This article has been corrected. See "Erratum: Author's Name Correction" in Volume 55 on page 692.
This article has been corrected. See "Erratum: Relationship among bacterial vaginosis, local inflammatory response and presence of cervical intraepithelial neoplasia in women with and without human papilloma virus infection" in Volume 55 on page 795.
Abstract
Objective
An assessment of influence of human papilloma virus (HPV) infection on the presence of dysplasia and relationship among the local immune system, HPV infection and bacterial vaginosis (BV).
Methods
The study group (n = 143) was divided into: experimental arm: positive HPV-DNA sequence with polymerase chain reaction method on the cervix tissue specimen (HPV group, n = 82), control arm: negative HPV-DNA sequence (nHPV group, n = 61). Secondarily, the study group was divided into: subgroup with malignant lesions (ML group, n = 95) and subgroup with benign lesions (BL group; n = 48). Each patient was evaluated for: bacterial morphotype (Nugent score), cervical inflammation, HPV cervical infection classified by virus subtype, histopathological examinations of the cervix biopsy.
Results
In HPV group there was higher prevalence of women who: had their first sexual contact between 16 and 22 years (P < 0.001), had more than 3 previous or actual sexual partners (P < 0.001, P < 0.05; respectively), were unmarried (P < 0.01). We found: significantly higher prevalence of polymorphonuclear cervicitis and Candida albicans (C. albicans)-hyphae predomination in HPV group, but Gardnerella vaginalis in nHPV group, predomination of benign lesions in nHPV group, prevalence of Trichomonas vaginalis, as well as normal vaginal flora in BL subgroup, but C. albicans -sporae in ML subgroup. The most frequent infections in HPV group were those with HPV type 16 and 53.
Bacterial vaginosis (BV) is common, treatable condition, where the normal Döderlein-dominated vaginal flora is replaced by other, predominantly anaerobic flora. Previous studies which have examined the relationship between BV and cervical intraepithelial neoplasia (CIN) gave conflicting conclusions with different results which ranged from a strong association [1] to no association at all [2]. In the earlier eighties Pavić [3], discussing possible analogies between gastric and cervical cancer, concluded that in both, an elevation of pH could encourage proliferation of bacteria, and those situation could be preceded by epithelial metaplasia and dysplasia. According to him, the nitrosamines, which were form anaerobes could act with a production of neoplastic change, or as a synergic agent with some viral agent. Some more recent studies also investigate the possible biochemical mechanism by which microorganisms might influence expression of oncogenic human papilloma virus (HPV). McNicol et al. [4] found that presence of Lactobacilus species, like (Döderlein bacillus) and E6 oncogene were associated with low-grade CIN or normal histology.
It is generally considered that the mutations observed among the cancer genomes are a consequence of the survival selection caused by the surrounding microenvironment. Loss of class-I human leukocyte antigen (HLA) alleles under the selective pressure of anti-tumor cytotoxic T lymphocyte responses has been demonstrated in cell lines obtained from metastatic melanomas [5]. Alternated HLA phenotypes implicate the possibility of tumor immune escape from T-cell recognition in human cancer models. In human cervical cancer, local immunity against this HPV-associated neoplasia has been signified. However, this possibility of tumor immune escape from immunocytes recognition, and T-cells residing within the tumor milieu remain to be clarified. Sheu et al. [6] demonstrated that human cancer cells may alter the functional composition of anti-tumor effector-cells, including CD8 cytotoxic T-cells in the human cancer microenvironment. The immunoregulatory effects of cancer HLA genetic alterations in associated HPV in the human cancer milieu remains to be stratified. Tsukui et al. [7] reported that helper T-lymphocyte response, particularly interleukin (IL)-2 production to HPV antigens was greater among women with normal cytology than in women with different degrees of cervical neoplasia. de Gruijil et al. [8] reported that T cell proliferative responses to HPV-16 E7 peptides correlated with persistence of HPV infection, but antigen specific IL-2 production was associated with both virus clearance, as well as progression of cervical lesions. A better understanding of tumor responses is needed to design future strategies for effective immune-prevention of HPV-associated malignancies. A common clinical management includes excisional treatment. However, a significant number of patients experience recurrence, but a clear understanding do not exists at the presence regarding the role of the immune system and its relationship with this disease recurrence. Our intention was to establish a prospective, controlled study with due regard to the presence of HPV whether there is a relationship between BV and CIN as this would mean a major shift in cervical screening practice, and giving some contribution to future understanding of possible relationship among the local immune system, present HPV infection and CIN.
