Abstract
Purpose
Food intake of COPD patients decreases because of appetite loss, depression, and breathing problems while eating, which increase the likelihood of patients becoming malnourished. This study investigated the nutrient intake and dietary quality of people with and without COPD in Korea.
Methods
There were 2,160 adults aged 50 and over who participated in the 5~6th Korea National Health and Nutrition Examination Survey. The subjects were divided into the COPD group and non-COPD group according to the rate of forced expiratory volume at 1 second (FEV1) against forced vital capacity (FVC). Consumption of food and nutrients were calculated based on the nutrition examination survey. Statistical analyses were conducted using SPSS 19.0.
Results
Among individuals in their 50s, intake of vitamin B1 in the COPD group was significantly less than the NCOPD group, while intake of sodium in the COPD group was significantly greater than the NCOPD group. Among individuals in their 60s, the energy intake of the COPD group was significantly less than that of the NCOPD group. The COPD group showed significantly less intake of vitamin B1 and vitamin C, but greater intake of sodium than the NCOPD group. In the group aged 70 and over, The COPD group had significantly less intake of vitamin B1 than the NCOPD group and showed lower nutrient adequacy ratio values in protein, vitamin B1, vitamin B2, and iron than the NCOPD group.
Chronic obstructive pulmonary disease (COPD) is a type of obstructive lung disease characterized by irreversible airflow limitation that is induced by damage to airways and lungs caused by chronic inflammation. The most important cause of COPD is smoking; however, there are other factors such as occupational exposure to risk factors, indoor air pollution and infection.1 A 2014 report by the World Health Organization (WHO) revealed that COPD was the third most common cause of death following ischemic heart disease and strokes.2 The prevalence of COPD among Koreans aged 40 and over was 14.2% in 2014; however, its awareness and treatment was 2.9% and 1.6%, respectively, which was much lower than that of other chronic diseases.3
Medications such as bronchodilators, steroids, and antibiotics have been the primary treatment for COPD; however, the need for and importance of nutrition therapy is currently attracting attention.4 Patients with COPD need more energy because of the extra effort involved in breathing and generalized inflammatory response; however, their food intake decreases because of loss of appetite, depression, decreased physical activity, and breathing problems while eating, which increase the likelihood of the patients becoming malnourished.56 Nutritional status is an important factor to determine the symptoms and prognoses of COPD patients,7 and previous research reported malnutrition among COPD patients such as insufficient nutrient intake and weight loss.89 Cochrane10 reported that 23% of COPD patients were malnourished, that the malnourished group showed poorer lung function than the normal group and that they experienced difficulties in eating food.
The main purpose of nutrition therapy for COPD is to enhance the function of respiratory muscles by increasing lean body mass and eventually improving the quality of life and life expectancy.4 When malnourished COPD patients are treated with nutrition therapy, their weight can increase and their lung functions can improve in the short term.11 Several results reporting that antioxidants such as vitamin A, vitamin C, vitamin E, and flavonoids are effective at preventing COPD have recently been released.12 However, the positive effects of each individual nutrient have not been sufficiently studied to reach a conclusion.13
A carbohydrate based diet is not recommended for COPD patients because it generates more carbon dioxide,14 but the Korean diet, which mostly consists of carbohydrates, tends to include insufficient protein and fat.15 Thus, proper nutritional education and nutritional interventions for COPD patients are necessary, but research into nutritional status, dietary status, and dietary quality of COPD patients in Korea is currently insufficient. For this reason, the present study examined and assessed nutrient and food intake and dietary quality of Korean adults aged 50 and over according to COPD, and investigated their nutritional status and nutrient intake by age group.
