta previa and placenta accreta) is associated with an increase time of surgery in women undergoing their 4th CS. But there has been little increase in major operative complications or adverse perinatal outcomes [4,5]. There is widely held sentiment among clinicians that the first repeat CS seldom presents a surgical problem, but by the time, a woman undergoes a 4th CS, operative complications are common including difficult dissection, major bleeding and bowel or bladder injury. So, this study was planned to determine whether intra-operative complications increase with increasing number of CS, in normally situated placenta. Moreover, to evaluate whether emergency high order repeat CS in comparison to elective ones carry greater risks regarding feto-maternal complications.
Medical records of all women who underwent a CS because of previous 3 or more CS from January to December 2012 at Abha General Maternity Hospital, Abha Kingdom of Saudi Arabia. Were included and reviewed. The inclusion criterion was repeated CS performed ≥28 weeks gestation. The cases of MRCS with placenta previa and placenta accrete diagnosed antenataly by magnetic resonance imaging, were excluded from the study because these cases are routinely referred to higher centres where higher level of intensive care unit (ICU) and interventional radiological facilities (to conserve uterus) are available. Total 650 cases of MRCS were done during the study period. Excluded cases were 123 due to abnormal placentation (previa and accereta) and eight cases because of <28 weeks gestation. The remaining 519 women were divided into three groups: group 1 with previous 3 CS (n=325), group 2 with previous 4 CS (n=139), and group=3 with previous ≥5 CS (n=55). Patients who had ≥4 previous CS were categories as high order repeat CS. High order (4-6) repeat CS was divided into elective and emergency groups.
The case records of women were analyzed for the demographics and clinical features including age, parity, gestational age, number of previous CS, type of CS, type of abdominal incision and whether bilateral tubal ligation (BTL) was performed/not at time of surgery. Operative and post-operative course including, time of operation, estimated blood loss, severity of adhesion, scar dehiscence, thinning of lower segment of uterus, bladder and bowel injury, blood transfusion, ICU admission, fall in hemoglobin, deep venous thrombosis, wound infection, and length of hospital stay were recorded. Fetal characteristics including birth weight, Apgar scores, and fetal outcome were recorded. The severity of the pelvic adhesions was graded according to American Fertility Society Classification of adnexal adhesions. Filmy/avascular adhesions involving 1% to 25% of the total area are classed as mild, dense/vascular involving 26% to 50% of pelvic area is moderate and greater than 50% of the area are severe. The departmental policy is to perform elective CS on patients who have had ≥3 previous CS between 37 and 38 weeks of gestation by specialist or consultant. Emergency CS was defined as an operative delivery, carried out for unplanned reasons. In general, pfannenstiel incision is used to open the abdominal cavity and a transverse incision is used in the lower segment of the uterus. Longitudinal abdominal incision is used if the patient has already had a longitudinal incision or if there is a history of severe pelvic adhesions. Uterine scar dehiscence was defined as, a window in the lower segment of the uterus with intact peritoneum and membrane. The operating time was estimated in minutes from induction of anesthesia to completion of skin suturing. In our department, bladder is considered to be injured if methyline blue dye test is positive during surgery.
Data entry and analysis were performed with SPSS ver. 17 (SPSS Inc., Chicago, IL, USA). Demographic data were summarized using descriptive statistics (mean, standard deviation, range, and percentage). Clinical data were compared by using unpaired t test for normally distributed continuous variables, χ2 and Fisher's exact test for categorical variables where appropriate. Variables of group 1 were compared with those of group 2 and 3 and variables of group 2 were compared with those of group 3. Statistical significance was considered when P<0.05. The study was approved by the respective institutional research and ethics committee.
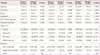
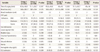
The demographics and clinical features of all women are given in Table 1. In group 3, out of 55 women, 52 (94.5%) had previous 5 CS and 3 (5.5%) had history of previous 6 CS. Regarding fetal outcome, no significant differences were observed among three groups in gestational age, birth weight and 5 minutes Apgar scores. In group 1, three cases of MRCS presented with intra uterine fetal death. In antenatal complications, pregnancy induced hypertension was observed in 14 (4.3%) women of group 1 and 4 (2.8%) cases of group 2. Diabetes mellitus was found in 7 (2.1%), 8 (5.7%), and 1 (1.8%) women of group 1, 2, and 3, respectively. There was placental abruption in 4 cases of group 1 and 2 women of group 3. Intra and postoperative course of women is presented in Table 2. No maternal death was observed. Only one cesarean hysterectomy was performed in group 1 because of uterine atony and heavy bleeding. Although severity of adhesions increased with successive number of CS (Table 2) but no remarkable difference was observed in, time of surgery and blood loss in all three groups of women. During surgery, drain was inserted in 7 (2.1%) of group 1, 3 (2.1%) of group 2 and 4 (7.2%) of group 3 women. Pulmonary embolism was detected postoperatively in one woman in group 1 that was managed successfully. Bilateral tubal ligation was performed in 32 (9.8%), 68 (48.9%), and 36 (65.4%) patients of group 1, 2, and 3 respectively. It was significantly increased successively in all groups (P<0.05).