For experimental group: presence of cervical HPV infection; for control group: absence of this infection.
The Department for Urogynecology and Pelvic Floor Disorders in the Clinic of Gynecology and Obstetrics, Medical Faculty in Skopje in the period from the 1st of January 2009 to the 1st of January 2010, according to the CONSORT statement [9].
The whole study group (n = 143) was divided into two subgroups: 1) The experimental arm: positive finding of the HPV DNA sequence with PCR method on the tissue specimen of the cervix (HPV group) (n = 82); 2) The control arm: negative finding of the HPV DNA sequence with polymerase chain reaction (PCR) method on the tissue specimen of the cervix (nHPV group) (n = 61). Secondarily, the whole study group was divided into another two subgroup according to the histology: 1) Subgroup with malignant lesions (ML) (n = 95); and 2) Subgroup with benign lesions (BL) (n = 48). The study was approved by the Local Research Ethics Committee of the Association of Gynecologists and Obstetricians of Macedonia.
Every outpatient admitted at our Department for Urogynecology for routine control in abovementioned period, assessed for eligibility for this study (n = 168). Nine patients were excluded because they refused to participate. Additional 16 patients dropped out because they had invalid smears for cervical inflammation evaluation, i.e. no identifiable for cervical mucus smears. So, 143 patients were randomised and they completed the study. Eighty-two of them were positive of HPV infection and were included in experimental HPV group, but other 61 patients were negative of this infection and were included in control nHPV group. All subjects were given an explanation of the study and written informed consent was obtained. This was a controlled trial with no allowance for patient preference.
The purpose of the study was an assessment of: 1) The influence of HPV infection on the presence of CIN; 2) The possible relationship among the local immune response, HPV infection and BV. The hypotheses were: 1) In the presence of HPV cervical infection there is a mononuclear predominance in the cervical smear as a sign of local immune response on the viral infection; 2) In presence of HPV cervical infection there is a predominance of the Candida albicans (C. albicans) infection with its active - hyphae as a sign of diminished local tissue immunity; 3) In presence of HPV cervical infection there is a predominance of CIN lesions.
Age, age of the first sexual contact, parity, number of previous partners, number of actual sexual partners, habits, social status, marriage status, profession.
Each PAP slide was assigned a score of 0 to 10 using a standardized scoring system (Nugent score) based on the relative proportion of bacterial morphotypes, which has been previous shown to be reliable test for BV [10]. The composite score, based on the number of each bacterial morphotype, was assigned: with: 1) Score (0), corresponding to vaginal flora dominated by Lactobacillus ; 2) Score (10), corresponding to vaginal flora dominated by Gardnerella/Bacteroides. The score of 0-3 was judged as normal (Lactobacillus - dominated) flora, a score of 4-6 was judged as intermediate or reduced Lactobacilli, and score of 7-10 was judged as BV-dominated.
Evaluation of the cervical inflammation was assessed by counting the number of polymorphonuclears (PMNLs) or mononuclears (MNLs), observed in microscope fields on PAP slides from each study subject. Enrollment smears were evaluated at ×40 initially to identify cervical mucus. Smears having no identifiable cervical mucus were considered invalid for evaluation because of uncertainties related to sampling adequacy. Valid slides were observed at ×100 to identify PMNLs, identifiable by their multi-lobed nuclei, or MNLs, identifiable by their single-lobed nuclei. The numbers of PMNLs or MNLs were counted in five nonadjacent fields not contaminated by squamous epithelial cells, and were averaged and scored as no inflammation (0-5 leukocytes/field); and PMNLs - cervicitiis or MNLs - cervicitis (>5 leukocytes/field). HPV infection was evaluated in each study subject with PCR method on the tissue specimen of the cervix and classified as positive or negative of the HPV DNA sequence and classified according to subtype of the HPV.
The tissue specimens of the cervical biopsy were fixed in 10% neutral buffered formalin for 24 to 48 hours and routinely processed in paraffin wax. They were examined by light microscopy by the same pathologist, who was not informed of the patient group. They were graded using the standard morphological criteria.
The Student's paired test was used to compare some demographic data, such as age and parity. The Kolmogarov-Smirnoff test was used to compare the differences between the particular types of HPV into HPV group regarding: inflammatory infiltration, type of vaginal flora and histological feature of the cervical specimens. The Mantel-Haenzel's χ2 test was used to compare demographic data, as well as to estimate differences between the study groups regarding: inflammatory infiltration, type of the vaginal flora and histological feature of the cervical specimens, according to the formula.
