Abstract
Purpose
The purpose of this study was to identify the lower limb lymphedema (LLL) and quality of life in gynecologic cancer patients.
Methods
A sample of 143 patients who have received pelvic lymphadenectomy and/or para-aortic lymphadenectomy recruied in the descriptive study. The instruments used were the Korean Version of the Gynecologic Cancer Lymphedema Questionnaire (GCLQ-K) and the European Organization for Research and Treatment of Cancer QOL Questionnaire-C30 (EORTC QLQ C-30).
Results
The level of LLL for all patients was 4.31±3.86. The level of GCLQ-K score was higher in the LLL group than the non LLL group (8.38±2.92 vs 1.76±1.41). The all functional scale score was lower in the LLL group than the non LLL group, and all symptom scale score except for appetite loss and financial difficulties was higher in the LLL group than the non LLL group. The global health status score was lower in the LLL group than the non LLL group.
Conclusion
The above results show that in the LLL patients after pelvic and/or para-aortic, lymphadenectomy was common. The quality of life was lower in the LLL group than the non LLL group. It is important to develop nursing intervention regarding prevention and management about LLL in gynecologic cancer patients.
Figures and Tables
Table 1
General Characteristics of Participants (N=143)

Table 2
Lower Limb Lymphedema of Participants (N=143)

Table 3
Lower Limb Lymphedema according to General Characteristics (N=143)

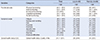
Table 4
Level of Lower Limb Lymphedema and Quality of Life (N=143)

Table 5
Correlation between Lower Limb Lymphedema and Quality of Life (N=143)
References
1. National Cancer Center, Korea Central Cancer Registry. Annual report of cancer statistics in Korean 2013 [Internet]. Accessed December 10, 2015. Available from: http://ncc.re.kr/cancerStatsList.ncc?searchKey=total&searchValue=&pageNum=1.
2. Brearley SG, Stamataki Z, Addington-Hall J, Foster C, Hodges L, Jarrett N, et al. The physical and practical problems experienced by cancer survivors: a rapid review and synthesis of the literature. Eur J Oncol Nurs. 2011; 15:204–212.

3. Dunberger G, Lindquist H, Waldenström AC, Nyberg T, Steineck G, Åvall-Lundqvist E. Lower limb lymphedema in gynecological cancer survivors--effect on daily life functioning. Support Care Cancer. 2013; 21:3063–3070.

4. McGarvey AC, Osmotherly PG, Hoffman GR, Chiarelli PE. Lymphoedema following treatment for head and neck cancer: impact on patients, and beliefs of health professionals. Eur J Cancer Care (Engl). 2014; 23:317–327.

5. Köhler C, Klemm P, Schau A, Possover M, Krause N, Tozzi R, et al. Introduction of transperitoneal lymphadenectomy in a gynecologic oncology center: analysis of 650 laparoscopic pelvic and/or paraaortic transperitoneal lymphadenectomies. Gynecol Oncol. 2004; 95:52–61.

6. Achouri A, Huchon C, Bats AS, Bensaid C, Nos C, Lécuru F. Complications of lymphadenectomy for gynecologic cancer. Eur J Surg Oncol. 2013; 39:81–86.

7. Beesley V, Janda M, Eakin E, Obermair A, Battistutta D. Lymphedema after gynecological cancer treatment : prevalence, correlates, and supportive care needs. Cancer. 2007; 109:2607–2614.
8. Brown JC, Chu CS, Cheville AL, Schmitz KH. The prevalence of lymphedema symptoms among survivors of long-term cancer with or at risk for lower limb lymphedema. Am J Phys Med Rehabil. 2013; 92:223–231.

9. Brown JC, John GM, Segal S, Chu CS, Schmitz KH. Physical activity and lower limb lymphedema among uterine cancer survivors. Med Sci Sports Exerc. 2013; 45:2091–2097.

