Abstract
BACKGROUND/OBJECTIVES
The immigrant population has grown considerably in South Korea since the early 1990s due to international marriages. Dietary changes in immigrants are an important issue, because they are related to health and disease patterns. This study was conducted to compare changes in dietary intake between baseline and follow-up periods.
SUBJECTS/METHODS
Two hundreds thirty three Vietnamese female married immigrants. Baseline data were collected during 2006-2009, and the follow-up data were collected during 2008 and 2010. Food consumption was assessed using a 1-day 24-hour recall.
RESULTS
The amount of the total food consumed (P < 0.001) including that of cereals (P = 0.004), vegetables (P = 0.003), and fruits (P = 0.002) decreased at follow-up compared to that at baseline, whereas consumption of milk and dairy products increased (P = 0.004). Accordingly, the overall energy and nutrient intake decreased at follow-up, including carbohydrates (P = 0.012), protein (P = 0.021), fiber (P = 0.008), iron (P = 0.009), zinc (P = 0.006), and folate (P = 0.002). Among various anthropometric and biochemical variables, mean skeletal muscle mass decreased (P = 0.012), plasma high density lipoprotein-cholesterol increased, (P = 0.020) and high sensitivity C-reactive protein decreased at follow-up (P < 0.001).
The immigrant population through international marriage has grown considerably in South Korea since the early 1990s, and the international marriage rate for all marriages was as high as 10.5% in South Korea in 2010. The number of foreign women marrying Korean men has increased by nearly four times, from 6,945 immigrants to 26,274 between 2000 and 2010 [1]. Of these, Vietnamese women represent the highest proportion [2].
Immigrants are in the process of acculturation and must cope with a language barrier, economic problems [3,4,5,6], discrimination, and cultural differences, including social habits and dietary changes to adapt to the new environment [7,8,9,10]. In particular, dietary changes are an important issue, because they are related to health and disease status [11,12,13,14,15]. Unlike other types of immigrants, women who immigrate through marriage are predominantly responsible for preparing meals for the entire family. However, they lack access to nutritionally adequate and culturally acceptable foods, in part, because they have not yet become accustomed to Korean food and have limited access to Vietnamese food [16,17,18,19,20,21]. Choi et al. [16] found that almost 50% of Vietnamese female marriage immigrants experience food insecurity because of factors such as economic problems and the lack of appetizing food. In addition to food insecurity, nutrient intake in Vietnamese female marriage immigrants is inadequate [22,23,24] compared to recommended dietary allowances for Vietnamese [25] and the Dietary References Intake for Koreans [26]. A previous study showed an association between nutritional status and length of residence in Korea in a cross-sectional study, but no significant differences based on the length of residence in Korea were observed for nutritional status except vitamin C [22]. Because it is difficult to identify the causal relationships between nutrient intake and the length of residence in a cross-sectional study, a follow-up study is needed to investigate dietary changes over time. However, no studies have been conducted on nutritional status changes between baseline and follow-up in Vietnamese female marriage immigrants. The purpose of this study was to investigate baseline and follow-up changes in dietary intake in Vietnamese female marriage immigrants.
The participants were Vietnamese female marriage immigrants who voluntarily participated in the Cohort of Intermarried Women in Korea. The Cohort of Intermarried Women in Korea is an ongoing, prospective, epidemiological study as part of the Korean Genome and Epidemiology Study (KoGES) established in November 2006 [22,23,24]. Baseline data were collected during 2006-2009, and follow-up data were collected in 2008 and 2010. A total of 274 subjects participated during both periods (baseline and follow-up) from clinical centers in Seoul, Busan, Daegu, Danyang, Gimhea, Gwangju, Gyeongju, Gongju, Jinju, Sangju, Masan, Okcheon, and Pohang. Among the 274 subjects, those with missing dietary intake (n = 37), energy consumption < 400 kcal (n=1) or > 3,500 kcal (n=1), and those who were pregnant (n = 1) or used chronic disease medications (n = 1) were excluded. Therefore, 233 immigrants were finally eligible for this study.
Subjects were individually interviewed by trained personnel using standard protocols at baseline and follow-up. Vietnamese translators helped in the process whenever needed. The study instrument used was the KoGES questionnaire, which included age, current alcohol consumption, exercise, education, and income. Alcohol drinking was classified into current and non-drinkers. A regular exerciser was defined as a person who performed exercise currently and regularly enough to induce sweating. Educational status was categorized as ≤ elementary school, middle school, and ≥ high school. Household monthly income was classified as < 1,000, 1,000-1,500, and > 1,500 thousand Korean Won.
Dietary changes after immigration are inevitable because it is difficult for Vietnamese female marriage immigrants to obtain some foods that they had before immigration because of their relatively higher price (pork, fish, and rice noodles), limited access to markets (rice noodles), and unavailability of Vietnamese food in Korea (vegetables such as swamp cabbage and yam and fruits such as papaya, longan, and guava). In contrast, dairy products are relatively less expensive in Korea [24]. A Mini Dietary Assessment (MDA) was used at baseline and follow-up to evaluate diet quality and was validated previously [27]. Ten questions were asked regarding meal regularity, diet diversity, intake frequency of each food group, intake frequency of snacks, and preference for salty taste. For each question, 5, 3, or 1 points were given for answers of "always", "generally", or "seldom", respectively. However, 1, 3, or 5 points were given to answers of "always", "generally", and "seldom", respectively, for questions on frequency of eating snacks and high-fat foods as well as on preference for salty taste. The total MDA score was 50. A higher MDA score indicates higher diet quality.
