Abstract
Purpose
The purpose of this study was to evaluate dietary habits, food intakes, nutrient intakes, and diet quality of non-alcoholic fatty liver disease in a health screening and promotion center.
Methods
The total number of study subjects was 10,111 adults, where 3087 subjects (30.5%) were diagnosed as NAFLD. The dietary intakes were obtained using a food frequency questionnaire. They were then compared with the dietary reference intakes could be used in the future for development of diet and nutrition guidelines s (KDRIs).
Results
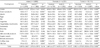
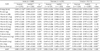
Mean age of subjects in the normal group was 52.9±10.3 yrs and body mass index (BMI) was 22.4 ± 2.6 kg/m2, and those of the NAFLD group were 55.1 ± 9.2 yrs and 25.4 ± 2.9 kg/m2. BMI, blood pressure of the NAFLD group were significantly higher than those of the normal group. The rates of skipping breakfast, overeating, and eating out were significantly could be used in the future for development of diet and nutrition guidelines er in the NAFLD group (p < 0.05, p < 0.000, p < 0.000 respectively). The speed of eating was fast in the NAFLD group (p < 0.000). The NAFLD group consumed significantly higher amounts of grains, meats, fish, seaweeds, kimchies, sugars, sweets, coffee, teas, and oils compared to the normal group (p < 0.05). Meanwhile, intakes of starch products, fruits, milk, and milk products were significantly lower in the NAFLD group compared with those of the normal group (p < 0.05). Riboflavin, calcium, and dietary fiber nutrient adequacy ratio (NAR) of the NAFLD group were significantly lower than those of the normal group. The Korean's dietary diversity score (KDDS) of the NAFLD group was lower than that of the normal group.
Conclusion
In conclusion, we suggest that diet guidelines, such as increasing the intake of calcium and dietary fiber, reducing the intake of energy, fat, and simple carbohydrates, are necessary to improvement of NAFLD. The results could be used in the future for development of diet and nutrition guidelines for NAFLD.
Figures and Tables
References
1. Jun DW. The role of diet in non-alcoholic fatty liver disease. Korean J Gastroenterol. 2013; 61(5):243–251.

2. Ministry of Food and Drug Safety. Influence of dietary intake on non-alcoholic fatty liver disease in Korean. Cheongwon: Ministry of Food and Drug Safety;2012.
3. Jun DW. Diet and exercise in nonalcoholic fatty liver disease. PG Course. 2013; (1):41–45.
4. McCarthy EM, Rinella ME. The role of diet and nutrient composition in nonalcoholic Fatty liver disease. J Acad Nutr Diet. 2012; 112(3):401–409.

5. Machado RM, Stefano JT, Oliveira CP, Mello ES, Ferreira FD, Nunes VS, de Lima VM, Quintão EC, Catanozi S, Nakandakare ER, Lottenberg AM. Intake of trans fatty acids causes nonalcoholic steatohepatitis and reduces adipose tissue fat content. J Nutr. 2010; 140(6):1127–1132.

6. Papandreou D, Karabouta Z, Pantoleon A, Rousso I. Investigation of anthropometric, biochemical and dietary parameters of obese children with and without non-alcoholic fatty liver disease. Appetite. 2012; 59(3):939–944.

7. Shi L, Liu ZW, Li Y, Gong C, Zhang H, Song LJ, Huang CY, Li M. The prevalence of nonalcoholic fatty liver disease and its association with lifestyle/dietary habits among university faculty and staff in Chengdu. Biomed Environ Sci. 2012; 25(4):383–391.
8. Lee JE, Ahn Y, Lee J, Cha JH, Park C, Kimm K. Evaluation of nutrient intake quality over 40 year-old people living in rural and suburban areas. Korean J Community Nutr. 2004; 9(4):491–500.
9. Kim M, Kim J, Bae W, Kim S, Lee Y, Na W, Sohn C. Relationship between nutrients intakes, dietary quality, and serum concentrations of inflammatory markers in metabolic syndrome patients. Korean J Community Nutr. 2011; 16(1):51–61.

10. Seo SH, Lee HW, Park HW, Jang BG, Chung WJ, Park KS, Cho KB, Hwang JS, Ahn SH. Prevalence and associated factors of nonalcoholic fatty liver disease in the health screen examinees. Korean J Med. 2006; 70(1):26–32.
11. Oh SY, Shin MH, Lee SH, Kim JE, Lee HS, Cho JS, Kim HY. The development of food frequency questionnare for nutriton assessment in adults. In : Proceedings of the Korean Society of Health Promotion Conference; 2007 May 19; Seoul. Seoul: Korean Society of Health Promotion.
12. The Korean Nutrition Society. Dietary reference intakes for Koreans, 1st revision. Seoul: The Korean Nutrition Society;2010.
13. Guthrie HA, Scheer JC. Validity of a dietary score for assessing nutrient adequacy. J Am Diet Assoc. 1981; 78(3):240–245.

14. Kant AK, Block G, Schatzkin A, Ziegler RG, Nestle M. Dietary diversity in the US population, NHANES II, 1976-1980. J Am Diet Assoc. 1991; 91(12):1526–1531.

