This article has been corrected. See "Erratum: Funding Acknowledgment" in Volume 6 on page 474.
Abstract
Radiation used in cancer treatment may cause side effects such as inflammation. Quercetin is a polyphenol that reduces inflammation. This study evaluated the recovery efficacy of quercetin on impaired immune function in irradiation-induced inflammatory mice. Quercetin administered at two concentrations of 10 and 40 mg/kg body weight was initiated 2 weeks before irradiation and was continued 30 days after irradiation. The animals exposed/not exposed to radiation were sacrificed on radiation days 10 and 30. Splenocyte proliferation, which was diminished after irradiation, was enhanced significantly by quercetin supplementation after 30 days of irradiation. Cytokine secretion increased in the radiation group compared to that in the non-radiation control group. After 30 days of radiation, interleukin (IL)-1β and IL-6 secretion decreased significantly in the radiation-quercetin groups. When quercetin was administered for 44 days, it showed a possible protective effect against irradiation-induced inflammation in mice. Quercetin could be beneficial in the recovery of irradiation-induced increases in cytokine secretion.
Many medicines are being developed to treat chronic diseases, including cancer, but their effects are limited. Therefore, it is important to develop healthy foods that have low toxicity but high treatment effects using natural resources [1]. Various studies have reported that the occurrence of chronic diseases, including cancer, is low in areas where individuals eat sufficient fruits and vegetables [2,3]. This preventive effect is due to antioxidant compounds present as bioactive materials in vegetables [4,5].
Various types of antioxidant compounds are active against reactive oxygen species produced during metabolism and reduce oxidative damage of DNA, proteins, amino acids, and lipids. These compounds also prevent the initiation or decrease the duration of inflammation by controlling the expression of various proteins; thus, preventing diseases such as cancer, rheumatoid arthritis, and stroke [6,7]. The most effective antioxidants in food that reduces oxidation stress in the body are polyphenols. Quercetin is a type of polyphenol and a renowned antioxidant that effectively prevents cancer by removing free radicals [8,9]. Quercetin is normally ingested in vegetables and red-colored fruits [2]. The medicinal properties of quercetin are well known and include the reduction of lipid peroxides [10] and carcinogenetic materials, inhibition of mutant cancer cell growth [11], and anti-bacterial effects [12]. Radiation treatment is administered to 50-60% of patients with cancer [1,13] However, it damages normal cells and causes nutritional problems.
Radiation-induced cell death is an immunogenic process that can be potentially exploited to stimulate tumor-specific immune responses [14]. Some researchers have suggested that pro- and anti-inflammatory cytokines can be used as markers to predict radiation-induced immunocompromised status [15,16]. Interleukin (IL)-12 induces interferon-gamma, IL-6, and tumor necrosis factor (TNF)-α production; stimulates T and natural killer cells; promotes T cell responses; and inhibits neovascularization [17].
The severity of the nutritional problems related to radiation treatment, which include weight loss, depends on the location and amount of treatment, tissue thickness, nutritional status, tissue sensitivity, and psychological status of the patient. Radiation treatment causes stomatitis, mucositis, esophagitis, gastroenteritis, loss of taste, nausea, vomiting, diarrhea, constipation, bleeding, and proctitis, which lead to difficulties eating and in digestion [18,19]. Malnutrition caused by radiation weakens immunity, which, in turn, increases the rate of infection, reduces the reaction to treatment, weakens the whole body, reduces quality of life, and ultimately leads to death [20,21].
Some researchers have studied the immune-enhancing activities of quercetin. However, most results were obtained in cell culture studies. In addition, no data are available on the use of quercetin for mitigating the adverse effects of radiation therapy. Hence, in this study, we induced inflammation by exposing mice to radiation. The mice were orally administered quercetin for 6 weeks, and we determined changes in weight, splenocyte proliferation, T lymphocyte composition in blood, cytokine (i.e., IL-1β, IL-6, and TNF-α) secretion levels, and blood protein levels (i.e., total protein and albumin) to clarify the effect of orally administered quercetin on immunity and nutritional indices of mice that received radiation treatment.
We purchased quercetin dehydrate from Sigma Chemical Co. (St. Louis, MO, USA). The animals were 6-week-old female ICR mice weighing 24-26 g (Central Laboratory Animal Inc., Seoul, Korea), and they were housed in the laboratory at 22 ± 2℃ and 40-60% humidity with a 12-hour light/12-hour photoperiod. The mice had free access to solid feed and water and were allowed to acclimatize for 1 week before the experiment. The animals were divided into six groups, which received different radiation and quercetin doses. Quercetin was dissolved in distilled water and administered orally for 10 or 30 days. The groups were further divided into normal groups (NC: normal control group, QC10: control group orally administered quercetin at 10 mg/kg body weight [bw], and QC40: a control group orally administered quercetin at 40 mg/kg bw) and radiation groups (RC: radiation control group, QR10: radiation group orally administered quercetin at 10 mg/kg bw, and QR40: radiation group orally administered quercetin at 40 mg/kg bw). Quercetin (10 or 40 mg/kg of body weight) was provided on alternate days throughout the experimental period. All animal procedures were in accordance with the guidelines for the care and use of laboratory animals issued by Sookmyung Women's University.