Food consumption was assessed using a 1-day, 24-hour recall by a trained dietitian. Food models were used to estimate portion size. Energy and nutrient intake data were analyzed using the Computer Aided Nutritional Analysis program version 3.0 software (CAN-Pro 3.0, Nutritional Assessment Program, 2006, The Korean Nutrition Society, Seoul, Korea) [28]. Energy and nutrient intake data were compared with the estimated energy requirements (EER) and estimated average requirements of the Korea Dietary Reference Intakes for women in the subject's age range [26].
Anthropometric variables and blood pressures were obtained by trained nurses or medical personnel during both periods. Standing height and body weight were measured using an automatic height/weight measuring instrument (Dong Sahn Jenix Co., Seoul, Korea). Body mass index was calculated as kg/m2. Waist and hip circumferences were measured with a tape measure (anthropometric tape; Preston 5193, Seoul, Korea). Body composition was assessed with the Inbody 230 (Biospace Co., Seoul, Korea). These measurements were taken once. Systolic and diastolic blood pressures were measured using the FT0500R automatic blood pressure calculator (Jawon Medical, Gyeongsan, Korea) and read by attending medical doctors after a 10-minute rest in the sitting position; the average of two measurements was used.
Blood samples were drawn by medical technologists after an 8-hour overnight fast, collected in EDTA-containing tubes, and centrifuged at 3,500 rpm for 10 minutes at 4℃. The plasma samples were stored at -70℃ until analysis. Serum albumin and protein, hemoglobin, and hematocrit were measured using an autoanalyzer (ADVIA 120, Bayer Diagnostics, Tarrytown, NY, USA). Fasting blood sugar level, total cholesterol, high density lipoprotein (HDL)-cholesterol, and triglycerides were also measured with an autoanalyzer (ADVIA 1550, Bayer Diagnostics). Low density lipoprotein (LDL)-cholesterol was calculated as total cholesterol-HDL-cholesterol-(triglycerides/5) [29]. Serum high sensitivity C-reactive protein (hs-CRP) was measured with an ADVIA 1650 using a hs-CRP-Latex (II) X2 kit (Seiken Laboratories Ltd., Tokyo, Japan).
Data are expressed as means and standard deviations (continuous) or as frequencies and percentages (categorical). Categorical variables were evaluated using the chi-square or Fisher's exact tests to investigate differences between groups. The paired t-test was used to compare general characteristics, anthropometric parameters, daily nutrient and food intakes, MDA scores, and blood profiles between the baseline and follow-up periods. All analyses were performed using SAS 9.2 software (SAS Institute, Cary, NC, USA). All reported probability tests were two-sided, and differences were considered significant at the 5% level.
The cohort observation period of the 233 Vietnamese subjects was 11-41 months, with a mean follow-up of 28.1 ± 7.8 months (Table 1). The mean age was 23.0 ± 3.8 years at baseline. Nearly 40% of subjects had graduated from elementary school. Mean height and weight were 154.7 ± 4.9 cm and 50.5 ± 7.3 kg at baseline and 154.9 ± 4.9 cm and 50.9 ± 7.5 kg, respectively.
Daily food intake of Vietnamese subjects is described in Table 2. Overall food intake decreased from baseline to follow-up. The consumption of cereal and cereal products (P = 0.004), vegetables (P = 0.003), fruits (P = 0.002), and fishes (P = 0.030) decreased significantly, whereas consumption of mushrooms (P = 0.030), milk and dairy products (P = 0.004) increased significantly. Total food intakes were 1,070.0 ± 496.4 g/d and 912.0 ± 371.9 g/d at baseline and follow-up, respectively, and decreased significantly by the follow-up period.
Daily nutrient intakes of Vietnamese subjects are presented in Table 3. Overall nutrient intake decreased over time. The intakes of total energy (P = 0.028), carbohydrates (P = 0.012), protein (P = 0.021), fiber (P = 0.008), iron (P = 0.009), phosphorus (P = 0.044), zinc (P = 0.006), vitamin B6 (P = 0.027), and folate (P = 0.002) decreased significantly over time. Most of the Vietnamese subjects (80.7%) had energy intake below the EER at both the baseline and follow-up, whereas only 5.6% of subjects had improved energy intake from baseline to follow-up (P = 0.023).
The MDA scores changed between baseline and follow-up. Milk and dairy product consumption increased in 27.5% of Vietnamese subjects, whereas it decreased in 25.3% of subjects (P = 0.039). Fried or stir-fried food consumption decreased in 27.9% of subjects but increased in 23.2% of subjects (P = 0.032) (Table 4).
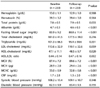
The blood profiles and blood pressure of Vietnamese subjects are shown Table 5. Total protein (P = 0.033), fasting blood sugar (P < 0.001), HDL-cholesterol (P = 0.020), HDL/LDL ratio (P = 0.002), mean corpuscular volume (P < 0.001), and mean corpuscular hemoglobin (P < 0.001) increased, whereas albumin (P < 0.001), mean corpuscular hemoglobin concentration, and hs-CRP (P < 0.001) decreased during the follow-up period.
