Abstract
Protein-energy malnutrition, PEM, and increased hs-CRP level are considered to be associated with increased risk of cardiovascular disease (CVD) in hemodialysis (HD) patients. This is commonly referred to as the vicious circle of malnutrition-inflammation-atherosclerosis cardiovascular disease (MIA syndrome) in chronic kidney disease (CKD). Low protein intake can decrease the serum level of albumin and increase inflammational markers; further, both low serum albumin and high hs-CRP are independent risk factors for all-cause mortality in HD patients. The aim of this study is comparing the serum levels of albumin and hs-CRP in HD patients according to the protein intake levels. The total number of subjects was 60 hemodialysis patients; they were grouped by dietary protein intake: low protein intake group (LPI, protein intake < 1.0 g/kg IBW, 11 men and 19 women) and adequate protein intake group (API, protein intake ≥ 1.0 g/kg IBW, 12 men and 18 women). Blood biochemical parameters, nutrient intake, and dietary behaviors were compared between the LPI and API groups. The LPI group showed a significantly lower serum level of albumin and higher serum level of hs-CRP than the API group (p < 0.05). The LPI group showed a significantly lower intake of most nutrients than the API group (p < 0.05). Index of Nutritional Quality of most nutrients of the LPI and API groups were lower than 1.0. Dietary protein intake was positively correlated with the serum level of albumin (r = 0.306, p < 0.05) and negatively correlated with the serum level of hs-CRP (r = -0.435, p < 0.01). The serum level of hs-CRP was negatively correlated with that of albumin (r = -0.393, p < 0.01). According to these result, serum albumin and hs-CRP in HD patients were influenced by the protein intake levels. To prevent MIA syndrome, it is necessary to improve nutritional status, especially in protein and energy.
Figures and Tables
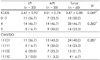
Table 2
Blood biochemical parameters of the subjects according to the protein intake

LPI: Low protein intake (<1.0 g protein/kg IBW), API: Adequate protein intake (≥1.0 g protein/kg IBW)
1) Mean ± SD 2) p value by ANCOVA after adjusting for age, HD duration and intake of medications 3) hs-CRP: high-sensitivity C-reactive protein 4) nPCR: normalized protein catabolic rate 5) BUN: blood urea nitrogen 6) TG: triglyceride 7) TC: total cholesterol 8) HDL-C: high density lipoprotein cholesterol 9) LDL-C: low density lipoprotein cholesterol 10) TIBC: total iron binding capacity
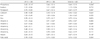
Table 3
Nutrient intakes and frequency of protein foods of the subjects according to the protein intake

Table 4
Assessment of nutrient intakes less than RNI1) and EAR2) of the subjects according to the protein intake n (%)

Table 6
Korean's Dietary Diversity Score (KDDS) and food group intake pattern (CMVDO) of the subjects according to the protein intake n (%)
References
1. Fouque D, Vennegoor M, ter Wee P, Wanner C, Basci A, Canaud B, Haage P, Konner K, Kooman J, Martin-Malo A, Pedrini L, Pizzarelli F, Tattersall J, Tordoir J, Vanholder R. EBPG guideline on nutrition. Nephrol Dial Transplant. 2007; 22:Suppl 2. ii45–ii87.

2. Stenvinkel P, Heimbürger O, Lindholm B, Kaysen GA, Bergström J. Are there two types of malnutrition in chronic renal failure? Evidence for relationships between malnutrition, inflammation and atherosclerosis (MIA syndrome). Nephrol Dial Transplant. 2000; 15(7):953–960.

3. Gallar-Ruiz P, Digioia C, Lacalle C, Rodríguez-Villareal I, Laso-Laso N, Hinostroza-Yanahuaya J, Oliet-Pala A, Herrero-Berron JC, Ortega-Marcos O, Ortiz-Libreros M, Mon-Mon C, Cobo-Jaramillo G, Vigil-Medina A. Body composition in patients on haemodialysis: relationship between the type of haemodialysis and inflammatory and nutritional parameters. Nefrologia. 2012; 32(4):467–476.
4. Kalantar-Zadeh K, Kopple JD, Humphreys MH, Block G. Comparing outcome predictability of markers of malnutrition-inflammation complex syndrome in haemodialysis patients. Nephrol Dial Transplant. 2004; 19(6):1507–1519.

5. Wanner C, Metzger T. C-reactive protein a marker for all-cause and cardiovascular mortality in haemodialysis patients. Nephrol Dial Transplant. 2002; 17:Suppl 8. 29–32.