Based on the results of our pilot study [22] and another report [23], a dose of 15 Gy was chosen for evaluating the time sequential changes in the mice. Before radiation, all mice were injected intramuscularly with 0.4 mL ketamine (0.8 mL) and xylazine (0.5 mL) to induce paralysis. A single 15-Gy dose of radiation was administered to the mice in the small intestinal area using a linear accelerator to induce inflammation at 2 weeks after quercetin administration. The mice were sacrificed on days 10 and 30 after irradiation. The irradiation was performed in the Department of Radiation Oncology, Ajou University of Medicine, Suwon, Republic of Korea.
Splenocytes were separated using the method of Mishell and Shiigi [24]. To measure splenocyte proliferation, splenocyte suspensions in each group were diluted and plated on 96-well plates (Corning, Corning, NY, USA). and Con A (5 µg/mL) and lipopolysaccharide (LPS) (15 µg/mL; Sigma Co., St. Louis, MO, USA) were used as mitogens. Optical density was measured using an enzyme-linked immunoassay (ELISA) reader at 540 nm for the MTT assay.
The proliferation index was calculated as follows: proliferation index = optical density in the sample well/optical density in the control well.
Blood T lymphocyte levels were measured in samples collected by heart puncture from mice in each group. Monoclonal mouse CD3-FITC, CD4-PE, and CD8-PE antibodies were purchased from Immunotech (Beckman Coulter Inc., Marseille, France). Immunostaining was performed according to the manufacturer's instructions. Briefly, 100 µL of whole blood was incubated with 20 µL of anti-CD3, anti-CD4, or anti-CD8 antibodies for 15 min at room temperature in the dark. The cells were then incubated in 500 µL of Optilyse C Solution for 15 min to lyse red blood cells, washed twice with 1 × phosphate-buffered saline (PBS), resuspended in 500 µL of 1 × PBS, and analyzed by flow cytometry (Coulter Epics XL, Brea, CA, USA).
The blood samples collected by heart puncture were centrifuged for 30 minutes at 800 × g, at 4℃. Blood serum was then extracted, and an ELISA cytokine kit (BioSource, Ann Arbor, MI, USA) was used to measure IL-1β, IL-6, and TNF-α levels.
All indices were measured in blood serum. Total protein content was measured by reading the optical density at 540 nm using the Burette method and Clinimate TP (Hitachi 7600-210, Tokyo, Japan) as the indicator. Albumin levels were measured by observing the optical density at 630 nm using the BCC method and Clinimate ALB as the indicator.
The changes in body weight over 6 weeks are shown in Fig. 1. Mice in the radiation group showed a rapid decrease in body weight after 5 days of radiation. However, these mice began to recover lost weight, and the recovery rate started to decelerate from irradiation day 20. Although no significant difference was observed between the quercetin and non-quercetin groups after radiation, the group receiving quercetin showed a more rapid increase in weight.
The splenocyte proliferation observations are shown in Table 1. After day 10 of oral quercetin administration, the group not exposed to radiation showed a higher spleen index than that of the group exposed to radiation. In the experiment in which splenocyte proliferation was induced by Con A activation, which selectively induces T cell proliferation (cells related to cell immunity), the QR10 group showed higher splenocyte proliferation than that in the non-RC group after day 30. In the experiment in which splenocyte proliferation was induced by LPS activation, which selectively induces B cell proliferation (cells related to humoral immunity), the QR10 group tended to show higher splenocyte proliferation than that in the other groups, but the difference was not significant. The RC group showed splenocyte proliferation indices of 0.48 ± 0.05 and 0.30 ± 0.03 after 10 days of radiation exposure to the abdomen and oral administration of quercetin when stimulated with Con A and LPS, respectively, indicating that splenocyte proliferation decreased after radiation exposure. When quercetin was orally administered for 30 days, the groups exposed and not exposed to different doses of radiation showed differences in splenocyte proliferation; the RC group exhibited the lowest splenocyte proliferation. Upon inducing splenocyte proliferation with Con A and LPS, the QR10 group showed the highest level of splenocyte proliferation.
The results of this experiment are shown in Figs. 2 and 3. No significant difference in the levels of CD4+ cells, (helper T cells) was observed after 10 and 30 days of radiation exposure, despite the changes in exposure status and variations in concentrations. The RC group on day 10 of radiation had significantly higher levels of CD8+ cells (cytotoxic T cells) than those in the NC group. Although significant differences were observed due radiation exposure, the changes in exposure status or variations in concentration did not produce significant differences in CD4+ and CD8+ T-lymphocytes after 10 days of radiation, except that the CD4+/CD8+ ratio was lower in the RC group than that in the NC group because of the effect of CD8+ cells. After 30 days of radiation, no significant difference was observed between the groups despite changes in exposure status and variations in concentration (Table 2).
