Abstract
BACKGROUND/OBJECTIVES
The prevalence of food allergies in Korean children aged 6 to 12 years increased from 10.9% in 1995 to 12.6% in 2012 according to nationwide population studies. Treatment for food allergies is avoidance of allergenic-related foods and epinephrine auto-injector (EPI) for accidental allergic reactions. This study compared knowledge and perception of food allergy labeling and dietary practices of students.
SUBJECTS/METHODS
The study was conducted with the fourth to sixth grade students from an elementary school in Yongin. A total of 437 response rate (95%) questionnaires were collected and statistically analyzed.
RESULTS
The prevalence of food allergy among respondents was 19.7%, and the most common food allergy-related symptoms were urticaria, followed by itching, vomiting and nausea. Food allergens, other than 12 statutory food allergens, included cheese, cucumber, kiwi, melon, clam, green tea, walnut, grape, apricot and pineapple. Children with and without food allergy experience had a similar level of knowledge on food allergies. Children with food allergy experience thought that food allergy-related labeling on school menus was not clear or informative.
Food allergy is an adverse immune response reaction to food and estimated to affect nearly 3-8% of children in America [1,2,3]. In Korea, the prevalence of food allergy in children aged 6-12 years was estimated at 10.9% in 1995, 8.9% in 2000 and 12.6% in 2012, according to a survey from the Korean version of International Study of Asthma and Allergy in Childhood (ISAAC) [4,5]. In 2005, a survey of children living in Seoul showed that 11.7% experienced a food-related allergic reaction more than once [6]. Treatment for food allergies is avoidance of allergenicrelated foods and epinephrine auto-injector (EPI) for accidental allergic reactions [7].
Food allergy presents a variety of symptoms on the skin (urticaria, dermatitis, eczema, angioedema, itching) and in the gastrointestinal tract (nausea, vomiting, diarrhea, abdominal cramping) and respiratory tract (rhinitis, asthma, laryngeal edema) [8]. Food-induced anaphylactic shock is the most frightening symptom that is acute in onset, occurring within minutes or hours, and may lead to death if prompt treatment is not administered [9]. Major food allergens among children are eggs, cow's milk, fish and other seafood, while peanuts, tree nuts, fish and crustaceans (shrimp, crab, lobster) are common among adults [8,10].
A survey of 993 children aged 18 and younger who visited 7 hospitals in the Seoul and Gyeonggi area showed that eggs, cow's milk and dairy products, peach, shrimp, pork, peanuts and tree nuts were common allergenic foods [11]. Lee et al. [5] studied the prevalence of food allergies and perception of food allergen labeling in school foodservice for 27,679 students at 1,000 elementary, middle and high schools in Korea. Approximately 12.6% of students showed food-related allergies, and 6.8% of respondents had been diagnosed with food allergies by a doctor. Cow's milk, peach and crab were the most common allergy-related foods among first and fifth graders.
A series of nationwide cross-sectional questionnaire surveys of Korean children in 1995, 2000 and 2010 showed that the prevalence of food allergies in children has increased [4,5]. The Ministry of Education implemented a mandatory 'school lunch food allergen labeling system' in 2012 that requires disclosure of allergenic food ingredients in school meals and developed 'the manual for school lunch food allergen labeling' [12,13]. In the United States, food allergy guidelines have been published by the American Academy of Allergy, Asthma, and Immunology and the American Academy of Pediatrics [14,15,16]. School management guidelines for food allergies detail preventive measures, such as a food allergen avoidance diet, substitution diet, food allergy education that includes avoidance of food sharing and cross-contact, and epinephrine for acute food reactions [17]. Based on guidelines and preventive measures, the role of parents, dietitians and teachers is important in the care and protection of children with food allergies [17]. Further, the education and management of young students with food allergies is important because mostly spend time at school [18] and lack awareness of food allergies and the ability to handle them [19].
Previous studies reported on the prevalence of food allergies and causative foods. However, little has been done to identify differences in perception level of food allergy labeling and knowledge of food allergies and dietary practices among groups with and without food allergy experience. The aims of this study were to investigate food allergens and symptoms of food allergy, and to examine knowledge of food allergies, recognition of food allergy labeling, and good dietary practices by elementary school children in fourth, fifth and sixth grade with and without food allergies.
Fourth, fifth and sixth grade students at an elementary school in Yongin, Gyeonggi Province voluntarily participated in the survey from 20 November 2012 to 10 April 2013, with the cooperation of school nutrition teachers. Upper grade students were selected to ensure a higher confidence level of data. A total of 437 of 460 distributed questionnaires were collected and used for statistical analysis. The survey was conducted by the guidelines of the institutional review board of Dankook University (DKU 2014-06-003), Yongin, Korea.
A 4-page survey was used for data collection. It consisted of 26 questions in four sections: Demographic variables (4 items), knowledge of food allergy-related variables (10 items), perceptions of labeling for the allergy-induced foods (4 items), and practices for a healthy dietary life (8 items).