This study is the first prospective report of the KoGES study. Our results suggest that dietary intake of Vietnamese marriage immigrants changed from baseline to follow-up. Consumption of cereal, vegetables, fruits, and total food decreased over time, whereas consumption of milk and dairy products increased. Many studies have reported that dietary patterns in immigrants change through acculturation. Regev-Tobias et al. [30] showed that intake of fruits, vegetables, and dairy products is negligible, whereas simple sugar consumption is high in Ethiopian women living in Israel. Rosenmöller et al. [31] reported that > 50% of Chinese immigrants increase their consumption of healthy foods such as fruits, and vegetables, white meats, and dairy products and decrease consumption of deep-fried, high fat foods, and soft drinks after immigrating to Canada [31]. Several studies have reported an association between acculturation and healthy dietary habits in immigrants [32]. Mexican immigrants to the United States change their diet over time, and an increase in fat intake and decrease in consumption of fruits and vegetables are observed with an increase in the duration of residency and greater acculturation [33].
However, food consumption of subjects is not sufficient. According to the 2009 Korea Health and Nutrition Examination Survey IV [34], total food intake by Korean women aged 19-29 years was 1,304.4 g/d, whereas total food intake of Vietnamese subjects was less than that of Korean women of the same age, at both baseline (1,070.0 g/d) and at follow-up (912.0 g/d). Furthermore, milk and dairy product consumption was lower in Vietnamese subjects (75.0 g/d at follow-up) than that in Korean women (119.2 g/d), although milk and dairy product consumption increased significantly from baseline to follow-up. Similarly, overall nutrient intake, including energy, carbohydrates, protein, fiber, iron, zinc, and folate decreased over time and a high proportion of subjects had energy intake below the EER at both the baseline and follow-up. Although a previous cross-sectional study using KoGES data reported that nutrient intake in Vietnamese female marriage immigrants does not differ by the length of residence in Korea [22], the cross-sectional nature of that study limited conclusions on cause-and-effect without regard to duration.
Changes in dietary behavior may be related to health condition of international immigrants. In a study of first-generation Korean-Americans, dietary changes were associated with length of residence in the United States and frequency of chronic diseases [15]. Tunisian immigrants who maintain their traditional diet have a lower risk of disease compared with natives living in France [35]. Japanese-Americans who retain a more traditional Japanese diet show reduced prevalence of diabetes in Hawaii [36]. Judging from the hematological data, our subjects were in fair condition. Interestingly, no changes in total cholesterol, triglycerides, or LDL-cholesterol but increased levels of HDL-cholesterol and the HDL/LDL ratio were found in our subjects, which was contrary to findings from immigrants to Western countries [37,38]. Further studies are needed to investigate why increased levels of HDL-cholesterol have occurred in our subjects despite decreased protein intake and no changes in fat intake. In addition, blood hs-CRP levels decreased from baseline to follow-up. hs-CRP, a biomarker of subclinical inflammation, is produced by the liver in response to various inflammatory conditions and is a predictor of cardiovascular disease risk [39,40,41]. These results can be explained by changes in milk and dairy food consumption, which were observed clearly in our study. The reduced fiber intake, partly due to decreased consumption of fruit and vegetable, may be attributable to increased blood glucose levels in our study subjects, as shown in other South Asian immigrant studies in Europe [42].
Several studies have found a negative association between the intake of milk or dairy products, rich sources of calcium, and risk factors for cardiovascular diseases including lipid metabolism [43,44] and blood hs-CRP levels [45,46]. Several mechanisms have been proposed for how calcium benefits lipid profiles. Calcium can be bound to fatty acids and bile acids in the gut by bile salt hydrolase; thus, interfering with lipid absorption [47,48]. In addition to these intestinal effects, an HDL-cholesterol-increasing effect of calcium via a reduction in plasma cholesteryl ester transport protein (CETP) has also been suggested [49]. Enhancing calcium intake via milk consumption could increase serum HDL-cholesterol by decreasing CETP activity. Dietary calcium may also suppress circulating 1-alpha, 25-dihydroxycholecalciferol, which inhibits inflammatory stress [45,46].
This study had some limitations. First, the cohort observation period in Korea may not have been long enough to have produced changes in dietary patterns, and it may have been too early to draw conclusions about the effects of immigration on health status. Second, a 1-day 24-hour recall may be insufficient to assess usual daily intake due to large intra-individual variability in food and nutrient intake, but trained dietitians using standard protocols were employed to minimize bias and to aid the subjects when reflecting on their daily diet. Third, some communication problems were encountered, particularly with subjects who had lived for a relatively short time in Korea and had a low level of education, although Vietnamese translators fluent in both Korean and Vietnamese assisted whenever needed.
Although this study had some limitations, it was the first to investigate changes in daily food and nutrient intakes and blood profiles between baseline and follow-up among Vietnamese female marriage immigrants living in Korea. Moreover, the results may be helpful for developing nutritional programs in Vietnamese female marriage immigrants in Korea and could be a basis for further studies on international marriage immigrants.
In conclusion, overall dietary intake decreased in Vietnamese female marriage immigrants during the follow-up period. A long-term follow-up study is needed to assess the association between changes in consumption of milk and dairy products and biochemical indicators including blood hs-CRP levels in Vietnamese female marriage immigrants.
Figures and Tables
Table 1
General characteristics and anthropometric variables of Vietnamese female marriage immigrants at baseline and follow-up1)