6. Koch M, Kutkuhn B, Grabensee B, Ritz E. Apolipoprotein A, fibrinogen, age, and history of stroke are predictors of death in dialysed diabetic patients: a prospective study in 412 subjects. Nephrol Dial Transplant. 1997; 12(12):2603–2611.

7. van der Sande FM, Kooman JP, Leunissen KM. The predictive value of C-reactive protein in end-stage renal disease: is it clinically significant? Blood Purif. 2006; 24(4):335–341.

8. Zimmermann J, Herrlinger S, Pruy A, Metzger T, Wanner C. Inflammation enhances cardiovascular risk and mortality in hemodialysis patients. Kidney Int. 1999; 55(2):648–658.

9. Menon V, Greene T, Wang X, Pereira AA, Marcovina SM, Beck GJ, Kusek JW, Collins AJ, Levey AS, Sarnak MJ. C-reactive protein and albumin as predictors of all-cause and cardiovascular mortality in chronic kidney disease. Kidney Int. 2005; 68(2):766–772.

10. Kim S, Sohn C, Chae DW. Comparison of nutritional status and inflammational markers in DM and nonDM hemodialysis patients. Korean J Community Nutr. 2005; 10(5):693–699.
11. K/DOQI guidelines of nutritional in chronic renal failure. Am J Kidney Dis. 2000; 35(6):S20–S21. S28–S29. S32–S33. S40–S41. S44–S45.
12. Aparicio M, Cano N, Chauveau P, Azar R, Canaud B, Flory A, Laville M, Leverve X. French Study Group for Nutrition in Dialysis. Nutritional status of haemodialysis patients: a French national cooperative study. Nephrol Dial Transplant. 1999; 14(7):1679–1686.
13. Yoo HS, Woo HJ, Kang ET, Choue RW. Evaluation of nutritional status and changes of biochemical parameters according to protein intake levels in hemodialysis patients. Korean J Nephrol. 2000; 19(5):769–777.
14. Friedman AN, Fadem SZ. Reassessment of albumin as a nutritional marker in kidney disease. J Am Soc Nephrol. 2010; 21(2):223–230.

15. Korean Dietetic Association. Food composition table for chronic kidney disease. Seoul: Korean Dietetic Association;1997.
16. The Korean Nutrition Society. Dietary reference intakes for Koreans. 1st revision. Seoul: The Korean Nutrition Society;2010.
17. Kim IS, Seo EA, Yu HH. A longitudinal study on the change of nutrients and food consumption with advance in age among middle-aged and the elderly. Korean J Community Nutr. 1999; 4(3):394–402.
18. Kim MH, Lee JC, Bae YJ. The evaluation study on eating behavior and dietary quality of elderly people residing in Samcheok according to age group. Korean J Community Nutr. 2009; 14(5):495–508.
19. Choi KB, Lee YS. Clinical significance of albumin slope in the hemodialysis patients. Korean J Nephrol. 2003; 22(6):713–721.
20. Cho JH. The study on nutritional status in Korean hemodialysis patients [dissertation]. Seoul: Ewha Womans University;2008.
21. Thunberg BJ, Swamy AP, Cestero RV. Cross-sectional and longitudinal nutritional measurements in maintenance hemodialysis patients. Am J Clin Nutr. 1981; 34(10):2005–2012.

22. Ridker PM, Buring JE, Cook NR, Rifai N. C-reactive protein, the metabolic syndrome, and risk of incident cardiovascular events: an 8-year follow-up of 14 719 initially healthy American women. Circulation. 2003; 107(3):391–397.
23. Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO 3rd, Criqui M, Fadl YY, Fortmann SP, Hong Y, Myers GL, Rifai N, Smith SC Jr, Taubert K, Tracy RP, Vinicor F. Centers for Disease Control and Prevention. American Heart Association. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003; 107(3):499–511.
24. Lee HT, Cho S, Lee SH, Kim SR, Kim YH, Seo HJ. Influence of routine calorie and protein intake on nutritional status in stable chronic hemodialysis patients: a 18 months follow-up study. Korean J Nephrol. 2002; 21(1):129–136.
25. Ministry of Health and Welfare. Korea Centers for Disease Control and Prevention. Korea National Health and Nutrition Examination Survey (KNHANES V-2). Seoul: Ministry of Health and Welfare;2012.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download