The levels of IL-1β, IL-6, and TNF-α in blood were measured after inducing inflammation in mice by exposure to radiation and oral administration of quercetin for 6 weeks and are shown in Table 3. IL-1β levels were higher on day 10 of radiation than those on day 30. This result shows that inflammation was initially induced by radiation in the small intestine, which, in turn, increased cytokine secretion and subsequently ameliorated the anti-inflammation reaction, probably because of oral quercetin administration. The QR10 and QR40 groups showed lower IL-1β levels than those in the RC group after 10 and 30 days of radiation. After day 10 of radiation, the QR10 and QR40 groups tended to show lower IL-6 levels than those in the RC group, but the difference was not significant. However, the difference between these groups was significant after 30 days, and the QR10 group showed the lowest level. The QR10 and QR40 groups showed lower TNF-α levels than those in the RC group after 10 days of radiation. Furthermore, TNF-α secretion was significantly lower in the QR10 and QR40 groups than that in the RC group on day 10 of radiation.
After inducing inflammation in the mice by exposure to radiation and oral administration of quercetin for 6 weeks, the protein indices in blood were measured and are shown in Table 4. The protein levels observed after day 10 of radiation were significantly higher in the non-radiation groups than those in the radiation groups. The group exposed to radiation and administered quercetin tended to have higher protein levels than those in the RC group, but the difference was not significant. However, the QR10 and QR40 groups had higher protein levels than those in the RC group after 30 days of radiation. The albumin levels observed on day 10 of radiation differed significantly between the non-radiation and radiation groups. However, this difference was not observed after 30 days of radiation. The QR10 and QR40 groups tended to have higher albumin levels than those in the RC group, but the difference was not significant. Significant differences were observed between the groups with respect to cholesterol levels on day 30 of radiation.
This study analyzed splenocyte proliferation after administering various concentrations of quercetin to mice to reveal the effects of quercetin on activation of the immune response in animals exposed to radiation. Patients with cancer receiving radiation treatment incorporate various fruits and vegetables containing quercetin into their diet. Patients receiving radiation treatment lose 5% of their normal weight during the treatment period [25]. The results of our study show that the main adverse effect of radiation treatment was weight loss and this has been confirmed in other studies. In particular, the results of our study are identical to those of a previous study [26] in that the reasons for the weight loss over 5 days and the subsequent recovery were enzyme activation and increased protein levels due to inflammation of the small intestine after 1 day of radiation followed by a recovery beginning after 4 days. which may have been due to relief of inflammation in the small intestine. Splenocytes, bone marrow cells, and thymocytes are the major cells used to investigate the immune reaction. Furthermore, the organs of laboratory animals are used to measure cell proliferation to determine the effects of food within the body [27]. The spleen is an organ in which various lymphocytes such as T lymphocytes, B lymphocytes, and macrophages are densely aggregated. The size and number of splenocytes are related to the strength of immunity [28]. We showed that splenocyte proliferation was restricted by exposure to radiation, which can be considered an adverse effect of radiation [29,30]. This adverse effect was relieved by orally administering quercetin. A fundamental aspect of the immune system is the induction and regulation of proliferation of specific immune cell populations. The spleen is the major site of immune responses to blood-borne antigens and is also a site of hematopoiesis in rodents [31]. Splenocyte proliferation after day 10 of radiation was less than that observed after the day 30. This is because complete absorption and metabolism could not occur because of inflammation in the small intestine. The increase in proliferation on day 30 of radiation occurred because of relief of inflammation and the increased number of immune cells. Thus, long-term administration of quercetin improved splenic immune cell proliferation after radiation exposure. No significant difference in the CD4+/CD8+ ratio was observed despite the exposure status and concentration variation, and only after 10 days did the CD4+/CD8+ ratio show a significant difference in response to radiation. The number and ratio of T lymphocytes decreased due to poor calorie and protein intake. These changes were reversed promptly by nutritional treatment. Therefore, the number and ratio of T lymphocytes are important standards for estimating nutritional status [32] and identifying possible infectious diseases [33,34]. This result shows that although quercetin may not affect T-lymphocyte subsets directly, it may affect other immune functions.
