Abstract
Purpose
Excess intake of sodium is a major diet-related risk factor for human diseases including hypertension and cancer as well as obesity and inflammation. However, findings are still controversial, and evidence is lacking in Koreans. Therefore, for better understanding of the role of dietary sodium intake in disease etiology, this study investigated the effects of dietary sodium intake on adiposity, inflammation, and hormones in Koreans.
Methods
A total of 80 males and females joined the study. The general characteristics and dietary intake data were investigated by trained interviewers using a questionnaire and 24-h dietary recall, respectively. For the markers of adiposity, body weight, body mass index, percent of body fat, visceral fat area, and waist and hip circumference were measured. For the inflammation and hormone markers, leptin, adiponectin, insulin, tumor necrosis factor-α, and interleukin-6 were also analyzed.
Results
Multivariate linear regression analyses suggested that dietary sodium intake was not associated with adiposity. However, dietary sodium showed a significant association with insulin level: Plasma insulin concentration increased with sodium intake independent of other dietary intake or percent of body fat (β = 0.296, adjusted r2 = 0.276, p < 0.01). Other markers for inflammation and hormonal responses were not associated with dietary sodium intake.
Excess intake of dietary sodium is a major health issue worldwide. Many studies have provided evidence that high dietary sodium affects blood pressure and susceptibility for cardiovascular disease and cancer.12345 The role of dietary sodium in each disease etiology may vary, but the findings from the National Health and Nutrition Examination Survey in the United States were that excess intake of dietary sodium is responsible for a 20% greater risk of all-cause mortality.67
Excess sodium intake is also observed to be associated with obesity. Greater sodium intake was often accompanied by increased body weight.89 This may be simply due to the amount of body fluid retained by the sodium. However, high sodium intake also correlated with consumption of high energy density foods including soft drinks.1011 Furthermore, although there are inconsistencies, dietary sodium intake was associated with body mass index (BMI) and overweight.712 This suggests that dietary sodium plays an intricate physiological role in obesity as well as human metabolism.
Recent studies reported that excess sodium intake may affect innate immunity. In murine explants, high sodium diet was associated with tissue inflammation and autoimmune disease.1314 Findings from human studies were consistent with these reports in that sodium intake correlated with changes in inflammatory markers including tumor necrosis factor-α (TNF-α) and adiponectin.151617 Obesity is considered a low grade of chronic inflammation. Therefore, the increased adipocytes associated with dietary sodium intake may lead to the production of adipokines, which initiate inflammation-related pathophysiological responses.1819 Additionally, few studies reported that dietary sodium intake was associated with insulin level and that abundant dietary sodium increased insulin resistance, key markers for inflammation and endocrine metabolism.202122 In line with these findings, although some evidence suggested that the inflammation responses by sodium level may be obesity independent, we still could not dismiss the potential links underlying dietary sodium, obesity, inflammation, and hormone metabolism.
Korea has among the highest sodium consumption worldwide. Reducing the dietary sodium intake by 3 grams is expected to decrease incidence of hypertension, cardiovascular disease, gastric cancer, and kidney disease, resulting in savings of 12.6 trillion won in health costs.23 Therefore, public health campaigns and nutritional education programs actively aim to reduce national dietary sodium intake. A decreasing trend in sodium intake is evident recently,24 but little is known regarding the relationship of dietary sodium with obesity and other inflammation and hormonal markers in a Korean population. Therefore, to better understand the role of sodium intake in human health and disease, with this study, we investigated the effects of dietary sodium intake on adiposity as well as inflammation and hormonal responses.
This cross-sectional study is a part of the research project The Development of a Sodium Adaptation Index Based on the Dietary Habits of Koreans: A Survey. Details of the project were described elsewhere.25 Briefly, the male and female participants were recruited from Gwangju area, Korea, from May 2014 to April 2015. Participants were limited to individuals aged 19 to 69 years who had not been diagnosed with hypertension, heart failure, diabetes, renal disease, or cancer. Individuals were also excluded who were taking any medicine or who were pregnant or lactating. Lastly, subjects who reported any severe recent change in diet or lifestyle habits were not included in this study.
The Institutional Review Board of Kyungbuk National University approved the study protocols (KNU 2014-0053), and all actual procedures were performed in accordance with the allowed guidelines. All participants provided written informed consent prior to the commencement of the study.
We asked volunteers to answer a questionnaire designed to obtain their sociodemographic and lifestyle information. Trained investigators asked each subject's smoking status, household income, education level, and general physical activity level.