In the section on demographic variables, students were asked about grade level, gender, height and weight, and experience with food allergies. Those who experienced food allergy symptoms were requested to list causative foods.
In the section on knowledge of food allergies, questions were based on the "Food Allergy Training and Foodservice Management Manual", as recommended by the Food Safety Enforcement Team in Seoul [20] and cited by previous studies [5,18,21,22,23]. Ten questions covered: definition of food allergy, substance causing food allergies, diseases similar to a food allergy, nutrition responding to food allergy, reminders of allergic disorders when consuming food allergic sources, a disease name that indicates a serious allergic symptom, types of food provoking allergy after consumption of wheat, foods to avoid in preventing a tomato allergy, substitute food item to prevent a milk allergy, and problems caused by restriction of allergy provoking foods during growth and development.
In the section on perception of food allergy labeling, students were surveyed to understand how well they recognize food allergy information on a school menu designed after the labeling law took effect in 2013 [5,13]. Four levels of agreement were offered: 'Easy to understand for students', 'satisfied with information', 'information is necessary' and 'easy to figure out' were asked [18,21,23,24].
In the section on healthy dietary life practices, eight questions were based on revised dietary guidelines for children published by the Ministry of Health and Welfare [25] and covered: unbalanced diets, eating a variety of vegetables, eating a moderate quantity of protein, drinking two cups of milk, physical activities, eating breakfast, choice of healthy snacks, and eating less salt, sugar or greasy foods.
Students were asked to select all that apply in the first section, choose the best answer in the second section, responded according to a 5-point Likert scale (1: strongly disagree to 5: strongly agree) in the third and fourth sections.
Data were analyzed with the SPSS 18.0 statistical package (SPSS Inc., Chicago, IL). Descriptive statistics were examined for frequencies and percentages of variables on demographic characteristics of respondents, food allergy symptoms experienced, and source of food allergies. Mean and standard deviation were calculated for food allergy-related knowledge, perception of allergy-related food labeling on school foodservice menus, and healthy dietary life practices of respondents. A t-test was used to compare the means of knowledge on food allergy, perception of food allergy labeling and healthy dietary life practices between the two groups by experience with food allergy. Level of significance was set at α = 0.05. Cronbach's α was used to examine reliability of questions on food allergy knowledge (10 items), perception of food allergy labeling (4 items), and healthy dietary life practices (8 items). Values were 0.618, 0.880, and 0.824, respectively, indicating higher reliability as all were above 0.6.
Respondents with food allergy experience comprised 28 persons (21.7%) in fourth grade, 36 students (23.7%) in fifth grade and 22 students (14.1%) in sixth grade (Table 1). When comparing gender, girls (46 persons, 20.7%) experienced food allergies more often than boys (40 persons, 18.6%). But there are no statistically significant difference by grades and gender. The prevalence rate of food allergies was 19.7%, based on 86 students who experienced a food allergy in the total elementary school sample.
Allergy symptoms experienced by 86 respondents are presented in Table 2. Urticaria (26.7%) was the most frequent symptom reported by students, followed by itching (22.1%), vomiting (11.6%), other symptoms (8.1%), nausea (4.7%), diarrhea (3.5%), stomachache (2.3%) and dyspnoea (1.2%).
In the 'other symptoms' of food allergies, 3 of 7 persons listed atopy dermatitis and other responses included sore throat, itching of tongue and cough. Some 19.8% of respondents have suffered two or more food allergic symptoms. The most common symptom was itching for boys (27.5%) and urticaria (34.8%) for girls.
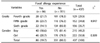
Foods most frequently causing allergy for elementary school students, as designated by the Ministry of Education in Korea, are milk and shrimp (7%), eggs and mackerel (5.8%), peanuts and tomato (3.5%), wheat and crab (2.3%), and pork meat, peach and soybean (1.2%) (Table 3). Further, respondents reported allergies to cheese (7.7%), cucumber (7.7%), kiwi (3.1%), melon (3.1%) and clams (3.1%), even though these foods are not designated as allergy foods by the Ministry of Education. Fruit (grape, apricot and pineapple), green tea, ice cream, cookies, fishcake, walnuts and mitre squid were also mentioned as the source of food allergies.
On knowledge of food allergies according to the food allergy experience in real-life (Table 4), students who experienced a food allergy scored 57.6 of 100 points and students who did not scored 61.1 of 100 points. However, there was no significant difference between the groups. Students with food allergy experience had more knowledge about 'the disease name of anaphylaxis' (30.9 vs. 30.2) and 'alternative foods for preventing milk allergy' (63.8 vs. 61.8) compared to those without allergy experience. However, results did not show statistically significant differences. The only item showing a statistically significant difference was the 'not true' items as problems caused by restriction of allergy provoking foods during growth and development. The food allergy no-experience group (49.9%) scored higher than the food allergy experience group (37.1%).