Cytokines are not only involved in organic reactions against antigens between cells and tissues and other external factors but also control hematogenesis, immune reactions, and inflammation, consequently, cytokines are closely related to various pathological phenomena [30]. IL-1β is initially secreted to activate T cells, and IL-6 is then secreted and participates in B and T cell differentiation [35,36]. TNF-α is one of the cytokines produced by mononuclear phagocytes; it is toxic to cancer cells and has an anti-viral effect [37]. The present results identified the secretion levels of these cytokines in blood and investigated the effects of orally administered quercetin in mice exposed to radiation. Acute effects such as weight loss, dehydration, and vomiting appeared on day 10 of radiation; these symptoms were moderated by day 30 of radiation, when long-term effects became evident. Symptoms that appeared on days 10 and 30 of radiation determined the effects of quercetin on the moderation of acute and chronic symptoms. Secretion of IL-1β and IL-6 was decreased significantly in the groups that were orally administered quercetin, whereas TNF-α levels tended to decrease, albeit insignificantly. In general, the secretion levels of pro-inflammatory cytokines (i.e., IL-1β, IL-6, and TNF-α) increase in patients with cancer [38]. Various drugs have been developed and used to reduce increased cytokine levels in patients with cancer [39,40]. According to the results of our experiment, because the levels of inflammatory cytokines decreased in the groups orally administered quercetin, oral administration of quercetin was considered to moderate inflammation, and its effect on the suppression of cytokine secretion was most significant at 10 mg/kg bw. Furthermore, quercetin effectively moderated inflammation, because the cytokine levels recovered on day 30 of radiation in the group orally administered quercetin.
Radiation affects cells present in areas subjected to radiation, which ultimately causes digestive malfunction if the gastrointestinal tract is exposed. The severity of nutritional problems, including weight loss, differ depending on the investigated region, quantity to be investigated, thickness of the investigated tissue subjected to radiation, nutritional status at the time of starting treatment, sensitivity of the tissue, and physical and mental status [41,42]. Radiation of the intestine causes nausea, vomiting, diarrhea, and defective nutritional absorption, and acute enteritis causes intestinal obstruction, ulcers, small bowel perforation, and fibrosis, leading to chronic enteritis. Ultimately, nutritional loss results in malnutrition. These problems may begin 2-3 weeks after starting treatment but often subside when treatment is completed. However, in some patients, these effects may become chronic. Most nutrition guidelines recommend that patients undergoing such treatment eat vegetables, fruits, and whole-grain products and limit the amount of red meat. However, when patients are being treated for cancer, nutritionists recommend eating high-fat, high-protein, and high-calorie foods to maintain normal weight [43]. This is because many patients undergoing radiotherapy are already experiencing nutritional problems and weight loss [44]. In the mice exposed to radiation and orally administered quercetin, no effects of quercetin on protein levels were observed after day 10 of radiation, but an effect was observed after 30 days of radiation. Quercetin increased total protein and albumin levels that were reduced by radiation. Therefore, administration of quercetin improved immune function and nutritional status, which were negatively affected by radiation. However, additional research on this topic is essential
The average daily intake of quercetin reaches 30 mg in most Western countries [45]. The bioavailability of quercetin depends on the metabolic form present in the food. According to recommendations, the average daily intake of quercetin for mice should be calculated using the formula for dose transition based on the body surface area normalization method [46]. This calculation provides a mouse-equivalent quercetin dose of 6.8 mg/kg bw The limited solubility of quercetin in water presents a major problem for chemopreventive administration. Many studies have investigated potential difficulties in quercetin transport to various tissues [47]. In this study, we used two concentrations of quercetin; 10 mg/kg bw as a lower concentration and 40 mg/kg bw as the higher concentration. Most of our experimental results indicated that the groups receiving quercetin at doses of 10 mg/kg bw showed positive effects on splenocyte proliferation, cytokine secretion, and total protein and albumin levels. Because high dose quercetin administration is less efficient than normal doses, this likely holds true for patients undergoing radiotherapy.
The quercetin treatment helped recover the cytokine levels at the lower dose of supplementation (i.e., 10 mg/kg bw oral administration) in the irradiated mice. However, the effective quercetin dose may differ depending on physical parameters. In conclusion, the results of this study verify that quercetin increased immune function, relieved inflammation, and enhanced nutritional status in irradiated mice. We expect our findings to be used as a basis for developing functional food products that contain quercetin to improve decreased immune function during radiation treatment for cancer.
Figures and Tables
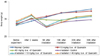 | Fig. 1Changes in body weights of mice orally administered quercetin and treated with or without irradiation for 6 weeks |
 | Fig. 2
Percentage of CD4+ lymphocytes in mice orally administered quercetin and treated with or without irradiation. Values are mean ± standard deviation for six mice per group (P < 0.05). NS, not significant. |
 | Fig. 3
Percentage of CD8+ lymphocytes in mice orally administered quercetin and treated with or without irradiation. Values are mean ± standard deviation in six mice per group (P < 0.05). Means with different letters (a, b) are significantly different at α = 0.05 as determined by Duncan's multiple range test (a > b). NS, not significant. |
Table 1
Proliferation of splenocytes in mouse orally administered quercetin treated and treated with or without irradiation (10 and 30 days of radiation)

