This article has been corrected. See "Corrigendum: Correction of the unit for stone size in the ABSTRACT and RESULTS section. The Gachon University Ureteral Narrowing score: A comprehensive standardized system for predicting necessity of ureteral dilatation to treat proximal ureteral calculi" in Volume 57 on page 372.
Abstract
Purpose
For treating proximal ureteral calculi, treatment decision has been known still difficult to choose ureteroscopic lithotripsy (URS) or shockwave lithotripsy. The aims of our study are to identify the possible predictors for necessity of URS and to propose the Gachon University Ureteral Narrowing scoring system (GUUN score) as a helpful predictor.
Materials and Methods
We evaluated 83 consecutive patients who underwent semirigid URS due to proximal ureteral calculi between April 2011 and February 2014 by a single surgeon. We reviewed patient characteristics and pre- and postoperative parameters and surgical records. We divided the patients into 2 groups (group 1, nondilation group; group 2, dilation group) according to whether or not balloon dilation was performed. A stepwise logistic regression was performed to identify the factors that predict dilatation. Receiver operating characteristic (ROC) curves were plotted and areas under the ROC curve (AUC) were calculated to GUUN score.
Results
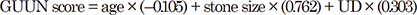
Mean patients' age and their stone size were 48.53±12.90 years and 7.79±2.57 cm, respectively. Significantly smaller stone size (p=0.009), lower stone density (p=0.005), and lower ureteral density differences between ureteral narrowing level and far distal ureter (UD) (p<0.001) were observed in group 1 (n=34) than in group 2 (n=49). GUUN score consists of age, stone size and UD (AUC, 0.938). Overall stone-free clearance rate was 85.5%.
For management of proximal ureteral calculi, there is still controversy with regard to determining which treatment option should be considered the first-line therapy. Some tiny calculi can be managed with medical expulsive therapy without any surgical manipulation. However, it is well known that almost all proximal ureteral calculi over 5 mm in size should be treated using surgical management. Although some studies have suggested that percutaneous antegrade access is more feasible than retrograde ureterolithotripsy for treatment of large, impacted upper ureteral calculi more than 1.5 cm [1], shockwave lithotripsy (SWL) and ureteroscopy (URS) are mainly used in treatment of moderate sized proximal ureteral calculi. According to 2007 American Urological Association (AUA) guidelines for management of ureteral calculi, both SWL and URS showed favorable outcomes as the first-line management [2]. They concluded that overall stone-free clearance rate for proximal ureteral calculi of SWL and URS were 82% and 81%, respectively.
On the other hand, in cases of intractable calculi with SWL, URS may be considered as a second-line therapy. However, in these cases, considering the interval of SWL, delay of treatment from symptom aggravation to stone-free status is inevitable.
Accordingly, from the viewpoint of the urologists, helpful predictors are needed for selection of an optimal treatment modality for treatment of patients who suffered from renal colic due to proximal ureteral calculi in order to minimize treatment delay.
Because flexible URS was introduced according to advancement of technology in medical devices, many studies have reported favorable outcomes for flexible URS for management of urinary stones [3]. However, with consideration for purchasing cost, flexible URS is not always a reasonable option under various medical environments. Rather, semirigid URS may generally be a more feasible option for treatment of ureteral calculi.
Therefore, our study is designed not only to assess the feasibility of semirigid URS but also to investigate helpful predictors for determining proper management for treatment of proximal ureteral calculi.
Our study was approved by the Institutional Review Board of Gachon University Gil Hospital (Incheon, South Korea). We retrospectively collected data for consecutive patients who underwent semirigid URS for management of proximal ureteral calculi between April 2011 and March 2014. All operations were performed with semirigid URS using a holmium: yttrium-aluminum-garnet laser lithotriptor by a single surgeon (JKO). The ureteroscope and holmium laser apparatus used in our study were 9.5 Fr., semirigid type (Karl Storz, Tuttlingen, Germany), OmniPulse (Trimedyne Inc., Irvine, CA, USA), respectively.
In review of preoperative computed tomography (CT) scans, we checked all stone parameters with 3-mm thickness noncontrast CT scan using CT scanner, SOMATOM Definition Flash (Siemens Healthcare Global, Erlangen, Germany) and we also measured region-of-interest (ROI) on magnified image using PiViewSTAR software (INFINITT Healthcare, Seoul, Korea). We defined 'U1' as density of the ureteral area immediately below the ureteral stone and 'U2' as density of the ureteral area on the far distal level, which was identified as the stricture-free level on the CT scan by retrospective review of surgical records. In addition, we defined 'C1' as density of the contralateral ureteral area, which was on the same level of 'U1.' We calculated anatomical parameters using coronal views of the CT scans, including stone size, stone density, skin-to-stone distance, and Hounsfield unit (HFU) of areas U1, U2, and C1 using a previously described method [456]. We designated 'UD' as the difference of HFU between U1 and U2. In addition, we calculated various other formulas using U1, U2, and C1.