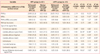
On Table 1 we represent the demographic data, we found that in HPV group there was a higher prevalence of women who: had their first sexual contact between 16 and 22 years (P < 0.001); 2) had more than three previous sexual partners (P < 0.001) and more than three actual sexual partners (P < 0.05); and 3) in HPV group there were more unmarried women than in nHPV group (P < 0.01). Regarding the profession, in HPV group there were more pupils/students, but in nHPV group there were more housewives (Table 1).
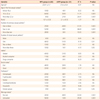
We found: 1) Significant predomination of the PMNLs inflammatory infiltration in the cervical smear and a predomination of C. albicans-sporal form in nHPV group; 2) A predominance of C. albicans-hyphae form in HPV group; 3) Gardnerella vaginalis in nHPV group, as well as predominance of benign lesions in the same group (Table 2).
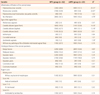
On Table 3 we represent the differences among the subgroups regarding: inflammatory infiltration of the cervical smear, type of vaginal flora and histological feature of the cervical specimens. We did not noticed differences between the subgroups with and without malignant pathology, but significant predominance of the MNLs into two subgroups with HPV infection vs. subgroups without it. Regarding the type of vaginal flora, we found: 1) Significantly higher predominance of Trichomonas vaginalis into the subgroups with benign cervical pathology; 2) C. albicans-hyphae form dominated in HPV group, but we did not found any significance between the subgroups with and without malignant pathology; It had to be point out that in subgroup nHPV(m) C. albicans was present in all patients, particularly with its sporal form, but on the contrary, in very small part of the nHPV(b) subgroup (15.4%); normal vaginal flora predominated into nHPV(b), but on the other hand also into the HPV(m), that was very surprising. Gardnerella vaginalis dominated into the subgroup nHPV(m) (Table 3).
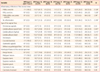
We found: significant prevalence of trichomonas vaginalis and C. albicans, as well as normal vaginal flora in BL, but sporal form of C. albicans in ML (Table 4).
We found that: PMNLs-cervicitis predominated in HPV type 16 and 58 infection; and MNLs-cervicitis in HPV type 18, 31, 33, and 53 infection. Regarding the vaginal flora, we found significant prevalence of: C. albicans-sporal form in HPV type 16 and 58 infection, but C. albicans-hyphae in HPV type 18; and normal vaginal flora in HPV 33 infection. Regarding the histological feature of the cervical specimen, we found the highest prevalence of malignant lesions in HPV type 18, mild dysplasia predominated in HPV type 53, but Carcinoma in situ in HPV type 18. The most frequent infections were those with HPV: type 16, 53 (Table 5).
According to Boyle et al. [11] women with BV were not found to have CIN more frequently than women with normal vaginal flora. Their study did not demonstrate a relationship between BV and CIN irrespective of the presence of high-risk HPV in cervical cells. To test whether changes in vaginal bacterial flora or the degree of cervical inflammation are associated with women having a HPV infection or with women infected with oncogenic HPV having high-grade cervical lesions, Castle et al. [12] found a marginally significant positive trend of increasing cervical inflammation associated with high-grade lesions in oncogenic HPV-infected women. We found significant predominance of C. albicans-sporal form in vaginal flora in nHPV group, and a predominance of C. albicans-hyphae form in HPV group. Our opinion is that this situation may be due to a declining of the local immunity by viral infection, and this situation could result in flourishment of some comensals, such as C. albicans, which is predominantly present in its active-hyphae form. Perhaps, the concomitant presence of HPV infection and C. albicans infection might be the two manifestations of the same situation, the diminished local and systemic immunity status of the patient. According to Laurence [13] male-to female penile-vaginal transmission of at least two viruses, HIV-1 and HPV is blocked by local mucosal responses, immunologic or otherwise, which require repetitive, uninterrupted exposure to pathogen. Exploration of the mechanisms underlying such ostensibly protective responses may facilitate development of sexual transmitted diseases (STD)-vaccines. He hypothesizes that this phenomenon is but one instance of an acquired mucosal-based response to certain viral STDs. Blockade of local infection receptors could result from competition for receptors on vaginal mucosa between infectious virus and defective virions. Another hypothesis proposes that mucin-degrading enzymes are increased in women with BV. These enzymes, like sialidases, play a role in degradation of the gel layer coating the cervical epithelium, causing micro-abrasions or alterations of epithelial cells and promoting virulence through destroying the protective mucosa barrier [14,15]. Mucosal immune system activation represents a critical response against microorganisms. PMNLs recruitment and activation is considered the main innate immune response against microbal and viral infections of the vaginal mucosa [16]. Women with BV and HPV infection have vaginal smears on which the neutrophils are typically relatively absent, as a sign of potentially altered immune response by enzymes produced by anaerobic vaginal bacteria [17]. In our study, in HPV group we found: no inflammation in one third of the group and a significant predominance of the MNLs - vs. PMNls - cervicitis, as a sign of the altered local immune response. The question remains whether BV and cervical HPV infection are simply related because there is a biologic interaction between them, or they are the expression of the promiscuity of women and their partners. The study of Mao et al. [18] confirmed the positive correlation between BV and HPV infection and also reported that BV was found to occur simultaneously with or after HPV infection, rather than ante-dating acquisition of HPV. These results suggest that cervical HPV infection may favor changes in the vaginal milieu that enhance development of BV. On average the risk for HPV infection rises nearly 10-fold for each new partner per month of observation [14]. According to Kjaer et al. [19] age is the most important risk factor for cervicovaginal infection. However, the found a declining incidence of HPV acquisition with increasing length and number of unprotected sexual exposures. In our study we found that in HPV group there was a higher prevalence of women who: had their first sexual contact between 16 and 22 years (P < 0.001); 2) had more than three previous sexual partners (P < 0.001) and more than three actual sexual partners (P < 0.05); and 3) were unmarried (P < 0.01) vs. nHPV group. Although classic signs of inflammation do not accompany HPV infection, clearance of HPV from genital tract is characterized by an active Th1-type cellular immune response. Lesion-derived T cells are primarily of an activated memory phenotype, and HPV antigens are present in locally differentiation keratinocytes, which could present these antigens to T cells [16]. Disorders of humoral immunity do not correlate with increased susceptibility to HPV infection or disease [17]. Inflammation is a relatively nonspecific physiological response to tissue injury caused by exogenous factors such, as microbial or viral agents. Hallmarks of the inflammatory response include migration of natural killer cells and phagocytes (e.g., neutrophyls and macrophages). The association of inflammation with many cancers suggests that inflammation may be a universal risk factor for carcinogenesis. In our study we found a significant predominance of the MNLs into two subgroups with HPV infection vs. subgroups without it. Our opinion is that our findings may be due to the immune response of the viral infection, which is grounded on natural killer cells and phagocytes, that is to say monocytes. Nunn et al. [20] found that females of the polyandrous macaque species had significantly higher levels of peripheral immune cells, lymphocytes and monocytes in ths absence of changes in inflamatory cells, such as neutrophils vs. monogamous gibbon apes. Castle et al. [12] collect paired plasma and cervical secretion in 70 women with low-grade cytologic abnormalities of the cervix to investigate the relationship between cervical concentrations of IL-10 and IL-12 as the immune markers with their association with Th1 and Th2 responses, respectively, and their plasma levels. They found lack of correlation and high concentrations in cervical secretions, which suggested a high local cytokine production. In our study we found a significant prevalence of C. albicans-sporal form in the subgroup with malignant cervical lesions (P < 0.01) vs. subgroup with benign pathology of cervix. These findings can be due to a secundary activation of the local immunity in appareance of cervical neoplasia and a changing of the comensals, such as C. albicans into its inactive sporal form. We did not find any significant differences between these two subgroups regarding cervical infiltration with PMNLs and MNLs.
In women with HPV infection local inflammatory response is predominantly expressed by mononuclear infiltration. In this population could be present a declining of local immunity, which could result in flourishing of the commensals, such as C. albicans, which is predominantly present in its active hyphae-form. With starting of cervical neoplastic process it could be possible a secundary activation of local immunity, which has its expression in changing of C. albicans into its inactive, sporal form.
Figures and Tables
Table 3
Differences among the subgroups
Values are presented as number (%).
HPV, human papilloma virus; nHPV, negative HPV; χ2 (1), differences between column 1 and 2; χ2 (2), differences between column 3 and 4; χ2 (3), differences between column 1 and 3; χ2 (4), differences between column 2 and 4; PMNLs, polymorphonuclears; MNLs, mononuclears.
Mantel-Haenzel's χ2 test with df of 1: aP<0.001, bP<0.01, cP<0.05.
Table 4
Differences between: Malignant lesions subgroup (ML) and benign lesions subgroup (BL) regarding: inflammatory infiltration of the cervical smear, type of vaginal flora and histological feature of the cervical specimens

References
1. Platz-Christensen JJ, Sundström E, Larsson PG. Bacterial vaginosis and cervical intraepithelial neoplasia. Acta Obstet Gynecol Scand. 1994. 73:586–588.