This study utilized data from the 5~6th Korea National Health and Nutrition Examination Survey. The subjects for this study were 2,160 adults aged 50 and over who participated in the 5th Korea National Health and Nutrition Examination Survey (2012) or the 6th Korea National Health and Nutrition Examination Survey (2013~2014). The subjects were divided into the COPD group and NCOPD group according to the rate of forced expiratory volume at 1 second (FEV1) against forced vital capacity (FVC), which is the criterion suggested by Global Initiatives for Obstructive Lung Disease (GOLD).16 Subjects who recorded lower than 70% FEV1/FVC were classified as belonging to the COPD group, while those who showed 70% or higher FEV1/FVC and were not diagnosed with any diseases affecting food intake, such as cardiovascular disease, respiratory diseases, neurologic/sensory disorders, urogenital diseases, endocrine metabolic disorders, and cancer, were classified as the NCOPD group.
Fundamental variables for this study include sociodemographic variables (age, sex, residence, educational level, occupation, and household income). Educational level was divided into elementary school or lower, middle school, high school, and college graduation or higher. Occupation was divided into white collar work, blue collar work, and unemployed. Household income was divided into low, middle-low, middle-high, and high according to the quartile of household income.
Body measurements such as height, weight, body mass index (BMI), and waist circumference were analyzed based on the results of a medical examination. BMI measurements were divided into underweight (BMI < 18.5), normal weight (18.5 ≤ BMI < 23), overweight (23 ≤ BMI < 25), and obese (BMI ≥ 25).17
Dietary information such as frequency of eating out was provided through dietary behavior survey items in the nutrition examination survey. Information regarding the frequency of alcohol intake, smoking habits and exercise frequency was provided through a health-related behavior survey.
The results of the medical examination were used for clinical index analysis. The examination included final systolic blood pressure, final diastolic blood pressure, total cholesterol, HDL-cholesterol, LDL-cholesterol, triglyceride, fasting glucose level, and HbA1c. LDL-cholesterol was calculated using the Freidewald equation18 {LDL-cholesterol = total cholesterol-HDL-cholesterol-(triglyceride / 5)}.
Consumption of food and nutrients was calculated based on the raw data of the nutrition examination survey, which used the 24-hour recall method. Briefly, food was divided into 18 groups (cereals and grain products, potatoes and starches, sugars and sweets, legumes and their products, seeds and nuts, vegetables, mushrooms, fruits, meats and their products, eggs, fish and shellfish, seaweeds, milk and dairy products, oils and fats, beverages, seasonings, prepared foods, and others) and consumption of each group was analyzed.
The nutrient adequacy ratio (NAR) was calculated for nine nutrients (protein, vitamin A, vitamin B1, vitamin B2, niacin, vitamin C, calcium, phosphorus, and iron) to assess the adequacy of nutrient intake. The upper limit of the calculated NAR values was set at 1, and if the ratio values were greater than 1, they were regarded as 1. The mean adequacy ratio (MAR) was calculated to assess general nutrient consumption.19
All statistical analyses were conducted using SPSS Ver. 19.0 (International Business Machines Corp., Armonk, NY, USA). The chi-squared test was used to test distribution differences of categorical variables in each group, and the independent t-test was used to test the mean differences of continuous variables. When the differences were tested, covariates (age, energy intake) that can affect clinical indices, body measurements, and nutrient and food consumption were included in the analysis model to correct their effects, and the corrected values were presented. Clinical indices and body measurements were adjusted by sex and age, and nutrient and food consumption were adjusted by age, sex and daily energy intake. Participants were divided into three groups: 50s, 60s and 70 and over to identify differences in nutrient intake by age group. When the p-value was lower than 0.05, it was regarded as a significant difference.
The general characteristics of the subjects are shown in Table 1. The average age was significantly higher in the COPD group than the NCOPD group (p < 0.001). The higher the age of the subjects, the more likely they would be in the COPD group (p < 0.001). Within the NCOPD group, 45.7% of respondents were male and 54.3% were female. In the COPD group, the males consisted of 72.5% and the females 27.5%. Therefore, males showed a significantly higher ratio of COPD than that of females, overall (p < 0.001).