We reviewed patient age, sex, body mass index (BMI), stone size, stone laterality, stone density, comorbidities, preoperative urinalysis, level of serum creatinine, presence of previous SWL, surgical records, duration of hospital stay, and postoperative laboratory findings, including serum creatinine required between the 2 groups. We defined stone-free status as no evidence of calculi in the urinary tract on follow-up CT scans.
We divided all patients into 2 groups according to whether or not intraoperative balloon dilation was performed. Group 1 consisted of patients who did not undergo ureteral balloon dilation, and group 2 consisted of patients who underwent ureteral balloon dilation in order to access targeted calculi via a ureteroscope. We compared the above mentioned, various parameters between the 2 groups. In addition, we assessed predictive variables that were helpful in determining the necessity of surgical treatment instead of less invasive management such as SWL.
A descriptive analysis of age, sex, BMI, stone size, and other variables related to CT scans was performed. Analyses of pre- and postoperative parameters between the 2 groups were performed using an independent Student t-test and chi-square test. A p-value of <0.05 was considered statistically significant.
The reliability of the predictors for dilatation was finally assessed by using a bootstrap resampling technique with 1,000 samples [78]. For each sample, a stepwise logistic regression was performed. If the final stepwise model variables occur in a majority (>50%) of the bootstrap models, the original final stepwise regression model can be judged to be stable. Only reliable (bootstrap frequency >50% in 1,000 simulated samples) predictors were used to construct the final aggregate score to predict dilatation.
To identify the score that predicted dilatation, receiver operating characteristic (ROC) curves were plotted and the areas under the ROC curve (AUC) were calculated. To determine the optimal cutoffs for the stone indices, the Youden index (sensitivity + specificity − 1) was calculated, and the corresponding value for the maximum of the Youden index was considered the optimal cutoff point. All statistical analyses were conducted using SAS 9.3 (SAS Institute Inc., Cary, NC, USA).
A total of 83 patients were enrolled in this study. Mean age of patients (±standard deviation) was 49.18 (±12.90) years. There were 52 males and 31 females. Mean stone size and BMI were 7.70 (±2.49) cm and 25.37 (±3.48) kg/m2, respectively. There were 43 left ureteral calculi and 40 right ureteral calculi. Mean stone density was 703.11 (±341.87) HFU. Of the 83 patients, 49 patients underwent ureteral balloon dilation intraoperatively due to luminal narrowing of the ureter. A slightly improved level of serum creatinine was observed postoperatively. Sixteen patients underwent SWL prior to URS. Mean number of previous SWL sessions was 2.2 (±1.8) (Table 1).
For investigation of the optimal variable related to intraoperative ureteral dilation using CT scan, we performed calculations using various formulas using U1, U2, and C1. As a result, UD, which is defined as the difference between U1 and U2, was the most significant parameter among various parameters related to U1, U2, and C1.
When we divided the patients into two groups (group 1, n=34; group 2, n=49) according to the presence of intraoperative ureteral dilation, no statistically significant differences were observed in age, BMI, comorbidities, stone laterality, skin-to-stone density, and duration of hospital stay. However, significantly smaller stone size and lower stone density were observed in group 1 than in group 2 (Table 2).
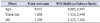
Stone-free clearance rate (%) of groups 1 and 2 was 100 % and 75.5%, respectively (p=0.002). Overall stone-free clearance rate was 85.5%. In group 2, most operations failed due to migration of stone and severe ureteral stricture. Logistic regression analysis was performed for assessment of the most predictive factor for determining selection of surgical manipulation instead of less invasive treatment modalities such as SWL. Using bootstrap resampling technique with 1,000 samples, the final aggregate formula to predict dilatation was made with reliable predictors such as age, stone size, and UD. We named the formula, the Gachon University Ureteral Narrowing (GUUN) score. The GUUN score was calculated the sum of (–0.105) × age, (0.762) × stone size and (0.303) × UD. Cutoff value of GUUN score for predicting ureteral dilatation was 4.86 by using Youden index. Sensitivity and specificity were 0.898 and 0.882, respectively (Fig. 1, Table 3). The GUUN score formula is as follows.
Concerning the ideal management of proximal ureteral calculi, controversy remains with regard to determination of the proper treatment modality [9]. Recent studies have reported that both treatment modalities are effective in treatment of proximal ureteral calculi [10]. Moufid et al. [1] reported that percutaneous anterior access was more feasible than URS for management of large, impacted proximal ureteral calculi over 1.5 cm in size. In their study, URS showed a failure rate of 33% due to stone migration. Using randomized, prospective methods in a study with 48 patients, Lopes Neto et al. [10] reported that laparoscopic ureterolithotomy showed the highest stone-free success rate and fewer surgical procedures among URS, SWL, and laparoscopic ureterolithotomy.
