Abstract
Esophagectomy can result in various postoperative nutrition-related complications that may impair the nutritional status of the patient. In our institution, we usually initiate 16-hour continuous jejunostomy feeding using an enteral feeding pump on postoperative day 2 as a routine protocol after esophagectomy. The target calorie intake was achieved in 6-7 days with this protocol, which is longer than that required with other recently reported feeding protocols. Accordingly, early jejunostomy feeding protocol, which starts on postoperative day 1 and continues for 24 hours was attempted. In the present report, we described 3 cases of early 24-hour continuous jejunostomy feeding after esophagectomy. The use of this new protocol reduced the duration required to achieve the target calorie intake as less than 5 days without any enteral feeding-related complications.
Postoperative malnutrition is relatively common in patients who undergo esophagectomy. In cases where preoperative radiotherapy and chemotherapy are administered during esophageal cancer treatment, preoperative dysphagia and weight loss are commonly observed. Since oral diet cannot be initiated for at least 1 week after esophagectomy, the malnutrition can be aggravated by insufficient nutritional support [1]. Early enteral feeding has been advocated in esophagectomy patients as it could reduce postoperative morbidity. Enteral access is usually obtained via jejunostomy tube feeding placed during the surgery [2]. Pump-assisted continuous drip infusions are the preferred method for jejunostomy feeding. Typically, continuous feeding is initiated at 20-50 mL/h and increased as tolerated by 10-25 mL/h every 4 to 24 hours until the target rate is achieved [3]. Continuous feeding enables to maintain the lowest possible hourly feed rate, thereby to meet nutrient requirements while obtaining better gastrointestinal tolerance due to the lower feed rate. Also, better control of glucose levels to continuous carbohydrate input can be achieved [4].
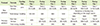
Jejunostomy feeding for patients after esophagectomy is not common in Korea. We established a jejunostomy feeding protocol to provide better nutritional support for esophagectomy patients in our institution 3 years ago. According to that protocol, we treated patients with continuous jejunostomy feeding, using an enteral feeding pump for 16 hours a day, except bedtime to increase their feeding tolerance; it was initiated on postoperative day (POD) 2, considering that no contraindications for jejunostomy were present. The target calorie intake was achieved in 6-7 days with this protocol, which is longer than that required with recently reported feeding protocols [2,5-11]. Therefore, we attempted to initiate early feeding, within 24 hours postoperatively, and continued the feeding for 24 hours per day (Table 1). In the present study, we aimed to reduce the time required to achieve the target calorie intake, without any complications, by using the new protocol.
We report the cases of 3 patients who received continuous 24-hour jejunostomy feeding after esophagectomy. The requirement for informed consent for this case report was waived by the Institutional Review Board of the Seoul National University Hospital.
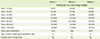
Table 2 shows the patients' surgical data. The mean age of the patients was 61.7 ± 8.9 (range, 56-72) years. All the patients were men who were diagnosed with esophageal cancer. However, the cases differed with regard to the preoperative treatments, operative methods, and postoperative complications. Patient 1 first received neoadjuvant concurrent chemoradiotherapy (CCRT), and thereafter, underwent a hybrid McKeown operation (robot-assisted thoracic esophageal dissection and stomach conduit preparation via laparotomy) and feeding jejunostomy. Since no postoperative complications were observed, other than increased glutamate oxaloacetate transaminase (GOT) and glutamate pyruvate transaminase (GPT) values, oral diet was initiated on POD 7. Patient 2 underwent neoadjuvant CCRT, followed by a McKeown operation (esophagectomy and stomach conduit preparation), excision of a jejunal gastrointestinal stromal tumor, and feeding jejunostomy. Since an oral diet could not be initiated due to postoperative anastomotic leakage, nutritional support was sustained by feeding jejunostomy until POD 48, after which oral nutrition could be initiated. In patient 3, neoadjuvant CCRT was discontinued due to the development of esophagopulmonary fistula, after which the patient was hospitalized and received feeding jejunostomy, followed by antibiotic treatment and nutritional support. After 1 month of supportive treatment, esophagectomy through a left thorcoabdominal incision and en bloc left lower lobectomy were performed. However, no oral feeding was permitted due to the presence of a minor chylothorax and anastomotic leakage after the operation; therefore, jejunostomy feeding was initiated under close observation.
Table 3 illustrates the jejunostomy feeding rates and the postoperative outcomes. In the present cases, we adopted the new protocol with early and 24-hour continuous jejunostomy feeding (Table 1); moreover, early jejunostomy feeding was initiated within 24 hours postoperatively in the patients, who were considered to be fit for feeding. For jejunostomy feeding, we used a fiber-free standard formula and maintained the feeding rate using feeding pumps.
As noted in Table 2, patient 3 had already undergone jejunostomy feeding using the previous protocol, after being hospitalized in a condition wherein an oral diet was not possible. After surgery, the patient underwent early postoperative 24-hour continuous jejunostomy that was initiated on the evening of POD 1 according to the new protocol. The target caloric requirement was achieved in all the subjects within 5 days of the commencement of feeding. None of these patients showed any feeding-associated complications such as diarrhea or abdominal discomfort. The mean duration of hospital stay was 41.0 ± 22.7 (range, 15-57) days and the mean postoperative weight loss was 6.6 ± 5.3 (9.6% ± 7.2%) kg. Moreover, the time taken to achieve the target caloric intake was reduced from 6-7 days to less than 5 days.
The nutritional status of patients who have undergone esophagectomy tends to be poor. Therefore, it is essential to provide proper nutritional support for such patients postoperatively, in order to minimize complications, shorten the recovery period, identify appropriate measures to prevent/modify a poor nutritional state, and ultimately improve the quality of life [1,5]. Table 4 shows the recently reported jejunostomy feeding protocols used in patients in whom initiation of an early oral diet after gastrointestinal surgery was difficult [2,5-11].
The protocols in most of the previous studies aimed to reach the target calorie requirement as quickly as possible, by starting with 10-40 mL/h on the first day after the operation, followed by increases every 6-8 hours during 20-24 hours of continuous feeding. Haverkort et al. [5] reported that 24% of their patients failed to reach a target caloric requirement 12 months after esophagectomy. A total of 48% of patients continued tube feeding and reached their target calorie and protein requirements after hospital discharge. At 6 months postoperatively, only 2 patients still received night tube feeding, and at 12 months postoperatively, only 1 patient still received night tube feeding. Thus, the patients received continuous tube feeding until the target caloric requirement was achieved.
As reported by Gerritsen et al. [6], European nutritional guidelines recommend the use of enteral feeding involving jejunostomy or nasojejunal feeding after pancreaticoduodenectomy. Han-Geurts et al. [2] examined the benefits of feeding and the associated complications, with the aim of providing early nutritional support using jejunostomy feeding and nasoduodenal tube feeding after esophagectomy. Feeding was initiated on POD 1 and helped the patient achieve the target caloric requirement within 3 days; moreover, catheter-related complications had an incidence of 30-35%.
Although our previous protocol invoving 16-hour continuous feeding through jejunostomy until oral feeding was found to be a good method for nutritional support, it had limitations due to later stage initiation and it took longer to achieve the target caloric intake, as compared to protocols reported in other recent studies wherein early feeding was started on POD 1 and the patient's caloric target was reached within 3 days. Accordingly, we attempted to initiate 24-hour continuous feeding on POD 1, which successfully reduced the time required to achieve the target caloric requirement from 6-7 days to less than 5 dyas.
Although the clinical conditions and surgical outcomes of the 3 patients were highly varied and the cases were difficult to manage, all the patients successfully adapted to 24-hour jejunostomy feeding without any complications. Night jejunostomy feeding is advantageous in that it can reduce abdominal fullness caused by combined feeding through per os and jejunostomy. If a patient can adapt to night jejunostomy feeding, he or she can continue oral feeding in daytime and jejunostomy feeding at night. This strategy would help to increase the total calorie intake and improve the nutritional status of patients who require additional jejunostomy feeding. Moreover, we believe that this new approach is useful for increasing the patients' total nutritional intake and expediting their recovery.
In conclusion, we noted that the protocol of early and 24-hour continuous jejunostomy feeding could be safely applied for enhancing nutritional support after esophagectomy. However, further studies on the efficacy and advantages of this novel protocol in patients who received esophagectomy are necessary.
Figures and Tables
Table 1
Comparison of the previous and new jejunostomy feeding protocols for esophagectomy patients in Seoul National University Hospital
References
1. Kight CE. Nutrition considerations in esophagetomy patients. Nutr Clin Pract. 2008; 23:521–528.
2. Han-Geurts IJ, Hop WC, Verhoef C, Tran KT, Tilanus HW. Randomized clinical trial comparing feeding jejunostomy with nasoduodenal tube placement in patients undergoing oesophagectomy. Br J Surg. 2007; 94:31–35.