More people lived in urban areas than in rural areas in both groups; however, population size did not differ significantly. There was a significant difference in the educational level between two groups (p < 0.001). Specifically, the rate of higher than high school education in the COPD group (38.4%) was lower than in the NCOPD group (59.1%). Regarding occupation, the rate of white collar workers was greater in the NCOPD group (16.3%) than the COPD group (8.3%), and the rate of unemployed was greater in the COPD group (43.6%) than the NCOPD group (34.5%) (p < 0.001). Comparison of household income revealed that the rate of respondents answering middle-high or high was greater in the NCOPD group (62.8%) than the COPD group (42.6%), while the rate of subjects answering middle-low or low was greater in the COPD group (57.4%) than in the NCOPD group (37.3%) (p < 0.001).
There was no significant difference in weight between groups, but the COPD group had significantly greater waist circumferences than the NCOPD group (p < 0.05). There were no differences in the mean of BMI, or the BMI distribution between the NCOPD group and the COPD group.
Health-related behaviors according to COPD are shown in Table 2. The rate of ex-smokers or current smokers was greater in the COPD group (66.9%) than the NCOPD group (39.1%) (p < 0.001). Additionally, in alcohol drinking, the rate of respondents answering 2–4 times per month or more than 2 or more times per week was greater in the COPD group (48.1%) than the NCOPD group (40.7%) (p < 0.001). There were no significant differences in the frequency of eating out or exercise between groups.
Clinical indices according to COPD are shown in Table 3. There were no significant differences in diastolic pressure, HDL-cholesterol, LDL-cholesterol, or triglycerides between groups. Systolic pressure (p < 0.05), fasting blood glucose (p < 0.05), HbA1c (p < 0.01) were significantly higher in the COPD group than the NCOPD group, while total cholesterol (p < 0.01) was significantly lower in the COPD group than the NCOPD group.
Daily nutrient intake of the subjects by age group is shown in Table 4. Among those in their 50s, the COPD group had significantly less intake of vitamin B1 (p < 0.001) than the NCOPD group, while the vitamin A (p < 0.05) and sodium intake in the COPD group was significantly greater than in the NCOPD group (p < 0.05). Among those aged 60~69, the average energy intake of the COPD group (1,892.99 kcal) was significantly less than that of the NCOPD group (2,132.30 kcal) (p < 0.01). The COPD group showed significantly less intake of vitamin B1 (p < 0.001) and vitamin C (p < 0.05), but greater intake of sodium (p < 0.05) than the NCOPD group. Among those aged 70 and over, the COPD group had significantly less intake of vitamin B1 (p < 0.01) than the NCOPD group. There was no difference in the ratio of carbohydrate, protein and fat intake between groups.
The results of NAR and MAR analysis of the subjects are shown in Table 5. The COPD group showed lower NAR values in protein (p < 0.05), vitamin B1 (p < 0.001), vitamin B2 (p < 0.01), and iron (p < 0.001) than the NCOPD group. The COPD group showed lower MAR values than the NCOPD group (p < 0.05).
With regard to food consumption (Table 6), consumption of potatoes and starches (p < 0.05), and fruits (p < 0.01) was significantly lower in the COPD than the NCOPD group. There were no statistical significances in other food groups.
This study investigated differences in the nutrient/food intake and dietary quality of Koreans aged 50 and over according to whether they were with or without COPD. The Korean Academy of Tuberculosis and Respiratory Diseases divided risk factors for COPD into host factors (genes, age and sex) and external factors (smoking, external harmful substances, socioeconomic level and respiratory infection).1 Age is an important risk factor for COPD, which is supported by studies conducted in Korea.20 In this study, revealed that the majority of the NCOPD group was in their 50s, while the majority of the COPD group was aged 60 and over. Moreover, there was a significant difference between male and female groups. COPD is believed to be more prevalent among men than women, which is usually attributed to higher smoking rates and more frequent occupational exposures of significance for men.1 Additionally, poverty is an external risk factor for COPD. Previous studies2021 have reported that, as the socioeconomic level decreases, the chances of getting lung diseases increases. This study found similar results, but the relationship between socioeconomic level and exposure to indoor/outdoor air pollution, nutrition status or infection is not clear.