Among total respondents, the average correct answer rate was approximately 60.4 points out of 100 points. The question on 'diseases similar to a food allergy' had the highest number of correct answers (83.3%). A majority of students knew the definition of food allergy (77.1%), foods restricted for people with a tomato allergy (76.2%), and foods restricted for people with a wheat allergy (74.4%). Data, not shown in Table, revealed that upper grade students have a moderate level of knowledge on allergy-provoking foods (64.5%), and milk-allergic foods (62.5%).
The lowest correct answer rate (24.7%) was in response to a question on the nutrient of protein that responds to food allergies, indicating that students know little about the causative material provoking food allergies. The question on the most serious symptom of food allergic disorders indicated the second lowest score (30.2%), indicating that not much is known about anaphylaxis. Restriction of allergy-provoking foods may be attributed a deficiency of specific nutrients for adolescent growth, as only 47.4% of students understand the importance. More education should be provided to students on anaphylaxis, food allergy mechanisms and alternative foods for those on allergy-restricted diets.
Students with food allergy experience showed a lower level of perception regarding food allergy labeling (3.08 points) than those without experience (3.29 points). However, there was no statistically significant difference (P < 0.05) (Table 5).
There were statistically significant differences on two items: 'satisfied with allergen food information on school menu' and 'easy to figure out food allergy information on menu'. The experienced group scored fewer points (3.02 and 2.83 points) than the inexperienced group (3.31 and 3.18 points).
On healthy dietary practices, students performed well on 'eat breakfast every day' (4.19 ± 1.20) but poorly on 'drink two cups of milk every day' (3.59 ± 1.33) (Table 6). The mean of students' dietary practices was 3.81 points, showing a higher than average score.
The experienced food allergy group had an overall score of 3.76 of 5 points for healthy dietary life practices, and the inexperienced group scored 3.82 points. However, there was no significant difference. In comparing content by item, there was a statistically significant difference for "drinking more than two glasses of milk every day" with the non-allergy-experienced students practicing it more often (3.66 points) than allergyexperienced students (3.30 points) (P < 0.05).
This study investigated food allergens and food allergy symptoms of fourth, fifth and sixth grade elementary school students, and examined food allergy-related knowledge and perception of food allergen labeling.
Our results showed that the prevalence of food allergy among respondents was 19.7%, and the most common food allergy-related symptoms were urticaria (26.7%), itching (22.1%), vomiting (11.6%), others (8.1%) and nausea (4.7%). Lee et al. [5] reported a food allergy prevalence of 12.6% (27 of 679) among students in Korea and 6.8% of these had been diagnosed with a food allergy by doctors. Our result (19.7%) was higher than the other study (12.6%) and national surveys (9-11%) [4,5]. This may be explained by the self-administered questionnaire for children, not have diagnosed a doctor. Subjects may have confused food allergy with other adverse reactions such as foodborne disease, lactose intolerance or food additive hypersensitivity.
The mostly common allergenic foods in this study were cow's milk and shrimp (7.0%), eggs and mackerel (5.8%), peanuts and tomato (3.5%), wheat and crab (2.3%) and pork, peach, and soybean (1.2%). Cow's milk, eggs, soy and peanuts are foods known to trigger allergies frequently among children [4], though an allergy to cow's milk or eggs is usually subside after childhood or adolescence [26]. A study on the prevalence and main characteristics of food allergenic school children in France reported that 62 of 182 respondents (25.4%) outgrew food allergies. Children most outgrew a food allergy to cow's milk (55.2%), but never to tree nuts [27]. Peanut and seafood allergies are most common among adults in North America, and a buckwheat allergy is common among adults in Japan and Korea [28,29,30]. The prevalence of food allergy to specific foods may be affected by age, ethnicity and eating habits [4,8].
Our study reported a number of allergenic foods outside the 12 designated by the Ministry of Food and Drug Safety (MFDS) [31], including cheese, cucumber, kiwi, melon, clams, green tea, walnuts, grape, apricot and pineapple. Currently, there are more than 160 allergenic foods worldwide. The 'school lunch food allergen labeling system' has been implemented by the Ministry of Education since 2013, and uses a red color and number from 1-12 for designated food allergens to indicate their presence on foodservice menus [13,32]. A study on management of food allergies in school lunch programs reported that 75% of most frequently served school meals contained more than one food allergen among 890 menu items [33]. Chicken, mushroom, kiwi and clams triggered food allergies, in addition to the 12 most common food allergens. Different varieties of food allergens have been reported [34,35,36], and specific food allergens such as tree nuts can seriously impact Korean children [36,37]. However, food allergens not designated by the MFDS are not managed or disclosed in school lunch programs [18]. Kim et al. [33] found that 84% of 154 participating schools tend to assign complete responsibility to food-allergic children and their caregivers. Therefore, "allergenic food labeling" should be improved, and policy makers from the Ministry of Education need to consider food allergies outside the 12 common food allergens. All allergenic foods should be managed with the same care as any food item can cause an allergic reaction in children.