However, many studies compared the treatment outcomes of URS with those of SWL. In their meta-analysis, Picozzi et al. [1112] reported stone-free clearance rates of SWL and URS for treatment of proximal ureteral calculi of 79% (range, 61%–95%) and 81.9% (range, 72%–91.8%). Some studies have demonstrated that both URS and SWL were effective, URS showed a lower retreatment rate than SWL [1314]. Recent AUA guidelines concluded that both SWL and URS are acceptable first-line therapy for management of proximal ureteral calculi. They reported that overall stone-free rates showed no difference between SWL and URS (82% vs. 81%) [2].
However, some problems related to SWL remain. The stone-free rate of SWL for treatment of ureteral stones over 1 cm in size appeared to be poorer despite consideration of AUA guidelines, and some proximal ureteral calculi are refractory to SWL. If concomitant ureteral narrowing is observed, impractical SWL appears to be unnecessary. Actually, in our study, of a total of 83 patients, 49 patients should have undergone concomitant ureteral balloon dilation in order to access targeted stones. The reasons why ureteral dilation was performed were mainly due to facilitate the advancement of ureteroscope. Almost all cases of group 2 showed ureteral luminal narrowing just below the level of ureteral calculi. However, ureteral dilation was needed in the level of distal or midureter because of luminal narrowing and fibrosis of ureter in some cases. In retrospective review of these patients, history of previous urinary calculi was found. Furthermore, the thickness of our semirigid ureteroscope should be considered to access proximal ureter level. Recent study shows 4.5-Fr ultrathin ureteroscope can access ureteral orifice easily without ureteral dilation [15].
The necessity of ureteral dilatation is meaningful because it is strongly related to the high probability of failure of SWL. Accordingly, our study was designed for investigation of a predictor to help in determining URS for proper management of proximal ureteral calculi instead of SWL.
As for the utility of ROI on CT scan, there have been several studies in urologic field [41617]. However, no study has been available related to ureteral density. In our results, U1 showed significant difference between groups 1 and 2. However, wide variations were observed in U1 of same group. Accordingly, we focused on the difference of ROI of same ureter and finally found 'UD' which is defined as the difference of density between U1 and U2 as a significant predictor for determination of whether or not to perform URS.
Therefore, we devised a formula to predict the necessity of ureteral dilatation using UD and suggested cutoff value. By use of GUUN score, our results demonstrated that age, stone size and UD are significant parameters for determining the necessity of URS (AUC, 0.938). Considering the best cutoff value, determination of URS may be recommended if GUUN score is more than 4.86.
According to technical advancement of medical devices, flexible URS was used widely for treatment of proximal ureteral calculi. In a recent study, flexible URS showed both a high stone-free rate (overall, 86 %) and feasibility in obese patients [3]. However, considering the cost of purchase and maintenance of flexible ureteroscopes, flexible URS may not be a generally accepted treatment modality for management of proximal ureteral calculi [18].
Semirigid URS is known to have an advantage in treatment of lower and midureter stones. However, low success rates and high complication rates have been reported in management of proximal ureteral calculi [19]. Nonetheless, semirigid URS has still been regarded as a feasible alternative for management of proximal ureteral calculi in developing countries [20].
Our results showed an overall stone-free clearance rate of 85.5%. The main reason for failure was due to migration of stones. However, some stones with intractable calculi were identified intraoperatively due to severe ureteral stricture after SWL. Considering other results related to semirigid URS, our results for semirigid URS indicate that it is equally safe and feasible. In comparison with SWL of other studies, our results showed a competent stone-free rate. Considering these results, semirigid URS may be a recommendable option in management of proximal ureteral calculi.
To the best of our knowledge, this is the first study to indicate a helpful predictor for use in determining surgical manipulation to treat proximal ureteral calculi. Our results might suggest that GUUN score can predict the necessity of URS using preoperative parameters such as age, stone size and the differences of ureteral density. In addition to the feasibility of noncontrast CT scan of previous studies, our study will be helpful in selection of an optimal treatment modality for management of proximal ureteral calculi.
Figures and Tables
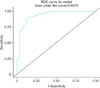 | Fig. 1Receiver operating characteristic (ROC) curves for Gachon University Ureteral Narrowing score system. |
Table 1
Demographic and clinical characteristics (n=83)
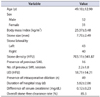
Table 2
Analysis of various parameters between the groups 1 and 2

ACKNOWLEDGMENTS
This work was supported by the Gachon University Research Fund of 2013 (GCU-2013-M031).