The rate of ex-smokers or current smokers was greater in the COPD group than the NCOPD group. The most important and well-known risk factor for COPD is smoking. Among Korean males aged 50 or older, the possibility of getting COPD is 2.1 times higher among smokers and 1.5 times higher among ex-smokers than non-smokers, which means smoking has a significant effect on the likelihood of developing COPD.22 The main cause of COPD is smoking in Korea and most advanced countries, so quitting smoking is vital to preventing COPD.2
There was no significant difference in frequency of exercise between groups. The most noticeable characteristic of COPD is difficulty in breathing and decreased activity. As COPD develops, breathing difficulties become severe and activity ability decreases, which results in a decrease in exercise.23 It has been reported that when nutrition therapy and exercise therapy are carried out at the same time by COPD patients, their lean body mass increases and respiratory muscles strengthen.24 Thus, COPD patients should increase their frequency of proper exercise to rehabilitate their breathing. Moreover, if nutrition therapy is carried out at the same time, this will be more effective.
The COPD group had higher systolic blood pressure than that of the NCOPD group.25 Considering that hypertension is the most common disease that COPD patients in Korea suffer from (51% of all COPD patients) and that it affects prognosis, blood pressure management seems to be necessary.126 Total cholesterol was greater in the NCOPD group than the COPD group, but the levels of both groups were included in the normal level.27 Ivanovska28 reported that total cholesterol and LDL-cholesterol levels of severe COPD patients were significantly higher, which is different from the results of this study. Fasting blood glucose and HbA1c was greater in the COPD group than the NCOPD group, and both groups were pre-diabetic.29 Diabetes is common in COPD patients, and diabetes can have a negative impact on the prognosis of COPD patients. Thus, it is necessary to systematically regulate blood glucose through adequate nutrient intake, diet improvement, and light physical activity.1
The energy intake of the COPD group tended to decrease as age increased. Among those in their 60s, the energy intake of the COPD group was significantly lower than that of the NCOPD group. This was higher than the daily calorie intake of COPD patients reported by Lee30; however, considering that the average energy requirements for Koreans aged 50 and over are 2,000~2,200 kcal for males and 1,600~1,800 kcal for females, the energy intake of subjects with COPD is not sufficient.31 It is common for COPD patients to have difficulty breathing while eating, as well as indigestion, fatigue and depression, and these symptoms are all related to a decrease in energy intake.4 Thus, proper nutritional intervention is needed for patients with COPD.
There was no significant difference in the daily intake of carbohydrates, proteins and fats or their energy ratio between groups. A previous study3 suggested that COPD patients should take a maximum of 50% of their energy from carbohydrates because excessive intake of carbohydrates can increase carbon dioxide production. The present study revealed that the rate of carbohydrate intake in the COPD group was about 70%, indicating that nutritional intervention and education for proper carbohydrate intake is required.
The intake of potatoes and starches, fruits was significantly lower in the COPD group than in the NCOPD group, and the intake of seaweeds tended to be lower in the COPD group than in the NCOPD group. Insufficient intake of fruits and seaweeds in the COPD group are probably related to insufficient intake of certain vitamins. A previous study32 reported that the intake of crude fiber, vitamin B2, folic acid and potassium in all clinical stages of the COPD group fell short of their average requirements, and another study8 on elderly also showed the COPD group consumed less calcium, phosphorus, folic acid, cholecalciferol, retinol and vitamin B1 than the same age group. Other studies1233 have shown that a diet with sufficient fruits and vegetables can improve generalized infection and help to treat respiratory disease, in particular, to improve pulmonary function. Thus, a diet with plentiful fruits and vegetables should be recommended to COPD patients to encourage them to consume sufficient vitamins and minerals.
Sodium consumption was twice the amount or more than the WHO recommended intake of 2,000 mg in both the COPD group and NCOPD group.34 Intake of sodium in the COPD group was significantly greater among those in their 50s and 60s group. Excessive sodium consumption can increase the risk of high blood pressure, and hypertension is the most common disease of COPD patients in Korea; thus, the intake of sodium should be carefully controlled.126