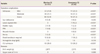
The BTL procedure was not possible in some women who had given its consent, because of severe adhesions in 3 (0.92%) of group 1, 3 (2.1%) of group 2 and 2 (3.6%) of group 3. Only 3 (5.4%) cases of group 3 required Foley's catheter to be retained for 10 days postoperatively, in suspicion of bladder injury (methyline blue test was negative). All six cases of bladder injury were managed by repair, done by the urologist during surgery. Two cases of postoperative urinary tract infection were found in group 3. One patient of group 2 developed frank hematuria postoperatively. No case of bowel injury was found. Women in group 3 had a significantly higher incidence (P<0.001) of scar dehiscence, thinning of lower segment of uterus and bladder injury. Difference in scar dehiscence was statistically significant (P=0.001) between group 2 (3.6%) and group 3 (16.3%). Similarly bladder injury was also statistically significant (P=0.001) between group 2 (0.7%) and group 3 (5.5%). The finding of thinning of lower segment was statistically significant (P=0.001) between group 1 (3.7%) and group 3 (9.1%). Table 3 is presenting comparison between elective and emergency high order MRCS for intra and postoperative complications. Regarding surgery time, blood loss, hemoglobin drop and hospital stay, no remarkable difference was observed in these two groups. In the emergency CS group, thinning of lower segment of uterus and postoperative wound infection had a statistically significant higher incidence (P<0.001). Intra-operative blood transfusion requirement and scar dehiscence was high in women who underwent emergency CS although it was statistically insignificant. Severe adhesions were (52.9% vs. 37.2%), postpartum hemorrhage (4.6% vs. 2.3%) and postoperative hernia was (3.3% vs. 0%) in elective versus emergency CS group. These all differences between both groups were statistically significantly (P=0.001). Neonatal outcome was not significantly different in these two groups.
A worldwide increase in CS rate has resulted in a decrease in the proportion of women achieving spontaneous vaginal delivery [7]. A considerable obstetric hazard of MRCS is previous uterine scar rupture with consequent increase in both maternal and fetal morbidity and mortality. In the present study, incidence of scar dehiscence was found successively increased with increasing number of CS. Although this difference was statistically significant only between group 2 (CS=4) and group 3 (CS≥5) (Table 2). This finding is in agreement with others [4,8] but out of line with some researchers who reported no increase in incidence of uterine scar rupture with increasing number of CS [1,2,9]. Our results are expected and clear but opponents explained their own results unexpected due to unclear reasons [1,9]. All cases with the finding of thinning of lower segment of uterus were also from emergency CS group (Table 3). This establishes the importance of proper counselling and planning of elective CS before starting labour. Different studies showed variable rates of adhesion formation and their consequences. We found that severe adhesions formation increased significantly with successive number of CS, (27%, 49%, and 53% in group 1, 2, and 3, respectively) (Table 2). It is in line with others [1,2,9,10]. This is not unexpected because repeated surgeries are associated with subsequent adhesion formation [5,11]. Furthermore, it has been described that presence of severe adhesions can adversely affect the course of subsequent abdominal surgery by increasing the time of operation, the need for blood transfusion and the injury to the surrounding structures including bowel and ureters. In the current study, no significant difference was observed in these parameters, in relation to number of CS. Reason may be that MRCS were done by the consultant or experienced specialists only. High attachment of the bladder on abdominal wall has been described frequently in the women with high number of CS and should be taken into consideration while opening the peritoneum. Alternatively, a midline incision should be considered in cases of severe adhesions. This study showed that the rate of midline incision to open the abdominal cavity, significantly increased with successive number of CS (4%, 40%, and 60% in group 1, 2, and 3, respectively) (Table 1). No bowel injury was observed in this study. Others have also reported a relatively low incidence of bowel injury during repeat CS as utero-intestinal adhesions are less common [9,12]. Due to pelvic adhesions, incidence of bladder injury was found to increase with successive number of CS (0.6%, 0.7%, and 5.5% in women of group 1, 2, and 3, respectively) (Table 2). In