References
1. Moufid K, Abbaka N, Touiti D, Adermouch L, Amine M, Lezrek M. Large impacted upper ureteral calculi: A comparative study between retrograde ureterolithotripsy and percutaneous antegrade ureterolithotripsy in the modified lateral position. Urol Ann. 2013; 5:140–146.
2. Preminger GM, Tiselius HG, Assimos DG, Alken P, Buck C, Gallucci M, et al. 2007 guideline for the management of ureteral calculi. J Urol. 2007; 178:2418–2434.
3. Best SL, Nakada SY. Flexible ureteroscopy is effective for proximal ureteral stones in both obese and nonobese patients: a two-year, single-surgeon experience. Urology. 2011; 77:36–39.
4. Perks AE, Schuler TD, Lee J, Ghiculete D, Chung DG, D'A Honey RJ, et al. Stone attenuation and skin-to-stone distance on computed tomography predicts for stone fragmentation by shock wave lithotripsy. Urology. 2008; 72:765–769.
5. Kim TB, Lee SC, Kim KH, Jung H, Yoon SJ, Oh JK. The feasibility of shockwave lithotripsy for treating solitary, lower calyceal stones over 1 cm in size. Can Urol Assoc J. 2013; 7:E156–E160.
6. Singh V, Sinha RJ, Gupta DK, Kumar M, Akhtar A. Transperitoneal versus retroperitoneal laparoscopic ureterolithotomy: a prospective randomized comparison study. J Urol. 2013; 189:940–945.
7. Blackstone EH. Breaking down barriers: helpful breakthrough statistical methods you need to understand better. J Thorac Cardiovasc Surg. 2001; 122:430–439.
8. Grunkemeier GL, Wu Y. Bootstrap resampling methods: something for nothing? Ann Thorac Surg. 2004; 77:1142–1144.
9. Aravantinos E, Anagnostou T, Samarinas M, Ioannides K, Ziavliakis K, Ntafos A, et al. Two-step minipercutaneous ureterolithotripsy under multimodal analgesia for complicated impacted calculi in proximal ureter. Urology. 2013; 81:1147–1152.
10. Lopes Neto AC, Korkes F, Silva JL 2nd, Amarante RD, Mattos MH, Tobias-Machado M, et al. Prospective randomized study of treatment of large proximal ureteral stones: extracorporeal shock wave lithotripsy versus ureterolithotripsy versus laparoscopy. J Urol. 2012; 187:164–168.
11. Picozzi SC, Ricci C, Gaeta M, Casellato S, Stubinski R, Bozzini G, et al. Urgent ureteroscopy as first-line treatment for ureteral stones: a meta-analysis of 681 patients. Urol Res. 2012; 40:581–586.
12. Picozzi SC, Ricci C, Gaeta M, Casellato S, Stubinski R, Ratti D, et al. Urgent shock wave lithotripsy as first-line treatment for ureteral stones: a meta-analysis of 570 patients. Urol Res. 2012; 40:725–731.
13. Youssef RF, El-Nahas AR, El-Assmy AM, El-Tabey NA, El-Hefnawy AS, Eraky I, et al. Shock wave lithotripsy versus semirigid ureteroscopy for proximal ureteral calculi (<20 mm): a comparative matched-pair study. Urology. 2009; 73:1184–1187.
14. Khalil M. Management of impacted proximal ureteral stone: Extracorporeal shock wave lithotripsy versus ureteroscopy with holmium: YAG laser lithotripsy. Urol Ann. 2013; 5:88–92.
15. Söylemez H, Yıldırım K, Utangac MM, Aydoğan TB, Ezer M, Atar M. A new alternative for difficult ureter in adult patients: no need to dilate ureter via a balloon or a stent with the aid of 4.5F semirigid ureteroscope. J Endourol. 2016; 30:650–654.
16. Motley G, Dalrymple N, Keesling C, Fischer J, Harmon W. Hounsfield unit density in the determination of urinary stone composition. Urology. 2001; 58:170–173.
17. Ciudin A, Luque Galvez MP, Salvador Izquierdo R, Franco de Castro A, Garcia-Cruz E, Alcover García J, et al. Unenhanced CT findings can predict the development of urinary calculi in stone-free patients. Eur Radiol. 2012; 22:2050–2056.
18. Collins JW, Keeley FX Jr, Timoney A. Cost analysis of flexible ureterorenoscopy. BJU Int. 2004; 93:1023–1026.
19. Yencilek F, Sarica K, Erturhan S, Yagci F, Erbagci A. Treatment of ureteral calculi with semirigid ureteroscopy: where should we stop? Urol Int. 2010; 84:260–264.
20. Khairy-Salem H, el-Ghoneimy M, el-Atrebi M. Semirigid ureteroscopy in management of large proximal ureteral calculi: is there still a role in developing countries? Urology. 2011; 77:1064–1068.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download