Trained research scientists also collected anthropometrical data. Body weight and height were determined using a weight and height measurement tool (HM-201, Panix, Seoul, Korea). BMI was computed as follows: weight (kg) divided by the square of the height (m). For the waist and hip circumference, a measuring tape was used. Percent body fat and visceral fat area were measured with a body composition analyzer (InBody720, Biospace Co. Seoul, Korea).
We collected dietary intake data using 24-h dietary recall. Specifically, a professional dietitian interviewed each participant on the first day of the study. Dietary intake for target nutrients including sodium potassium and total energy intake were estimated by Computer Aided Nutritional Analysis program (CAN-Pro) version 4.0 (Korean Nutrition Society, Seoul, Korea)
Based on a literature review, we selected body weight, BMI, percent body fat, visceral fat area, and waist and hip circumference as adiposity markers. We also selected, leptin, adiponectin, insulin, TNF-α and interleukin-6 (IL-6) as inflammation and hormone response markers.
Blood samples were taken by venipuncture after a minimum of 12 hours of fasting. Serum plasma or whole blood samples were aliquoted and stored at −80℃ until the assay. We analyzed leptin, adiponectin, TNF-α, C-reactive protein (CRP), and IL-6 using modified enzyme immunoassay with the following commercial kits (BioVendor R&D, Brno, Czech Republic): human leptin ELISA, human adiponectin ELISA, human TNF-alpha ELISA, human CRP ELISA and human IL-6 ELISA. We prepared the samples following the manufacturer's instruction and performed tests with the Multiskan EX ELISA reader (Thermo Electron Corporation, Shanghai, China).
Data on continuous variables are presented as means ± standard deviations, and categorical variables exhibited as number of subjects and percent. We energy adjusted the dietary intake variables before the statistical analysis with Willet's residual method. We primarily conducted Pearson's correlation coefficient analyses to screen for potential associations among the variables with respect to diet, anthropometry, and biochemical markers. We then ascertained the effects of dietary sodium intake on those variables using separate linear regression tests in the presence or absence of covariates. We determined covariates for the models such as age, sex, total energy, and potassium intake. We only added lifestyle covariates (smoking status, household income, educational and general physical activity level) to the models when the ANOVA results for each lifestyle factor were statistically associated with each target variable. We tested for multicollinearity among the covariates prior to the multiple linear regression tests using the condition index (all variables < 90). We used Bonferroni-corrected p values for multiple comparisons. We conducted all statistical analyses using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA) and considered a two-sided p < 0.05 statistically significant.
Table 1 displays the general characteristics of the study participants. The mean age of the subjects was 43.3 ± 14.5 years, and there were equal numbers of males and females, 40 each. Total daily sodium intake of the study subjects was 3,960.1 ± 1,824.3 mg/day, and this was not different from the average intake for Koreans whom we investigated earlier. Mean calorie intake was 1,862.9 ± 556.9 kcal/day. The majority of subjects were nonsmokers (71.3%) and college graduates (55.0%). They also had monthly incomes of less than 2,000,000 won (67.3%) and did not engage in heavy physical activity (70%). The mean BMI was 22.44 ± 3.01, and 18.3% of subjects were obese (BMI > 25, n = 15). The Pearson's coefficient correlation analysis showed that sodium intake was not correlated with energy intake, BMI, or other investigated variables (data not shown), with the exception of insulin concentration (r = 0.410, p < 0.001).
We established linear regression models to verify whether sodium intake affected body size, adiposity, hormones, and inflammation in the presence and absence of covariates (Table 2). The statistical results with respect to body size measurement revealed that dietary sodium intake was not associated with body weight, BMI, percent of body fat, visceral fat area, or waist or hip circumference. The regression models for adiposity, inflammation markers, and hormones, however, suggested that higher dietary sodium intake increased the insulin level (model 1: β = 0.301, adjusted r2 = 0.168, Bonferroni-corrected p < 0.001), and this association held when we adjusted for other dietary and lifestyle factors (model 3: β = 0.295, adjusted r2 = 0.230, Bonferroni-corrected p = 0.011). We did not observe these effects of dietary sodium intake on leptin, adiponectin, TNF-α, or IL-6.
Blood insulin level might be associated with other adiposity and dietary intake factors. Therefore, in order to verify clearer associations between dietary sodium intake and insulin, we established a regression model that incorporated percent body fat and total carbohydrate and fat intake. We found that a significant positive association between dietary sodium and insulin level was retained after we adjusted for those factors (model 2: β = 0.296, adjusted r2 = 0.276) (Table 3).
Excess dietary sodium intake is a critical health issue in Korea. Studies have suggested that increased sodium intake is associated with risk of obesity and inflammation response as well as hypertension and cancer. However, the precise mechanisms of dietary sodium in disease risk are not fully understood. For this reason, it is necessary to collect more comprehensive evidence to evaluate the role of dietary sodium in human metabolism.