15. Kim IS, Seo EA, Yu HH. A longitudinal study on the change of nutrients and food consumption with advance in age among middle-aged and the elderly. Korean J Community Nutr. 1999; 4(3):394–402.
16. National Institute on Alcohol Abuse and Alcoholism (US). Drinking levels defined [Internet]. Rockville (MD): National Institute on Alcohol Abuse and Alcoholism;2014. cited 2014 May 20. Available from: http://www.niaaa.nih.gov/alcohol-health/overviewalcohol-consumption/moderate-binge-drinking.
17. Korean Association for the Study of the Liver. Clinical practice guidelines for the management of non-alcoholic fatty liver disease. Seoul: Korean Association for the Study of the Liver;2013.
18. Ko ES, Shin JH, Kang EY, Hwang YN, Seo AR, Song SW. Relationship between non-alcoholic fatty liver disease and metabolic syndrome in examiners of a health promotion center in Kyeong-ki do. Korean J Obes. 2008; 17(1):37–44.
19. Jun DW. Non-alcoholic fatty liver disease. Clin Mol Hepatol. 2011; 17(3):s. S332–S336.
20. Yasutake K, Nakamuta M, Shima Y, Ohyama A, Masuda K, Haruta N, Fujino T, Aoyagi Y, Fukuizumi K, Yoshimoto T, Takemoto R, Miyahara T, Harada N, Hayata F, Nakashima M, Enjoji M. Nutritional investigation of non-obese patients with non-alcoholic fatty liver disease: the significance of dietary cholesterol. Scand J Gastroenterol. 2009; 44(4):471–477.

21. Andrade AM, Greene GW, Melanson KJ. Eating slowly led to decreases in energy intake within meals in healthy women. J Am Diet Assoc. 2008; 108(7):1186–1191.

22. Yasutake K, Kohjima M, Kotoh K, Nakashima M, Nakamuta M, Enjoji M. Dietary habits and behaviors associated with nonalcoholic fatty liver disease. World J Gastroenterol. 2014; 20(7):1756–1767.

23. Yamazaki T, Nakamori A, Sasaki E, Wada S, Ezaki O. Fish oil prevents sucrose-induced fatty liver but exacerbates high-safflower oil-induced fatty liver in ddy mice. Hepatology. 2007; 46(6):1779–1790.

24. Zelber-Sagi S, Nitzan-Kaluski D, Goldsmith R, Webb M, Blendis L, Halpern Z, Oren R. Long term nutritional intake and the risk for non-alcoholic fatty liver disease (NAFLD): a population based study. J Hepatol. 2007; 47(5):711–717.

25. Abdelmalek MF, Suzuki A, Guy C, Unalp-Arida A, Colvin R, Johnson RJ, Diehl AM. Nonalcoholic Steatohepatitis Clinical Research Network. Increased fructose consumption is associated with fibrosis severity in patients with nonalcoholic fatty liver disease. Hepatology. 2010; 51(6):1961–1971.

26. Ross AB, Godin JP, Minehira K, Kirwan JP. Increasing whole grain intake as part of prevention and treatment of nonalcoholic Fatty liver disease. Int J Endocrinol. 2013; 2013:585876.

27. Alla V, Bonkovsky HL. Iron in nonhemochromatotic liver disorders. Semin Liver Dis. 2005; 25(4):461–472.

28. Miele L, Dall'armi V, Cefalo C, Nedovic B, Arzani D, Amore R, Rapaccini G, Gasbarrini A, Ricciardi W, Grieco A, Boccia S. A case-control study on the effect of metabolic gene polymorphisms, nutrition, and their interaction on the risk of non-alcoholic fatty liver disease. Genes Nutr. 2014; 9(2):383.

29. Asrih M, Jornayvaz FR. Diets and nonalcoholic fatty liver disease: the good and the bad. Clin Nutr. 2014; 33(2):186–190.

30. Subramanian S, Goodspeed L, Wang S, Kim J, Zeng L, Ioannou GN, Haigh WG, Yeh MM, Kowdley KV, O'Brien KD, Pennathur S, Chait A. Dietary cholesterol exacerbates hepatic steatosis and inflammation in obese LDL receptor-deficient mice. J Lipid Res. 2011; 52(9):1626–1635.

31. Zivkovic AM, German JB, Sanyal AJ. Comparative review of diets for the metabolic syndrome: implications for nonalcoholic fatty liver disease. Am J Clin Nutr. 2007; 86(2):285–300.

32. Panchal SK, Poudyal H, Waanders J, Brown L. Coffee extract attenuates changes in cardiovascular and hepatic structure and function without decreasing obesity in high-carbohydrate, high-fat diet-fed male rats. J Nutr. 2012; 142(4):690–697.

33. Birerdinc A, Stepanova M, Pawloski L, Younossi ZM. Caffeine is protective in patients with non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2012; 35(1):76–82.

34. Hashemi Kani A, Alavian SM, Esmaillzadeh A, Adibi P, Azadbakht L. Dietary quality indices and biochemical parameters among patients with non alcoholic fatty liver disease (NAFLD). Hepat Mon. 2013; 13(7):e10943.

35. Musso G, Gambino R, De Michieli F, Cassader M, Rizzetto M, Durazzo M, Fagà E, Silli B, Pagano G. Dietary habits and their relations to insulin resistance and postprandial lipemia in nonalcoholic steatohepatitis. Hepatology. 2003; 37(4):909–916.

36. Wardlaw GM. Contemporary nutrition. 3rd edition. Madison (WI): Brown & Benchmark;1997.
37. Kim MH, Bae YJ. Evaluation of diet quality of children and adolescents based on nutrient and food group intake and Diet Quality Index-International (DQI-I). Korean J Community Nutr. 2010; 15(1):1–14.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download