3. Mueller CM, Kovacevich DS, McClave SA, Miller SJ, Schwartz DB. The A.S.P.E.N adult nutrition support core curriculum. 2nd ed. Silver Spring (MD): American Society for Parenteral and Enteral Nutrition;2012.
4. Bankhead R, Boullata J, Brantly S, Corkins M, Guenter P, Krenitsky J, Lyman B, Metheny NA, Mueller C, Robbins S, Wessel J. The A.S.P.E.N. Enteral nutrition practice recommendations. JPEN J Parenter Enteral Nutr. 2009; 33:122–167.
5. Haverkort EB, Binnekade JM, de Haan RJ, Busch OR, van Berge Henegouwen MI, Gouma DJ. Suboptimal intake of nutrients after esophagectomy with gastric tube reconstruction. J Acad Nutr Diet. 2012; 112:1080–1087.

6. Gerritsen A, Besselink MG, Cieslak KP, Vriens MR, Steenhagen E, van Hillegersberg R, Borel Rinkes IH, Molenaar IQ. Efficacy and complications of nasojejunal, jejunostomy and parenteral feeding after pancreaticoduodenectomy. J Gastrointest Surg. 2012; 16:1144–1151.

7. Ryan AM, Rowley SP, Healy LA, Flood PM, Ravi N, Reynolds JV. Postoesophagectomy early enteral nutrition via a needle catheter jejunostomy: 8-year experience at a specialist unit. Clin Nutr. 2006; 25:386–393.

8. Sica GS, Sujendran V, Wheeler J, Soin B, Maynard N. Needle catheter jejunostomy at esophagectomy for cancer. J Surg Oncol. 2005; 91:276–279.

9. Gabor S, Renner H, Matzi V, Ratzenhofer B, Lindenmann J, Sankin O, Pinter H, Maier A, Smolle J, Smolle-Jüttner FM. Early enteral feeding compared with parenteral nutrition after oesophageal or oesophagogastric resection and reconstruction. Br J Nutr. 2005; 93:509–513.

10. Nabi MS, Bilal A, Shah SA, Ahmad Z. Use of a feeding jejunostomy after esophageal surgery. J Postgrad Med Inst. 2001; 15:29–32.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download