There was no significant difference in calcium intake between the two groups, but the NAR values of the two groups were around 0.6, indicating that the calcium intake is severely insufficient. COPD patients experience a decrease in exercise and weak skeletal muscles, which results in an increase in the risk of developing osteoporosis. As osteoporosis is the main cause of comorbidity in COPD,126 proper nutritional intervention for the COPD group to provide calcium is required.
It is difficult to confirm the causal relationship between COPD prevalence and nutrient intake or diet quality because of the limitations of this cross-sectional study. Moreover, because food intake data used in this study was based on results of a survey conducted using the 24-hour recall method for one day, the data do not represent individuals' daily intakes. However, this study analyzed the relationships between COPD and diet using the Korea National Health and Nutrition Examination Survey data, which best show the characteristics of the Korean diet, and verified that there are differences in nutrient and food intake according to whether the subjects do or do not have COPD. Based on the not-so-severe stage of COPD among study subjects, it is considered that if the GOLD stage of COPD becomes severe, a more distinct lack of nutrient intake and decrease in dietary quality would be observed.35
In conclusion, the COPD group consumed less energy and fewer of certain nutrients than the NCOPD group among Koreans aged 50 and over, and the quality of their diet was not appropriate; however, there was not much difference between groups. As age increased, patients with COPD had a poorer and less balanced diet than non-COPD adults. Indeed, in patients with COPD, good diet has been associated with better lung function and reduced mortality.36 Patients with COPD are at higher risk for malnutrition, these patients undergo careful assessment and screening to identify those who require dietary intervention. Moreover, more detailed research is needed to determine how individual nutrient intake in COPD patients affects their malnutrition.
This study examined and assessed nutrient and food intake and dietary quality of 2,160 Korean adults aged 50 and over with and without COPD who participated in the Korea National Health and Nutrition Examination Survey. The energy intake of the COPD group tended to decrease as age increased and was significantly less than that of the NCOPD group. Moreover, the ratio of carbohydrate intake in the COPD group was higher than those recommended in COPD patients. The COPD group generally showed lower NAR values than the NCOPD group. The intake of potatoes and starches, fruits was lower in the COPD group than in the NCOPD group. Insufficient intake of fruits in the COPD group is related to low intake of certain vitamins. On the other hand, salt intake was twice that of the WHO recommendations in both groups. Overall, the COPD group consumed less energy and fewer of certain nutrients than the NCOPD group, and the quality of their diet was inadequate; however, there was not much difference between groups. Therefore, it is necessary to study changes in food group intake and nutrient intake due to COPD prevalence. In addition, studies on nutrients that are insufficient in patients with COPD and appropriate intervention are required.
Figures and Tables
Table 1
General characteristics and anthropometric characteristics of the subjects
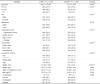
1) COPD: Chronic obstructive pulmonary disease group, NCOPD: Non-chronic obstructive pulmonary disease group 2) Mean ± SE 3) n (%) 4) Adjusted for age, sex 5) Underweight: < 18.5 kg/m2, 18.5 ≤ Normal < 23 kg/m2, 23 kg/m2 ≤ Overweight < 25 kg/m2, Obese: ≥ 25 kg/m2
*p < 0.05, ***p < 0.001, Significant difference by student's t-test, chi-squared test
References
1. The Korean Academy of Tuberculosis and Respiratory Diseases. Guideline of COPD 2014. Revised edition [Internet]. Seoul: The Korean Academy of Tuberculosis and Respiratory Diseases;2016. cited 2016 Nov 4. Available from: http://www.lungkorea.org/bbs/index.html.
2. World Health Organization. Burden of COPD [Internet]. Geneva: World Health Organization;2014. cited 2016 Nov 4. Available from: http://www.who.int/respiratory/copd/burden/en/.
3. Korea Centers for Disease Control and Prevention. The analysis result of 2014 National Health and Nutrition Survey data [Internet]. Cheongju: Korea Centers for Disease Control and Prevention;2015. cited 2016 Nov 4. Available from: https://knhanes.cdc.go.kr/knhanes/index.do.
4. Lee KH. Nutritional management in patients with chronic obstructive pulmonary disease. Yeungnam Univ J Med. 2004; 21(2):133–142.