Table 3
Daily nutrient intake and changes in proportion below the EER1) or EAR2) in Vietnamese female marriage immigrants3-5)

ACKNOWLEDGMENTS
This study was supported by a fund (2006-E71017-00, 2007-E71007-00, 2008-E71002-00, 2009-E71003-00, 2010-E71002-00) for research from the Korea Centers for Disease Control and Prevention and by the BK21 Project in 2011.
References
1. Statistics Korea. Population and households of Koreans [Internet]. Daejeon: Statistics Korea;2010. cited 2011. Available from: http://kostat.go.kr.
2. Ministry of Justice (KR). Immigration Service Statistics 2010. Gwacheon: Ministry of Justice;2010.
3. Ben-David A, Lavee Y. Migration and marital distress: the case of Soviet immigrants. J Divorce Remarriage. 1994; 21:133–146.
4. Kasper J, Gupta SK, Tran P, Cook JT, Meyers AF. Hunger in legal immigrants in California, Texas, and Illinois. Am J Public Health. 2000; 90:1629–1633.

6. Thomas M, Choi JB. Acculturative stress and social support among Korean and Indian immigrant adolescents in the United States. J Sociol Soc Welf. 2006; 33:123–143.
7. Smith A, Kaminskas G. Female Filipino migration to Australia: an overview. Asian Migr. 1992; 5:72–81.
8. Hofstede G. Gender stereotypes and partner preferences of Asian women in masculine and feminine cultures. J Cross Cult Psychol. 1996; 27:533–546.