general, careful and meticulous entry into peritoneal cavity is the key in reducing injury to the surrounding organs. No significant correlation was observed regarding minor morbidities such as urinary tract infection and chest infection in various groups. In keeping with others [4,8,13,14] the incidence of post operative hernia and wound infection was found significantly increased with the number of CS (Table 2). In accordance with other reports [1,14] no significant difference was observed in the neonatal Apgar score, neonatal intensive care unit admission and perinatal mortality rate, in high versus low order repeat CS. In contrast Seidman et al. [15] described significant association between low Apgar scores and high number of previous CS. We found significantly lower rate of emergency CS (22%) than elective ones (78%) in women of high order (4-6) MRCS. This achievement was probably due to close antenatal follow up and early scheduling for CS in women with high order MRCS. Because of awareness of risks associated with MRCS, about one half of group 2 and 2/3rd of group 3 women opted for tubal ligation despite the fact that BTL is generally not accepted by Saudi women [1]. Unexpectedly, the incidence of severe adhesions, postpartum hemorrhage and postoperative hernia were observed significantly high in women of elective CS group (Table 3). Cause of increased incidence of severe adhesions may be early scheduling of CS due to past difficult operative history but high incidence of postpartum hemorrhage and hernia were unexplainable in elective CS group. No significant differences were observed regarding morbidity between emergency and elective MRCS groups. This may be due to the reason that women who had emergency CS reached hospital soon, after starting labour pains or prelabour rupture of membranes. On the basis of these results, it cannot be concluded that there is no difference in morbidity of emergency and elective MRCS due to small sample size. However larger scale studies are recommended to verify these findings.
In conclusion, the incidence of scar dehiscence, adhesion formation and bladder injury increases with increasing number of CS. However, there is no remarkable difference in serious morbidity associated with emergency and elective CS cases. Although not life threatening, multiple repeat CS is associated with risks, so awareness should be extended to the women.
Figures and Tables
References
1. Rashid M, Rashid RS. Higher order repeat caesarean sections: how safe are five or more? BJOG. 2004; 111:1090–1094.
2. Juntunen K, Makarainen L, Kirkinen P. Outcome after a high number (4-10) of repeated caesarean sections. BJOG. 2004; 111:561–563.
3. Gilliam M, Rosenberg D, Davis F. The likelihood of placenta previa with greater number of cesarean deliveries and higher parity. Obstet Gynecol. 2002; 99:976–980.
4. Kirkinen P. Multiple caesarean sections: outcomes and complications. Br J Obstet Gynaecol. 1988; 95:778–782.
5. Lynch CM, Kearney R, Turner MJ. Maternal morbidity after elective repeat caesarean section after two or more previous procedures. Eur J Obstet Gynecol Reprod Biol. 2003; 106:10–13.
6. Miller DA, Chollet JA, Goodwin TM. Clinical risk factors for placenta previa-placenta accreta. Am J Obstet Gynecol. 1997; 177:210–214.
7. Robson M. Can the high caesarean section rates be reduced?. In : Bonnar J, Dunlop W, editors. Recent advances in obstetrics and gynaecology. Vol. 22. London: Royal Society of Medicine;2003. p. 71–83.
8. Qublan HS, Tahat Y. Multiple cesarean section. The impact on maternal and fetal outcome. Saudi Med J. 2006; 27:210–214.
9. Sobande A, Eskandar M. Multiple repeat caesarean sections: complications and outcomes. J Obstet Gynaecol Can. 2006; 28:193–197.
10. Roset E, Boulvain M, Irion O. Nonclosure of the peritoneum during caesarean section: long-term follow-up of a randomised controlled trial. Eur J Obstet Gynecol Reprod Biol. 2003; 108:40–44.
11. Tulandi T, Agdi M, Zarei A, Miner L, Sikirica V. Adhesion development and morbidity after repeat cesarean delivery. Am J Obstet Gynecol. 2009; 201:56.e1–56.e6.
12. Piver MS, Johnston RA Sr. The safety of multiple cesarean sections. Obstet Gynecol. 1969; 34:690–693.
13. Nisenblat V, Barak S, Griness OB, Degani S, Ohel G, Gonen R. Maternal complications associated with multiple cesarean deliveries. Obstet Gynecol. 2006; 108:21–26.
14. Uygur D, Gun O, Kelekci S, Ozturk A, Ugur M, Mungan T. Multiple repeat caesarean section: is it safe? Eur J Obstet Gynecol Reprod Biol. 2005; 119:171–175.
15. Seidman DS, Paz I, Nadu A, Dollberg S, Stevenson DK, Gale R, et al. Are multiple cesarean sections safe? Eur J Obstet Gynecol Reprod Biol. 1994; 57:7–12.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download