5. Grönberg AM, Slinde F, Engström CP, Hulthén L, Larsson S. Dietary problems in patients with severe chronic obstructive pulmonary disease. J Hum Nutr Diet. 2005; 18(6):445–452.

6. Schols AM, Buurman WA, Staal van den Brekel AJ, Dentener MA, Wouters EF. Evidence for a relation between metabolic derangements and increased levels of inflammatory mediators in a subgroup of patients with chronic obstructive pulmonary disease. Thorax. 1996; 51(8):819–824.

7. Openbrier DR, Irwin MM, Rogers RM, Gottlieb GP, Dauber JH, Van Thiel DH, Pennock BE. Nutritional status and lung function in patients with emphysema and chronic bronchitis. Chest. 1983; 83(1):17–22.

8. Hallin R, Gudmundsson G, Suppli Ulrik C, Nieminen MM, Gislason T, Lindberg E, Brøndum E, Aine T, Bakke P, Janson C. Nutritional status and long-term mortality in hospitalised patients with chronic obstructive pulmonary disease (COPD). Respir Med. 2007; 101(9):1954–1960.

9. Laudisio A, Costanzo L, Di Gioia C, Delussu AS, Traballesi M, Gemma A, Antonelli Incalzi R. Dietary intake of elderly outpatients with chronic obstructive pulmonary disease. Arch Gerontol Geriatr. 2016; 64:75–81.

10. Cochrane WJ, Afolabi OA. Investigation into the nutritional status, dietary intake and smoking habits of patients with chronic obstructive pulmonary disease. J Hum Nutr Diet. 2004; 17(1):3–11.

11. Whittaker JS, Ryan CF, Buckley PA, Road JD. The effects of refeeding on peripheral and respiratory muscle function in malnourished chronic obstructive pulmonary disease patients. Am Rev Respir Dis. 1990; 142(2):283–288.

12. Keranis E, Makris D, Rodopoulou P, Martinou H, Papamakarios G, Daniil Z, Zintzaras E, Gourgoulianis KI. Impact of dietary shift to higher-antioxidant foods in COPD: a randomised trial. Eur Respir J. 2010; 36(4):774–780.

13. Heyland DK, Dhaliwal R, Suchner U, Berger MM. Antioxidant nutrients: a systematic review of trace elements and vitamins in the critically ill patient. Intensive Care Med. 2005; 31(3):327–337.

14. Cai B, Zhu Y, Ma Y, Xu Z, Zao Y, Wang J, Lin Y, Comer GM. Effect of supplementing a high-fat, low-carbohydrate enteral formula in COPD patients. Nutrition. 2003; 19(3):229–232.

15. Moon HK, Kong JE. Assessment of nutrient intake for middle aged with and without metabolic syndrome using 2005 and 2007 Korean National Health and Nutrition Survey. Korean J Nutr. 2010; 43(1):69–78.

16. Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. GOLD Scientific Committee. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001; 163(5):1256–1276.
17. Korean Society for the Study of Obesity. Guideline of obesity 2012 [Internet]. Seoul: Korean Society for the Study of Obesity;2012. cited 2017 Feb 17. Available from: http://www.kosso.or.kr/general/board/list.html?num=72&start=0&sort=count%20asc&code=general_03&key=&keyword=.
18. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972; 18(6):499–502.

20. Kim DS, Kim YS, Jung KS, Chang JH, Lim CM, Lee JH, Uh ST, Shim JJ, Lew WJ. Korean Academy of Tuberculosis and Respiratory Diseases. Prevalence of chronic obstructive pulmonary disease in Korea: a population-based spirometry survey. Am J Respir Crit Care Med. 2005; 172(7):842–847.
21. Gan WQ, FitzGerald JM, Carlsten C, Sadatsafavi M, Brauer M. Associations of ambient air pollution with chronic obstructive pulmonary disease hospitalization and mortality. Am J Respir Crit Care Med. 2013; 187(7):721–727.