Table 2
Percentage of CD4+/CD8+ lymphocytes in mice orally administered
quercetin and treated with or without irradiation (10 and 30 days of radiation)

Table 3
Cytokine (IL-1β, IL-6, TNF-α) secretion in serum of mice orally administered quercetin and treated with or without irradiation (10 and 30 days of radiation)

References
1. Kim SH, Jo SK, Kwon OD. The radioprotective effects of rhizomata herbs. J Radiat Prot. 2001. 26:13–18.
2. Hertog MG, Hollman PC, Katan MB, Kromhout D. Intake of potentially anticarcinogenic flavonoids and their determinants in adults in The Netherlands. Nutr Cancer. 1993. 20:21–29.

3. Sharafetdinov KhKh, Plotnikova OA, Voznyĭ EK. Nutrition management of the cancer patients: modern view on problem. Vopr Pitan. 2008. 77:4–14.
4. Mojzisová G, Kuchta M. Dietary flavonoids and risk of coronary heart disease. Physiol Res. 2001. 50:529–535.
5. Giugliano D. Dietary antioxidants for cardiovascular prevention. Nutr Metab Cardiovasc Dis. 2000. 10:38–44.
6. Halliwell B, Rafter J, Jenner A. Health promotion by flavonoids, tocopherols, tocotrienols, and other phenols: direct or indirect effects? Antioxidant or not? Am J Clin Nutr. 2005. 81:268S–276S.

7. Heo BG, Chon SU, Park YJ, Bae JH, Park SM, Park YS, Jang HG, Gorinstein S. Antiproliferative activity of Korean wild vegetables on different human tumor cell lines. Plant Foods Hum Nutr. 2009. 64:257–263.

8. Bors W, Saran M. Radical scavenging by flavonoid antioxidants. Free Radic Res Commun. 1987. 2:289–294.

9. Gavelová M, Hladíková J, Vildová L, Novotná R, Vondrácek J, Krcmár P, Machala M, Skálová L. Reduction of doxorubicin and oracin and induction of carbonyl reductase in human breast carcinoma MCF-7 cells. Chem Biol Interact. 2008. 176:9–18.

10. Cai Q, Rahn RO, Zhang R. Dietary flavonoids, quercetin, luteolin and genistein, reduce oxidative DNA damage and lipid peroxidation and quench free radicals. Cancer Lett. 1997. 119:99–107.