10. Carter J, Raviv L, Appollo K, Baser RE, Iasonos A, Barakat RR. A pilot study using the Gynecologic Cancer Lymphedema Questionnaire (GCLQ) as a clinical care tool to identify lower extremity lymphedema in gynecologic cancer survivors. Gynecol Oncol. 2010; 117:317–323.

11. Finnane A, Hayes SC, Obermair A, Janda M. Quality of life of women with lower-limb lymphedema following gynecological cancer. Expert Rev Pharmacoecon Outcomes Res. 2011; 11:287–297.

12. Kang SH, Hwang KH, Sim YJ, Jeong HJ, Lee TH, Kim SH. The prevalence and risk factors of lower limb lymphedema in the patients with gynecologic neoplasms. Korean J Obstet Gynecol. 2009; 52:815–820.
13. Yang HS, Lee K, Kim DS, Sim YJ, Jeong HJ, Kim GC, et al. The association of social support and quality of life in gynecological cancer related of lymphedema in a hospital: a pilot study. Korean J Obstet Gynecol. 2011; 54:355–360.

14. Hyun HY, Yeom CH, Lee HR. The treatment effect of the complex lymphatic therapy for lymphedema. J Korean Acad Fam Med. 2002; 23:646–651.
15. Cho MO, Jung HM, Jun JY, Sohn SK, Yoo YJ, No MY, et al. A study on self-care among the lymphedema patients. J Korean Acad Adult Nurs. 2003; 15:383–392.
16. Rowlands IJ, Beesley VL, Janda M, Hayes SC, Obermair A, Quinn MA, et al. Quality of life of women with lower limb swelling or lymphedema 3-5 years following endometrial cancer. Gynecol Oncol. 2014; 133:314–318.

17. Erickson VS, Pearson ML, Ganz PA, Adams J, Kahn KL. Arm edema in breast cancer patients. J Natl Cancer Inst. 2001; 93:96–111.

18. Lockwood-Rayermann S. Lymphedema in gynecologic cancer survivors: an area for exploration? Cancer Nurs. 2007; 30:E11–E18.
19. Lim MC, Lee JS, Joo J, Park K, Yoo HJ, Seo SS, et al. Development and evaluation of the Korean version of the Gynecologic Cancer Lymphedema Questionnaire in gynecologic cancer survivors. Gynecol Oncol. 2014; 133:111–116.

20. Hammer SM, Brown JC, Segal S, Chu CS, Schmitz KH. Cancer-related impairments influence physical activity in uterine cancer survivors. Med Sci Sports Exerc. 2014; 46:2195–2201.

21. Yun YH, Park YS, Lee ES, Bang SM, Heo DS, Park SY, et al. Validation of the Korean version of the EORTC QLQ-C30. Qual Life Res. 2004; 13:863–868.

22. Kim SI, Lim MC, Lee JS, Lee Y, Park K, Joo J, et al. Impact of lower limb lymphedema on quality of life in gynecologic cancer survivors after pelvic lymph node dissection. Eur J Obstet Gynecol Reprod Biol. 2015; 192:31–36.

23. Abu-Rustum NR, Alektiar K, Iasonos A, Lev G, Sonoda Y, Aghajanian C, et al. The incidence of symptomatic lower-extremity lymphedema following treatment of uterine corpus malignancies: a 12-year experience at Memorial Sloan-Kettering Cancer Center. Gynecol Oncol. 2006; 103:714–718.

24. Scott NW, Fayers PM, Aaronson NK, Bottomley A, de Graeff A, Groenvold M, et al. EORTC QLQ-C30 reference values. Brussels: EORTC Quality of Life Group;2008.
25. Yang GH, Shim JY. The diagnosis and treatment of lymphedema. J Korean Med Assoc. 2013; 56:1115–1122.

26. Langbecker D, Hayes SC, Newman B, Janda M. Treatment for upper-limb and lower-limb lymphedema by professionals specializing in lymphedema care. Eur J Cancer Care (Engl). 2008; 17:557–564.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download