2. Peters N, Van Leeuwen AM, Pieters WJ, Hollema H, Quint WG, Burger MP. Bacterial vaginosis is not important in the etiology of cervical neoplasia: a survey on women with dyskaryotic smears. Sex Transm Dis. 1995. 22:296–302.
3. Pavić N. Is there a local production of nitrosamines by the vaginal microflora in anaerobic vaginosis/trichomoniasis? Med Hypotheses. 1984. 15:433–436.
4. McNicol PJ, Paraskevas M, Guijon FB. The effect of vaginal microbes on in vivo and in vitro expression of human papillomavirus 16 E6-E7 genes. Cancer Detect Prev. 1999. 23:13–21.
5. Lehmann F, Marchand M, Hainaut P, Pouillart P, Sastre X, Ikeda H, et al. Differences in the antigens recognized by cytolytic T cells on two successive metastases of a melanoma patient are consistent with immune selection. Eur J Immunol. 1995. 25:340–347.
6. Sheu BC, Hsu SM, Ho HN, Lin RH, Torng PL, Huang SC. Reversed CD4/CD8 ratios of tumor-infiltrating lymphocytes are correlated with the progression of human cervical carcinoma. Cancer. 1999. 86:1537–1543.
7. Tsukui T, Hildesheim A, Schiffman MH, Lucci J 3rd, Contois D, Lawler P, et al. Interleukin 2 production in vitro by peripheral lymphocytes in response to human papillomavirus-derived peptides: correlation with cervical pathology. Cancer Res. 1996. 56:3967–3974.
8. de Gruijl TD, Bontkes HJ, Stukart MJ, Walboomers JM, Remmink AJ, Verheijen RH, et al. T cell proliferative responses against human papillomavirus type 16 E7 oncoprotein are most prominent in cervical intraepithelial neoplasia patients with a persistent viral infection. J Gen Virol. 1996. 77:2183–2191.
9. Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet. 2001. 357:1191–1194.
10. Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol. 1991. 29:297–301.
11. Boyle DC, Barton SE, Uthayakumar S, Hay PE, Pollock JW, Steer PJ, et al. Is bacterial vaginosis associated with cervical intraepithelial neoplasia? Int J Gynecol Cancer. 2003. 13:159–163.
12. Castle PE, Hillier SL, Rabe LK, Hildesheim A, Herrero R, Bratti MC, et al. An association of cervical inflammation with high-grade cervical neoplasia in women infected with oncogenic human papillomavirus (HPV). Cancer Epidemiol Biomarkers Prev. 2001. 10:1021–1027.
13. Laurence J. Repetitive and consistent cervicovaginal exposure to certain viral pathogens appears to protect against their sexual acquisition in some women: potential mechanisms. J Reprod Immunol. 2003. 58:79–91.
14. Briselden AM, Moncla BJ, Stevens CE, Hillier SL. Sialidases (neuraminidases) in bacterial vaginosis and bacterial vaginosis-associated microflora. J Clin Microbiol. 1992. 30:663–666.
15. Gillet E, Meys JF, Verstraelen H, Bosire C, De Sutter P, Temmerman M, et al. Bacterial vaginosis is associated with uterine cervical human papillomavirus infection: a meta-analysis. BMC Infect Dis. 2011. 11:10.
16. Cauci S. Vaginal Immunity in Bacterial Vaginosis. Curr Infect Dis Rep. 2004. 6:450–456.
17. Figueiredo PG, Sarian LO, Tambascia JK, Simões JA, Rabelo-Santos SH, Discacciati MG, et al. Increased detection of clue cells in smears from cervical intraepithelial lesions with reduced expression of COX-2. Diagn Cytopathol. 2008. 36:705–709.
18. Mao C, Hughes JP, Kiviat N, Kuypers J, Lee SK, Adam DE, et al. Clinical findings among young women with genital human papillomavirus infection. Am J Obstet Gynecol. 2003. 188:677–684.
19. Kjaer SK, Svare EI, Worm AM, Walboomers JM, Meijer CJ, van den Brule AJ. Human papillomavirus infection in Danish female sex workers. Decreasing prevalence with age despite continuously high sexual activity. Sex Transm Dis. 2000. 27:438–445.
20. Nunn CL, Gittleman JL, Antonovics J. Promiscuity and the primate immune system. Science. 2000. 290:1168–1170.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download