22. Jung IS, Jung IK. Effects of smoking status on chronic obstructive pulmonary disease prevalence in males 40 years and older: findings from the Korean National Health and Nutrition Examination Survey. Korean J Health Promot. 2014; 14(4):155–161.

23. Rochester DF, Braun NM. Determinants of maximal inspiratory pressure in chronic obstructive pulmonary disease. Am Rev Respir Dis. 1985; 132(1):42–47.
24. Schols AM, Soeters PB, Mostert R, Pluymers RJ, Wouters EF. Physiologic effects of nutritional support and anabolic steroids in patients with chronic obstructive pulmonary disease. A placebo-controlled randomized trial. Am J Respir Crit Care Med. 1995; 152(4 Pt 1):1268–1274.

25. The Korean Society of Hypertension. Guideline of hypertension 2013 [Internet]. Seoul: The Korean Society of Hypertension;2013. cited 2017 Feb 17. Available from: http://14.63.223.46/bbs/content_view?post_num=4&bbs=guideline.
26. Fabbri LM, Luppi F, Beghé B, Rabe KF. Complex chronic comorbidities of COPD. Eur Respir J. 2008; 31(1):204–212.

27. The Korean Society of Lipidology and Atherosclerosis. Guideline of dyslipidemia [Internet]. Seoul: The Korean Society of Lipidology and Atherosclerosis;2015. cited 2016 Nov 16. Available from: http://www.lipid.or.kr/bbs/index.html.
28. Zafirova-Ivanovska B, Stojkovikj J, Dokikj D, Anastasova S, Debresliovska A, Zejnel S, Stojkovikj D. The level of cholesterol in COPD patients with severe and very severe stage of the disease. Open Access Maced J Med Sci. 2016; 4(2):277–282.

29. Korean Diabetes Association. Treatment guideline for diabetes 2015 [Internet]. Seoul: Korean Diabetes Association;2015. cited 2017 Feb 17. Available from: http://www.diabetes.or.kr/pro/publish/guide.php?code=guide&mode=view&number=625.
30. Lee H, Kim S, Lim Y, Gwon H, Kim Y, Ahn JJ, Park HK. Nutritional status and disease severity in patients with chronic obstructive pulmonary disease (COPD). Arch Gerontol Geriatr. 2013; 56(3):518–523.

31. Ministry of Health and Welfare (KR). The Korean Nutrition Society. Dietary reference intakes for Koreans 2015. Sejong: Ministry of Health and Welfare;2016.
32. Park YM, Yoon HI, Sohn C, Choue R. Nutritional status of chronic obstructive pulmonary disease patients according to the severity of disease. Korean J Nutr. 2008; 41(4):307–316.
33. Fåk F, Jakobsdottir G, Kulcinskaja E, Marungruang N, Matziouridou C, Nilsson U, Stålbrand H, Nyman M. The physico-chemical properties of dietary fibre determine metabolic responses, short-chain fatty acid profiles and gut microbiota composition in rats fed low- and high-fat diets. PLoS One. 2015; 10(5):e0127252.

34. World Health Organization. Sodium intake for adults and children: guideline [Internet]. Geneva: World Health Organization;2012. cited 2016 Nov 4. Available from: http://www.who.int/nutrition/publications/guidelines/sodium_intake/en/.
35. Yoo KH, Kim YS, Sheen SS, Park JH, Hwang YI, Kim SH, Yoon HI, Lim SC, Park JY, Park SJ, Seo KH, Kim KU, Oh YM, Lee NY, Kim JS, Oh KW, Kim YT, Park IW, Lee SD, Kim SK, Kim YK, Han SK. Prevalence of chronic obstructive pulmonary disease in Korea: the fourth Korean National Health and Nutrition Examination Survey, 2008. Respirology. 2011; 16(4):659–665.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download