9. Imamura AE. The loss that has no name: social womanhood of foreign wives. Gend Soc. 1988; 2:291–307.
10. Mirsky J, Kohn R, Levav I, Grinshpoon A, Ponizovsky AM. Psychological distress and common mental disorders among immigrants: results from the Israeli-based component of the World Mental Health Survey. J Clin Psychiatry. 2008; 69:1715–1720.
11. Garretson JA, Burton S. Effects of nutrition facts panel values, nutrition claims, and health claims on consumer attitudes, perceptions of disease-related risks, and trust. J Public Policy Mark. 2000; 19:213–227.

12. Heald AH, Sharma R, Anderson SG, Vyas A, Siddals K, Patel J, Bhatnagar D, Prabharkaran D, Rudenski A, Hughes E, Durrington P, Gibson JM, Cruickshank JK. Dietary intake and the insulin-like growth factor system: effects of migration in two related populations in India and Britain with markedly different dietary intake. Public Health Nutr. 2005; 8:620–627.

13. Whittemore AS, Wu-Williams AH, Lee M, Shu Z, Gallagher RP, Deng-ao J, Lun Z, Xianghui W, Kun C, Jung D, Teh CZ, Chengde L, Yao XJ, Paffenbarger RS Jr, Henderson BE. Diet, physical activity, and colorectal cancer among Chinese in North America and China. J Natl Cancer Inst. 1990; 82:915–926.

14. He J, Klag MJ, Wu Z, Qian MC, Chen JY, Mo PS, He QO, Whelton PK. Effect of migration and related environmental changes on serum lipid levels in southwestern Chinese men. Am J Epidemiol. 1996; 144:839–848.

15. Yang EJ, Chung HK, Kim WY, Bianchi L, Song WO. Chronic diseases and dietary changes in relation to Korean Americans' length of residence in the United States. J Am Diet Assoc. 2007; 107:942–950.

16. Choi HN, Chung HW, Hwang JY, Chang N. Intrahousehold discrepancy regarding food insecurity within intermarried couples of Vietnamese wives and Korean husbands in South Korea. Nutr Res Pract. 2011; 5:471–480.

17. Ministry of Culture and Tourism (KR). Immigrant Women of Culture and Art Educational Program. Seoul: Ministry of Culture and Tourism;2005.
18. Kang EJ. What are inside the Korean-Chinese international marriage?: an exploratory study. J Fam Relat. 1999; 4:61–80.
19. Kwon BS, Cha BH. The impact of communication and cultural identity on marital satisfaction among Kosian housewives in rural areas. Korean J Soc Welf. 2006; 58:109–134.
20. Lee HK. Marriage migration to South Korea: issues, problems, and responses. Korea J Popul Stud. 2005; 28:73–106.
21. Nord M, Andrews M, Carlson S. Food Insecurity in the United States, 2005. Washington, D.C.: U.S. Department of Agriculture;2006.
22. Lyu JE, Yang YJ, Lee SE, Chung HW, Kim MK, Kim WY. Nutritional status of Vietnamese female marriage immigrants to Korea in relation to length of residence in Korea. Ann Nutr Metab. 2009; 55:317–324.

23. Kim SH, Kim WY, Lyu JE, Chung HW, Hwang JY. Dietary intakes and eating behaviors of vietnamese female immigrants to Korea through marriage and Korean spouses and correlations of their diets. Korean J Community Nutr. 2009; 14:22–30.
24. Hwang JY, Lee SE, Kim SH, Chung HW, Kim WY. Psychological distress is associated with inadequate dietary intake in Vietnamese marriage immigrant women in Korea. J Am Diet Assoc. 2010; 110:779–785.

25. Khan NC, Hoan PV. Vietnam recommended dietary allowances 2007. Asia Pac J Clin Nutr. 2008; 17:Suppl 2. 409–415.
26. The Korean Nutrition Society. Dietary Reference Intakes for Koreans. Seoul: The Korean Nutrition Society;2010.
27. Kim WY, Cho MS, Lee HS. Development and validation of mini dietary assessment index for Koreans. Korean J Nutr. 2003; 36:83–92.
28. The Korean Nutrition Society, Nutrition Information Center. Nutritional assessment program, 'Can-pro 3.0' [CD-ROM]. Seoul: The Korean Nutrition Society;2006.
29. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972; 18:499–502.

30. Regev-Tobias H, Reifen R, Endevelt R, Havkin O, Cohen E, Stern G, Stark A. Dietary acculturation and increasing rates of obesity in Ethiopian women living in Israel. Nutrition. 2012; 28:30–34.