11. Avila MA, Velasco JA, Cansado J, Notario V. Quercetin mediates the down-regulation of mutant p53 in the human breast cancer cell line MDA-MB468. Cancer Res. 1994. 54:2424–2428.
12. Nagata H, Takekoshi S, Takeyama R, Homma T, Yoshiyuki Osamura R. Quercetin enhances melanogenesis by increasing the activity and synthesis of tyrosinase in human melanoma cells and in normal human melanocytes. Pigment Cell Res. 2004. 17:66–73.

13. Garabige V, Giraud P, De Rycke Y, Girod A, Jouffroy T, Jaulerry C, Brunin F, Rodriguez J. Impact of nutrition management in patients with head and neck cancers treated with irradiation: is the nutritional intervention useful? Cancer Radiother. 2007. 11:111–116.
14. Kamrava M, Bernstein MB, Camphausen K, Hodge JW. Combining radiation, immunotherapy, and antiangiogenesis agents in the management of cancer: the Three Musketeers or just another quixotic combination? Mol Biosyst. 2009. 5:1262–1270.

15. Toda M, Wang L, Ogura S, Torii M, Kurachi M, Kakimi K, Nishikawa H, Matsushima K, Shiku H, Kuribayashi K, Kato T. UV irradiation of immunized mice induces type 1 regulatory T cells that suppress tumor antigen specific cytotoxic T lymphocyte responses. Int J Cancer. 2011. 129:1126–1136.

16. Gaton DD, Lichter H, Avisar I, Slodovinic D, Solomon AS. Lymphocytic reaction to ultraviolet radiation on rabbit conjunctiva. Ann Ophthalmol (Skokie). 2007. 39:128–133.

17. Sgadari C, Angiolillo AL, Tosato G. Inhibition of angiogenesis by interleukin-12 is mediated by the interferon-inducible protein 10. Blood. 1996. 87:3877–3882.

18. Gwak HS, Yoo HJ, Youn SM, Lee DH, Kim MS, Rhee CH. Radiosurgery for recurrent brain metastases after whole-brain radiotherapy : factors affecting radiation-induced neurological dysfunction. J Korean Neurosurg Soc. 2009. 45:275–283.

19. Rao V, Chaukar D, D'Cruz AK. Hypercalcemia and treated breast cancers: the diagnostic dilemma. J Cancer Res Ther. 2009. 5:46–48.

20. Barros GC, Labate RC. Psychological repercussions related to brachytherapy treatment in women with gynecological cancer: analysis of production from 1987 to 2007. Rev Lat Am Enfermagem. 2008. 16:1049–1053.

21. Ghadjar P, Vock J, Vetterli D, Manser P, Bigler R, Tille J, Madlung A, Behrensmeier F, Mini R, Aebersold DM. Acute and late toxicity in prostate cancer patients treated by dose escalated intensity modulated radiation therapy and organ tracking. Radiat Oncol. 2008. 3:35.

22. Lee YR, Jung JH, Kim HS. Hesperidin partially restores impaired immune and nutritional function in irradiated mice. J Med Food. 2011. 14:475–482.

23. Kim KO, Chun M, Kang S, Kim HS. Effect of high protein diet and resveratrol supplementation on the nutritional status and immunoreactivity in the irradiation-induced inflammatory rats. Korean J Nutr. 2009. 42:605–614.

24. Mishell BB, Shiigi SM. Selected Methods in Cellular Immunology. 1980. San Francisco: Freeman.
25. Gosselin TK, Gilliard L, Tinnen R. Assessing the need for a dietitian in radiation oncology. Clin J Oncol Nurs. 2008. 12:781–787.

26. Bhanja P, Saha S, Kabarriti R, Liu L, Roy-Chowdhury N, Roy-Chowdhury J, Sellers RS, Alfieri AA, Guha C. Protective role of R-spondin1, an intestinal stem cell growth factor, against radiation-induced gastrointestinal syndrome in mice. PLoS One. 2009. 4:e8014.

27. Nagai H, Nishiyori T, Ochi T, Imai Y, Tanaka H, Inagaki N. The effect of methanolic extract from Corydalis Tuber on cytokine production and allergic reactions in experimental animals. J Tradit Med. 1999. 16:51–57.
28. Peter W. Understanding Immunology. 2006. 2nd edition. Harlow, England: Pearson Prentice Hall;98–110.
29. Taylor CW, Nisbet A, McGale P, Darby SC. Cardiac exposures in breast cancer radiotherapy: 1950s-1990s. Int J Radiat Oncol Biol Phys. 2007. 69:1484–1495.

