Abstract
Peutz-Jeghers syndrome, which has autosomal dominant inheritance, shows pigmentation in lip and skin. It also has features of harmatomatous polyp over the gastrointestinal tract, while sometimes developing tumor in genital tract. Known tumors in female genital tract include cervical adenocarcinoma, sex cord tumor, etc. Adenomyomatous polyp in uterus is also one of the rare diseases, which seldom develop in the absence of hormone treatment such as Tamoxifen. Currently, there is one case of Peutz-Jeghers syndrome patient with endometrial adenomyomatous polyp. Authors found mole-like lesions on the transvaginal ultrasonogram in a typical Peutz-Jeghers syndrome patient without pregnancy history and previous chemotherapy. After confirming its diagnosis of adenomyomatous polyp on resectoscopic biopsy, we report our fihndings along with brief literature review.
Peutz-Jeghers syndrome (PJS) is known to have autosomal dominant inheritance and is related to the STK11 gene. The symptoms include dark-colored pigmentation from the lip and buccal mucosa to fingers and to the toes, along with harmatomatous polyp over the entire gastrointestinal tract. Moreover, in addition to gastrointestinal tract, it can cause tumor in breast, genital tract, lung, etc. Known tumors in female genital tract include cervical adenocarcinoma, ovarian sex cord tumor, granulosa cell tumor, etc. adenomyomatous polyp in uterus has stromal component consisting of smooth muscle cells and it occasionally develops among women who received hormonal therapy such as Tamoxifen. It has a feature of mole-like appearance of vesicle pattern on the transvaginal ultrasonogram.
A twenty-eight-year-old female visited our hospital with vaginal spotting for about a month. She did not experience pregnancy and had characteristic dark-colored pigmentation in skin and lip. She has a history of bowel resection seventeen and twelve years ago. She did not remember the reasons of bowel resection. As for Family history, the patient's mothor died from cervical cancer. She had no history of previous hormonal therapy, such as Tamoxifen. In a transvaginal ultrasonogram, mole-like lesion with a thickness of 3 cm was detected in endometrium, with normal β human choriogonadotropin level. There were no abnormalities on uterine cervix and both adnexaes. Diagnostic uterine curettage was performed, but enough specimen was not taken. There was no malignant cells. Following ultrasonogram assisted resectoscopic polypectomy was performed under general anesthesia after two weeks, where the endometrium was filled with Swiss cheese like lesion. During the follow-up observation period, she visited Division of Gastroenterology to receive endoscopic mucosal resection and colonoscopy. The duodenal polypectomy revealed harmatomatous polyp and hence the patient was diagnosed with PJS. According to the follow-up transvaginal ultrasonogram, the endometrium showed decreased thickness to 1.6 cm, while still being observed as mole-like lesion. Two months after performing primary resectosopy, the secondary resectoscopic polypectomy was performed under general anesthesia. The endometrium was still filled with Swiss cheese like lesion and the diagnosis of adenomyomatous endometrial polyp was confirmed.
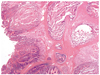
The submitted endometrium from the primary curettage and the secondary resectoscopic biopsy showed the similar histologic finding each other. The endometrium revealed several pieces of irregular sized polyps measuring 1.5×1.5 cm of the largest one and aggregating volume was about 20 mL. The polyps were composed of irregularly distributed endometrial glands and prominent bundles of smooth muscle cells in the stroma as well as combined plasma cells. Theses bundles of smooth muscle cells were variable in proportion. The endometrial glands revealed cellular proliferation and focal glandular crowding. Also, relatively usual endometrial polyps were present around adenomyomatous polyps (Fig. 1). More than 8 polyps were found at the duodenum and resected polyps showed hyperplastic and dilated glands with intervening smooth muscle bundles which were compatible with hamartomatous polyp (Fig. 2). Two years after surgery, there was no recurrence of symptoms and no thickened uterine endometrium on regular ultrasonographic examination but amenorrhea continued after resectoscopy without menopausal symptoms. Because the patient wants to preserve uterus, even though there are the risk of endometrial cancer, the prophylactic hysterectomy is not performed.
This case is considered to be the second endometrial adenomyomatous polyp in patient with PJS on literature review. PJS can cause tumor in genital tract in addition to gastrointestinal tract, which is often precancerous. It is known that the occurrence of such cancer is fifteen times more likely compared to the general population. Even though gynecologic neoplasms related to PJS include cervical adenocarcinoma, endometrial cancer, epithelial ovarian tumor, sex cord stromal ovarian tumor, etc., specific occurrence rate is unknown [1-3].