Healthy dietary life practices between the two groups were not significantly different, except 'drink two cups of milk.' This result may be explained by the need to restrict or avoid allergenic foods or potential food allergens such as milk, fish, eggs and meat among children with food allergies. A study suggested that allergy subjects were prone to lifestyle choices such as more frequent alcohol drinking and smoking than non-allergy subjects. [23] The allergy group had dietary habits of skipping breakfast more often, higher consumption of instant foods and less fruit, and more irregular eating patterns, in addition to more frequent consumption of pork, eggs, walnuts, tuna, kiwi and shellfish than non-allergy counterparts [23].
To the best of our knowledge, prevalence of food allergy in childhood and type of food allergens for a representative sample of Korean children has not yet been investigated. Therefore, longitudinal studies and the establishment of a surveillance monitoring center for food allergy incidents are needed for accurate data on prevalence of food-allergic children and all causative food allergens.
On perception of food allergen labeling on school meals, results showed that respondents viewed it as important but were not satisfied. Data showed that differences between students with and without food allergy experience were rarely significant. However, Lee et al. [5] found that food-allergenic students read labeling more carefully and frequently on school menus than students without food allergies. Lee et al. [11] studied the perception of allergenic food labels among 962 subjects that included 337 food-allergic subjects and 656 non-food allergic subjects. The survey found that 38.3% of food-allergic and 18.6% of non-food allergic subjects understood allergy-related labels and 79.2% of food-allergic and 70.1% of non-food allergic subjects expressed a negative view on the current food allergen labeling system. Reasons for dissatisfaction were too ambiguous, ingredient list too technical, font size too small, and hard to understand food allergen labels. Rhim and McMorris [38] found that only 21% of school staff could read hidden allergens on food labels. Sicherer et al. [39] reported that 55% of peanut-allergic children accidentally ingested them at school due to allergens hidden in food, food-sharing and cross-contact. Food-allergic consumers or those buying for individuals with a food allergy urgently need to read and easily understand food allergy-related labels. Convenient and clear labeling of food allergens and identification of possible crosscontamination with allergenic ingredients is needed to make informed and safe food choices. Adding more food allergens to the list of 12 statutory food allergens requiring mandatory ingredient labeling must also be considered, as management guidelines of food allergen labeling state that the system is provided to help food allergic consumers.
On food allergy-related knowledge, children knew the definition of food allergy, food allergens, and the difference between a food allergy and foodborne disease, but were not informed about mechanisms of food allergies or anaphylaxis. For prevention and treatment of food-allergic incidents among children, schools need to provide education on food allergy, preventive measures and treatment guidelines. In America, most schools provide special meals on request and food substitution for foodallergy students [38]. Food allergy education should contain easily understood contents and a class teaching real-life skills, such as how to read a food label or shop for safe ingredients. A comprehensive educational program with the cooperation of parents, school teachers and dietitians for food allergic children can prevent and manage serious consequences of food-allergic reactions in children.
The study had limitations. First, the study was a case study with the upper grade students at an elementary school, which must be considered when generalizing the results. Second, knowledge of food allergies did not show a significant difference between students with and without food allergy experience, except one question. Therefore, future study is needed to identify the association between food allergy and the learning capacity of students. Third, the prevalence of food allergy among students was totally dependent on the self-evaluation of respondents. Students with food allergy symptoms were not asked if a doctor diagnosed a food allergy, which may explain our data showing a somewhat higher prevalence rate than other studies. A future study should include a survey question on diagnosis of food allergies by a doctor.
This study suggested meaningful outcomes in that additional allergenic foods should be designated to ensure safe food-service and school administrators should advocate for a better allergy labeling system to inform and protect students. Future studies can use information about prevalence and types of food allergy among Korean children to develop effective educational programs and implement preventive measures on food-related allergies.
Figures and Tables
References
2. Gupta RS, Springston EE, Warrier MR, Smith B, Kumar R, Pongracic J, Holl JL. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics. 2011; 128:e9–e17.