30. Yokoyama Y, Sakamoto K, Arai M, Akagi M. Radiation and surgical stress induce a significant impairment in cellular immunity in patients with esophageal cancer. Jpn J Surg. 1989. 19:535–543.

31. Batista FD, Harwood NE. The who, how and where of antigen presentation to B cells. Nat Rev Immunol. 2009. 9:15–27.

32. Osada J, Kamocki Z, Rusak M, Dabrowska M, Kedra B. The effect of surgical and nutritional treatment on activation parameters of peripheral blood T lymphocytes in stomach cancer patients in postoperative period. Pol Merkur Lekarski. 2008. 24:231–236.
33. Jiang W, Kang L, Lu HZ, Pan X, Lin Q, Pan Q, Xue Y, Weng X, Tang YW. Normal values for CD4 and CD8 lymphocyte subsets in healthy Chinese adults from Shanghai. Clin Diagn Lab Immunol. 2004. 11:811–813.

34. Nagel JE, Chopra RK, Chrest FJ, McCoy MT, Schneider EL, Holbrook NJ, Adler WH. Decreased proliferation, interleukin 2 synthesis, and interleukin 2 receptor expression are accompanied by decreased mRNA expression in phytohemagglutinin-stimulated cells from elderly donors. J Clin Invest. 1988. 81:1096–1102.

35. Rechciński T, Grebowska A, Kurpesa M, Sztybrych M, Peruga JZ, Trzos E, Rudnicka W, Krzemińska-Pakuła M, Chmiela M. Interleukin-1b and interleukin-1 receptor inhibitor gene cluster polymorphisms in patients with coronary artery disease after percutaneous angioplasty or coronary artery bypass grafting. Kardiol Pol. 2009. 67:601–610.
36. Meng Z, Liu Y, Wu D. Effect of sulfur dioxide inhalation on cytokine levels in lungs and serum of mice. Inhal Toxicol. 2005. 17:303–307.

37. Meydani SN. Dietary modulation of cytokine production and biologic functions. Nutr Rev. 1990. 48:361–369.

38. Wu KS, Zhou X, Zheng F, Xu XQ, Lin YH, Yang J. Influence of interleukin-1 beta genetic polymorphism, smoking and alcohol drinking on the risk of non-small cell lung cancer. Clin Chim Acta. 2010. 411:1441–1446.

39. Hepgül G, Tanrikulu S, Unalp HR, Akguner T, Erbil Y, Olgaç V, Ademoğlu E. Preventive effect of pentoxifylline on acute radiation damage via antioxidant and anti-inflammatory pathways. Dig Dis Sci. 2010. 55:617–625.

40. Calveley VL, Khan MA, Yeung IW, Vandyk J, Hill RP. Partial volume rat lung irradiation: temporal fluctuations of in-field and out-of-field DNA damage and inflammatory cytokines following irradiation. Int J Radiat Biol. 2005. 81:887–899.

41. Van Cutsem E, Arends J. The causes and consequences of cancer-associated malnutrition. Eur J Oncol Nurs. 2005. 9:Suppl 2. S51–S63.

42. Isenring EA, Bauer JD, Capra S. Nutrition support using the American Dietetic Association medical nutrition therapy protocol for radiation oncology patients improves dietary intake compared with standard practice. J Am Diet Assoc. 2007. 107:404–412.

43. Rockenbach G, Di Pietro PF, Ambrosi C, Boaventura BC, Vieira FG, Crippa CG, Da Silva EL, Fausto MA. Dietary intake and oxidative stress in breast cancer: before and after treatments. Nutr Hosp. 2011. 26:737–744.
44. Kröner A, Stoll H, Spichiger E. Malnutrition and weight lossnurse assessment of nutritional status and counselling: experiences of patients with newly diagnosed or relapsed cancer. Pflege. 2012. 25:85–95.

45. Noroozi M, Burns J, Crozier A, Kelly IE, Lean ME. Prediction of dietary flavonol consumption from fasting plasma concentration or urinary excretion. Eur J Clin Nutr. 2000. 54:143–149.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download