Endometrial polyp is frequent lesion in uterus, which shows histologically focal hyperplasia of basalis with a localized overgrowth of gland, stroma, and blood vessels. Adenomyomatous polyp has an overgrowth of benign smooth muscle cell as a component of endometrial polyp. The incidence is known to be very low, with its 1.3% proportion of polyp lesion [4].
Nasu et al. [5] reported nine cases of adenomyomatous polyp which showed abnormal uterine bleeding and dysmenorrhea in 1994. Five among them received hysterectomy, while the remaining four received polypectomy. All the polypoid lesion showed the composition of smooth muscle cell and endometrial gland, while no atypia was observed. Meanwhile, the adenomyomatous polyp is known to be related to the hormonal therapy such as Tamoxifen. Takeuchi et al. [6] reported a patient who after tamoxifen treatment, had heterogenous hyperechoic mass in uterus. The lesion revealed adenomyomatous polyp with small cystic lesion after hysterectomy. According to de Brux [7] it is still unsolved question whether the adenomyomatous polyp is a variant of adenomyosis, endometriosis or a truly neoplastic one. According to Silverberg and Kurman [8] adenomyomatous polyp is harmatomatous and one of the variants of adenomyosis. As a supporting evidence, Nasu et al. [5] reported that the smooth muscle cell element, one of the histological features of adenomyomatous polyp, arise in myometrium. Transvaginal ultrasonogram can be used in diagnosing adenomyomatous polyp. In this case typical mole-like appearance was observed. Furuhashi et al. [9] reported a case of adenomyomatous polyp showing vesicle pattern similar to hydatidiform mole. Treatment includes polypectomy and hysterectomy with purpose of improving symptoms or preserving fertility. Hertig and Gore reported that adenomyomatous polyp usually develops among infertile young patients [10]. However, only one out of nine was nulligravida in a case reported by Nasu et al. [5]. It is also possible that adenomyomatous polyp in PJS is one of the manifestations similar to harmatomatous polyp in gasgtrointestinal tract. Even though atypia is not observed histologically in case of adenomyomatous polyp, there are reports of endometrial cancer in PJS. Hence, close follow-up for the cancerous condition in genital tract is required.
In conclusion, the adenomyomatous polyp in PJS is very rare disease and this lesion may be related with harmatomatous lesion which occurs in PJS.
Figures and Tables
Fig. 1
Adnomyotous polyps characterized histologically by the intertwining of smooth muscle, endometrial glands and endometrial stroma. (A) The polyp contains many cystically dilated glands and abundant smooth muscle fibers (H&E, ×40). (B) Insert, The white arrows represent smooth muscle fibers in stroma (H&E, ×40). (C) The brown color in stroma reveals positive reactivity upon smooth muscle actin (immunohistochemistry for smooth muscle actin, ×40).

References
1. Chen KT. Female genital tract tumors in Peutz-Jeghers syndrome. Hum Pathol. 1986. 17:858–861.
2. Giardiello FM, Brensinger JD, Tersmette AC, Goodman SN, Petersen GM, Booker SV, et al. Very high risk of cancer in familial Peutz-Jeghers syndrome. Gastroenterology. 2000. 119:1447–1453.
3. Sato H, Nanjo H, Tanaka H, Tanaka T. Arias-Stella reaction in an adenomyomatous polyp of the uterus. Acta Obstet Gynecol Scand. 2007. 86:106–108.
4. Peterson WF, Novak ER. Endometrial polyps. Obstet Gynecol. 1956. 8:40–49.
5. Nasu K, Sugano T, Miyakawa I. Adenomyomatous polyp of the uterus. Int J Gynaecol Obstet. 1995. 48:319–321.
6. Takeuchi M, Matsuzaki K, Uehara H, Shimazu H, Nishitani H. A case of adenomyomatous polyp of the uterus associated with tamoxifen therapy. Radiat Med. 2005. 23:432–434.
7. De Brux J. Histopathologie gyntcologique. 1971. Paris: Masson.
8. Silverberg SG, Kurman RJ, editors. Atlas of tumor pathology. 1992. 3rd ed. Washington, DC: Armed Forces Institute of Pathology.
9. Furuhashi M, Miyabe Y, Oda H. Adenomyomatous polyp mimicking hydatidiform mole on ultrasonography. Arch Gynecol Obstet. 2000. 263:198–200.
10. Firminger HI. Atlas of tumor pathology. 1968. Washington, DC: Armed Forces Institute of Pathology.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download