In this study, we evaluated the effects of dietary sodium intake on body size and adiposity in addition to hormones and inflammation response. Among the examined variables, only insulin level was associated with dietary sodium intake: Plasma insulin increased with higher sodium intake. Associations between dietary sodium intake and insulin sensitivity or resistance have been observed in previous studies. Although some controversies exist, observational and intervention studies have found that low dietary intake was associated with decreased insulin resistance.20 A number of possible mechanisms have been proposed for the association, including that lower sodium intake decreases leptin, which reduces abdominal fat cells, resulting in lower adiposity and insulin resistance.26 A second proposition is that lower intake of dietary sodium modifies the expression of glucose transporter type-4 protein in adipocytes and may therefore improve insulin sensitivity.27 A final proposed mechanism is that low sodium intake alters the level of angiotensin II, which regulates insulin activity.28 These proposed mechanisms all suggest that lower dietary sodium intake is associated with human glucose and insulin metabolism and could further help to prevent diabetes mellitus and metabolic syndrome. In the present study, we did not assess insulin resistance because we had limited information on blood glucose level. However, the increased insulin levels with higher sodium intake could be evidence for an association between sodium and insulin resistance. The multiple study findings all suggest the importance of reducing dietary sodium intake for human health.
Earlier studies reported that dietary sodium intake was associated with body size including body weight, BMI, and overweight,78 and additional evidence has suggested that increased sodium intake could alter markers for inflammation responses.1229 In the current study, however, dietary sodium intake did not show a significant influence on body weight, BMI, percent body fat, visceral fat area, or waist or hip circumference, and these insignificant associations held even when we considered total energy and dietary intake and lifestyle factors. These limited associations could have resulted from the obesity levels of the study participants. Because chronic inflammation responses could be mediated by obesity status, we intended to perform additional analyses according to obesity level to more precisely verify the associations among dietary sodium, adiposity and inflammation response. However, there were only 15 obese subjects in the study, and therefore, we could not perform the subgroup analyses. High dietary sodium intake and obesity could have shown clear correlations with our study variables, but the subjects did not show extreme sodium intake or high BMI, and this might have been responsible for the minimal association between dietary sodium intake and obesity and inflammation markers. Lastly, the subjects joined the study voluntarily, so they may have been more concerned about their health, diet, and lifestyles than the general population. In short, the study findings did not show clear associations between diet and our examined variables.
For this study, we comprehensively investigated the relationships between dietary sodium intake, adiposity, and inflammation. The study provided preliminary evidence of an association between sodium intake and insulin level but with the limitation discussed above that our study sample was relatively small. A larger study cohort could give better statistical power for the findings. Additionally, there were sex-specific differences in diet and intake, but we could not perform stratified analyses because of the limited numbers of subjects. We therefore considered covariates in the statistical models, but we could not dismiss potential underlying effects. Therefore, our findings should be confirmed in larger, well-designed studies.
In conclusion, our study exhibited that dietary sodium intake was not associated with body size but it did significantly affect plasma insulin level. Considering the importance of insulin for presenting diabetes mellitus and metabolic diseases, this preliminary evidence supports the idea that reducing dietary sodium is a critical diet-related factor in improving public health.
Excess intake of sodium is observed to be a major risk factor in many human diseases, and furthermore, the association between immune responses and sodium intake has been of interest as a potential underlying mechanism of obesity. In this Korean study, we examined the effects of dietary sodium intake on adiposity, inflammation, and hormone markers. Among the examined variables using multivariate linear regression analyses, plasma insulin was the sole marker associated with sodium intake; plasma insulin was higher with higher sodium intake, and this association was independent of other dietary intake and overweight. This increase of insulin level with increased sodium intake could be evidence for a relationship between sodium and insulin resistance. The current study did not exhibit any associations between dietary sodium and obesity or inflammation responses, but it did provide evidence that reducing dietary sodium intake could be effective for preventing diabetes mellitus and other metabolic disorders.
Figures and Tables
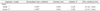
Table 2
Association of dietary sodium intake with measures of body size and inflammation and hormone markers