3. Goossens NJ, Flokstra-de Blok BM, van der Meulen GN, Botjes E, Burgerhof HG, Gupta RS, Springston EE, Smith B, Duiverman EJ, Dubois AE. Food allergy knowledge of parents - is ignorance bliss? Pediatr Allergy Immunol. 2013; 24:567–573.

4. Lee SY. IgE mediated food allergy in Korean children: focused on plant food allergy. Asia Pac Allergy. 2013; 3:15–22.

5. Lee AH, Kim KE, Lee KE, Kim SH, Wang TW, Kim KW, Kwak TK. Prevalence of food allergy and perceptions on food allergen labeling in school foodservice among Korean students. Allergy Asthma Respir Dis. 2013; 1:227–234.

6. Park JY, Park GY, Han YS, Shin MY. Survey of food allergy in elementary school children in Bucheon-city and relationship between food allergy and other allergic diseases. Allergy Asthma Respir Dis. 2013; 1:266–273.

7. Gupta RS, Springston EE, Kim JS, Smith B, Pongracic JA, Wang X, Holl J. Food allergy knowledge, attitudes, and beliefs of primary care physicians. Pediatrics. 2010; 125:126–132.

8. Taylor SL, Hefle SL. Food allergies and other food sensitivities. Food Technol. 2001; 55:68–83.
9. Sampson HA, Muñoz-Furlong A, Campbell RL, Adkinson NF Jr, Bock SA, Branum A, Brown SG, Camargo CA Jr, Cydulka R, Galli SJ, Gidudu J, Gruchalla RS, Harlor AD Jr, Hepner DL, Lewis LM, Lieberman PL, Metcalfe DD, O'Connor R, Muraro A, Rudman A, Schmitt C, Scherrer D, Simons FE, Thomas S, Wood JP, Decker WW. Second symposium on the definition and management of anaphylaxis: summary report--second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. Ann Emerg Med. 2006; 47:373–380.

10. Ahn K. Food allergy: diagnosis and management. Korean J Asthma Allergy Clin Immunol. 2011; 31:163–169.
11. Lee SY, Kim KW, Ahn K, Kim HH, Pyun BY, Park YM, Kim KE. Consumers use and satisfaction of allergic food labels. Pediatr Allergy Respir Dis. 2011; 21:294–301.