31. Rosenmöller DL, Gasevic D, Seidell J, Lear SA. Determinants of changes in dietary patterns among Chinese immigrants: a cross-sectional analysis. Int J Behav Nutr Phys Act. 2011; 8:42.

32. Lv N, Cason KL. Dietary pattern change and acculturation of Chinese Americans in Pennsylvania. J Am Diet Assoc. 2004; 104:771–778.

33. Neuhouser ML, Thompson B, Coronado GD, Solomon CC. Higher fat intake and lower fruit and vegetables intakes are associated with greater acculturation among Mexicans living in Washington State. J Am Diet Assoc. 2004; 104:51–57.

34. Ministry of Health and Welfare, Korea Center for Disease Control and Prevention. Korea Health Statistics 2008: Korea National Health and Nutrition Examination Survey (KNHANES IV-2). Cheongwon: Korea Center for Disease Control and Prevention;2009.
35. Méjean C, Traissac P, Eymard-Duvernay S, Delpeuch F, Maire B. Influence of acculturation among Tunisian migrants in France and their past/present exposure to the home country on diet and physical activity. Public Health Nutr. 2009; 12:832–841.

36. Huang B, Rodriguez BL, Burchfiel CM, Chyou PH, Curb JD, Yano K. Acculturation and prevalence of diabetes among Japanese-American men in Hawaii. Am J Epidemiol. 1996; 144:674–681.

37. Koya DL, Egede LE. Association between length of residence and cardiovascular disease risk factors among an ethnically diverse group of United States immigrants. J Gen Intern Med. 2007; 22:841–846.

38. Lee WP, Lingard J, Bermingham M. Insulin, lipid profiles and measures of fatness in Taiwanese women in relation to duration of residence in Australia. Asia Pac J Clin Nutr. 2007; 16:254–261.
39. Gewurz H, Mold C, Siegel J, Fiedel B. C-reactive protein and the acute phase response. Adv Intern Med. 1982; 27:345–372.
40. Pai JK, Pischon T, Ma J, Manson JE, Hankinson SE, Joshipura K, Curhan GC, Rifai N, Cannuscio CC, Stampfer MJ, Rimm EB. Inflammatory markers and the risk of coronary heart disease in men and women. N Engl J Med. 2004; 351:2599–2610.

41. Ridker PM, Rifai N, Rose L, Buring JE, Cook NR. Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. N Engl J Med. 2002; 347:1557–1565.

42. Holmboe-Ottesen G, Wandel M. Changes in dietary habits after migration and consequences for health: a focus on South Asians in Europe. Food Nutr Res. 2012; 56:18891.

43. Kwon HT, Lee CM, Park JH, Ko JA, Seong EJ, Park MS, Cho B. Milk intake and its association with metabolic syndrome in Korean: analysis of the third Korea National Health and Nutrition Examination Survey (KNHANES III). J Korean Med Sci. 2010; 25:1473–1479.

44. Lee SS, Kim SL, Kim SH. An association between milk consumption and serum lipid profiles of postmenopausal women in Korea. Korean J Nutr. 2005; 38:144–150.
45. Panagiotakos DB, Pitsavos CH, Zampelas AD, Chrysohoou CA, Stefanadis CI. Dairy products consumption is associated with decreased levels of inflammatory markers related to cardiovascular disease in apparently healthy adults: the ATTICA study. J Am Coll Nutr. 2010; 29:357–364.

46. Qureshi MM, Singer MR, Moore LL. A cross-sectional study of food group intake and C-reactive protein among children. Nutr Metab (Lond). 2009; 6:40.

47. Denke MA, Fox MM, Schulte MC. Short-term dietary calcium fortification increases fecal saturated fat content and reduces serum lipids in men. J Nutr. 1993; 123:1047–1053.
48. Ejtahed HS, Mohtadi-Nia J, Homayouni-Rad A, Niafar M, Asghari-Jafarabadi M, Mofid V, Akbarian-Moghari A. Effect of probiotic yogurt containing Lactobacillus acidophilus and Bifidobacterium lactis on lipid profile in individuals with type 2 diabetes mellitus. J Dairy Sci. 2011; 94:3288–3294.

49. Ma KY, Yang N, Jiao R, Peng C, Guan L, Huang Y, Chen ZY. Dietary calcium decreases plasma cholesterol by down-regulation of intestinal Niemann-Pick C1 like 1 and microsomal triacylglycerol transport protein and up-regulation of CYP7A1 and ABCG 5/8 in hamsters. Mol Nutr Food Res. 2011; 55:247–258.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download