Dietary sodium intake (g/day) was adjusted for total energy intake using Willet's residual method prior to the analyses.
1) Model 1: crude model 2) Model 2: adjusted for age, sex, total energy and potassium intake 3) Model 3: adjusted for age, sex, total energy and potassium intake, smoking status, household income, education level and general physical activity, as appropriate ***p < 0.001, Bonferroni-corrected p < 0.05
References
1. Stamler J, Cohen J, Culter JA, Grandits G, Kjeldsberg M, Kuller L. Sodium intake and mortality from myocardial infarction: multiple risk factor intervention trial (MRFIT). Can J Cardiol. 1997; 13:Suppl B. 272B.
2. World Health Organization. Guideline: sodium intake for adults and children. Geneva: World Health Organization;2012.
3. Asaria P, Chisholm D, Mathers C, Ezzati M, Beaglehole R. Chronic disease prevention: health effects and financial costs of strategies to reduce salt intake and control tobacco use. Lancet. 2007; 370(9604):2044–2053.

4. Bibbins-Domingo K, Chertow GM, Coxson PG, Moran A, Lightwood JM, Pletcher MJ, Goldman L. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med. 2010; 362(7):590–599.

5. Woo HD, Park S, Oh K, Kim HJ, Shin HR, Moon HK, Kim J. Diet and cancer risk in the Korean population: a meta-analysis. Asian Pac J Cancer Prev. 2014; 15(19):8509–8519.

6. Yang Q, Liu T, Kuklina EV, Flanders WD, Hong Y, Gillespie C, Chang MH, Gwinn M, Dowling N, Khoury MJ, Hu FB. Sodium and potassium intake and mortality among US adults: prospective data from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2011; 171(13):1183–1191.
7. Yi SS, Firestone MJ, Beasley JM. Independent associations of sodium intake with measures of body size and predictive body fatness. Obesity (Silver Spring). 2015; 23(1):20–23.

8. Hoffmann IS, Cubeddu LX. Salt and the metabolic syndrome. Nutr Metab Cardiovasc Dis. 2009; 19(2):123–128.

9. Hulthén L, Aurell M, Klingberg S, Hallenberg E, Lorentzon M, Ohlsson C. Salt intake in young Swedish men. Public Health Nutr. 2010; 13(5):601–605.

10. Libuda L, Kersting M, Alexy U. Consumption of dietary salt measured by urinary sodium excretion and its association with body weight status in healthy children and adolescents. Public Health Nutr. 2012; 15(3):433–441.

11. Yoon YS, Oh SW. Sodium density and obesity; the Korea National Health and Nutrition Examination Survey 2007–2010. Eur J Clin Nutr. 2013; 67(2):141–146.

12. Zhu H, Pollock NK, Kotak I, Gutin B, Wang X, Bhagatwala J, Parikh S, Harshfield GA, Dong Y. Dietary sodium, adiposity, and inflammation in healthy adolescents. Pediatrics. 2014; 133(3):e635–e642.