12. Han YS, Jang EY, Yoon J, Jung JI, Go SH, Lee HY. Food allergymanual for education and school meal management. Seoul: Seoul Metropolitan Government Food Safety Task Force Team;2010.
13. Ministry of Education. Law for School Feeding No. 3 Stat. 16 Mandatory notice of foods containing allergenic ingredients in school meals. 2013. 05. 22.
14. The treatment in school of children who have food allergies. Committee report from the Adverse Reactions to Food Committee of the American Academy of Allergy and Immunology. J Allergy Clin Immunol. 1991; 87:749–751.
15. Anaphylaxis in schools and other childcare settings. AAAAI Board of Directors. American Academy of Allergy, Asthma and Immunology. J Allergy Clin Immunol. 1998; 102:173–176.
16. American Academy of Pediatrics Committee on School Health: Guidelines for urgent care in schoo. Pediatrics. 1990; 86:999–1000.
17. Young MC, Muñoz-Furlong A, Sicherer SH. Management of food allergies in schools: a perspective for allergists. J Allergy Clin Immunol. 2009; 124:175–182. 182.e1–182.e4.

18. Park EJ. Study on level of perception and execution about food allergy in Seoul district school meal services [MS Thesis]. Seoul: Kyunghee University;2012.
19. Kim S, Yoon J, Kwon S, Kim J, Han Y. Current status of managing food allergies in schools in Seoul, Korea. J Child Health Care. 2012; 16:406–416.

20. Seoul Metropolitan Government Food Safety Task Force Team. Food allergy training and foodservice management manual. Seoul: Seoul Metropolitan Government Food Safety Task Force Team;2010.
21. Kim YJ. Comparison of the perception for food allergy between nutrition teachers and children in elementary and middle school [MS Thesis]. Seoul: Jungang University;2010.
22. Yoon HS. Immediate type reaction of food allergy. Allergy Asthma Respir Dis. 1992; 12:5–12.
23. Yang SH, Kim EJ, Kim YN, Seong KS, Kim SS, Han CK, Lee BH. Comparison of eating habits and dietary intake patterns between people with and without allergy. Korean J Nutr. 2009; 42:523–535.

24. Han JS, Hong SO, Kim JS, Han JP, Kim NS. Frequency of food allergy in Korea and the causative food allergens. J Korean Soc Food Sci Nutr. 1997; 26:1–9.
25. Kim MH. A study of change food-intake elementary school children with atopic dermatitis [MS Thesis]. Seoul: Kyunghee University;2007.
26. Skypala I. Adverse food reactions--an emerging issue for adults. J Am Diet Assoc. 2011; 111:1877–1891.

27. Rancé F, Grandmottet X, Grandjean H. Prevalence and main characteristics of schoolchildren diagnosed with food allergies in France. Clin Exp Allergy. 2005; 35:167–172.

28. Taylor SL, Hefle SL, Munoz-Furlong A. Food allergies and avoidance diets. Nutr Today. 1999; 34:15–22.

29. Lehrer SB, Helbling A, Daul CB. Seafood allergy: prevalence and treatment. J Food Saf. 1992; 13:61–76.

30. Kang SY, Min KU. Three cases of buckwheat allergy. J Korean Med Assoc. 1984; 27:765–768.
31. Ministry of Food and Drug Safety. Notification No. 2010-97. Food labeling regulation. 2013. 12. 30.
32. Ministry of Education. The manual of school lunch food allergen labeling. Seoul: Ministry of Education;2012.
33. Kim YM, Heo YR, Ro HK. Perception and practices regarding food allergy of elementary and middle school nutritionists in the Jeonnam area. J Korean Soc Food Sci Nutr. 2014; 43:151–161.

34. Oh JW, Pyun BY, Choung JT, Ahn KM, Kim CH, Song SW, Son JA, Lee SY, Lee SI. Epidemiological change of atopic dermatitis and food allergy in school-aged children in Korea between 1995 and 2000. J Korean Med Sci. 2004; 19:716–723.

35. Son DY, Yoon KR, Lee SI. Study of the most common allergic foods in Korea. Korean J Food Sci Technol. 2002; 34:885–888.
36. Seo WH, Jang EY, Han YS, Ahn KM, Jung JT. Management of food allergies in young children at a Child Care Center and Hospital in Korean. Pediatr Allergy Respir Dis. 2011; 21:32–38.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download