13. Wu C, Yosef N, Thalhamer T, Zhu C, Xiao S, Kishi Y, Regev A, Kuchroo VK. Induction of pathogenic TH17 cells by inducible salt-sensing kinase SGK1. Nature. 2013; 496(7446):513–517.

14. Kleinewietfeld M, Manzel A, Titze J, Kvakan H, Yosef N, Linker RA, Muller DN, Hafler DA. Sodium chloride drives autoimmune disease by the induction of pathogenic TH17 cells. Nature. 2013; 496(7446):518–522.

15. Rodrigues Telini LS, de Carvalho Beduschi G, Caramori JC, Castro JH, Martin LC, Barretti P. Effect of dietary sodium restriction on body water, blood pressure, and inflammation in hemodialysis patients: a prospective randomized controlled study. Int Urol Nephrol. 2014; 46(1):91–97.

16. Costa AP, de Paula RC, Carvalho GF, Araújo JP, Andrade JM, de Almeida OL, de Faria EC, Freitas WM, Coelho OR, Ramires JA, Quinaglia e Silva JC, Sposito AC. Brasilia Heart Study Group. High sodium intake adversely affects oxidative-inflammatory response, cardiac remodelling and mortality after myocardial infarction. Atherosclerosis. 2012; 222(1):284–291.

17. Yilmaz R, Akoglu H, Altun B, Yildirim T, Arici M, Erdem Y. Dietary salt intake is related to inflammation and albuminuria in primary hypertensive patients. Eur J Clin Nutr. 2012; 66(11):1214–1218.

18. Calder PC, Ahluwalia N, Brouns F, Buetler T, Clement K, Cunningham K, Esposito K, Jönsson LS, Kolb H, Lansink M, Marcos A, Margioris A, Matusheski N, Nordmann H, O'Brien J, Pugliese G, Rizkalla S, Schalkwijk C, Tuomilehto J, Wärnberg J, Watzl B, Winklhofer-Roob BM. Dietary factors and low-grade inflammation in relation to overweight and obesity. Br J Nutr. 2011; 106:Suppl 3. S5–S78.

19. Dobrian AD, Schriver SD, Lynch T, Prewitt RL. Effect of salt on hypertension and oxidative stress in a rat model of diet-induced obesity. Am J Physiol Renal Physiol. 2003; 285(4):F619–F628.
20. Oh H, Lee HY, Jun DW, Lee SM. Low salt diet and insulin resistance. Clin Nutr Res. 2016; 5(1):1–6.

21. Donovan DS, Solomon CG, Seely EW, Williams GH, Simonson DC. Effect of sodium intake on insulin sensitivity. Am J Physiol. 1993; 264(5 Pt 1):E730–E734.

22. Kuroda S, Uzu T, Fujii T, Nishimura M, Nakamura S, Inenaga T, Kimura G. Role of insulin resistance in the genesis of sodium sensitivity in essential hypertension. J Hum Hypertens. 1999; 13(4):257–262.

23. Lee C, Kim DI, Hong J, Koh E, Kang BW, Kim JW, Park HK, Kim CI. Cost-benefit analysis of sodium intake reduction policy in Korea. Korean J Community Nutr. 2012; 17(3):341–352.

24. Kim HJ. Sodium intake status in Korea and plan for improvement of sodium intake estimation in the Korea National Health and Nutrition Examination Survey (KNHANES). Public Health Wkly Rep. 2014; 7(20):425–430.
25. Nam GE, Kim SM, Choi MK, Heo YR, Hyun TS, Lyu ES, Oh SY, Park HR, Ro HK, Han K, Lee YK. Association between 24-h urinary sodium excretion and obesity in Korean adults: a multicenter study. Nutrition. 2017; 41:113–119.

26. Graudal NA, Hubeck-Graudal T, Jurgens G. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst Rev. 2011; (11):CD004022.

27. Fonseca-Alaniz MH, Takada J, Andreotti S, de Campos TB, Campaña AB, Borges-Silva CN, Lima FB. High sodium intake enhances insulin-stimulated glucose uptake in rat epididymal adipose tissue. Obesity (Silver Spring). 2008; 16(6):1186–1192.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download