Abstract
This study was conducted to identify dietary factors that may affect the occurrence of gastric cancer in Koreans. Preoperative daily nutrition intake and diet quality of patients diagnosed with gastric cancer were evaluated. Collected data were comparatively analyzed by gender. The results were then used to prepare basic materials to aid in the creation of a desirable postoperative nutrition management program. The subjects of this study were 812 patients (562 men and 250 women) who were diagnosed with gastric cancer and admitted for surgery at Soonchunhyang University Hospital between January 2003 and December 2010. Nutrition intake and diet quality were evaluated by the 24-hr recall method, the nutrient adequacy ratio, mean adequacy ratio (MAR), nutrient density (ND), index of nutritional quality (INQ), dietary variety score (DVS), and dietary diversity score (DDS). The rate of skipping meals and eating fast, alcohol consumption, and smoking were significantly higher in males than those in females. The levels of energy, protein, fat, carbohydrate, phosphorous, sodium, potassium, vitamin B1, vitamin B2, niacin, and cholesterol consumption were significantly higher in males than those in females. Intake of fiber, zinc, vitamin A, retinol, carotene, folic acid were significantly higher in females than those in males. MAR in males was significantly higher (0.83) than that in females (0.79). INQ values were higher in females for zinc, vitamin A, vitamin B2, vitamin B6, and folic acid than those in males. The average DVS was 17.63 for females and 13.19 for males. The average DDS was 3.68 and the male's average score was 3.44, whereas the female's average score was 3.92. In conclusion, males had more dietary habit problems and poor nutritional balance than those of females. Our findings suggest that proper nutritional management and adequate dietary education for the primary prevention of gastric cancer should be emphasized in men.
Gastric cancer incidence has been decreasing and the rate of complete recovery is increasing due to early detection and treatment. However, gastric cancer is still a frequently occurring cancer in Korea and is ranked second in terms of cancer mortality [1]. Although the global incidence of gastric cancer is decreasing gradually, gastric cancer will still display an absolute increasing trend until 2050 [2].
Factors contributing to the development of gastric cancer include hereditary and endocrinological, immunological, and environmental factors including diet [3]. Studies on nutrition and gastric cancer have suggested the relevance of dietary factors. Certain habits including smoking and drinking have been associated with the outbreak of gastric cancer [4]; and sufficient intake of fresh vegetables, fruits, and nutrients such as carotene, vitamin E, vitamin C and selenium, known as anticancer nutrients, lower the risk of gastric cancer [5]. In contrast, frequent consumption of meat [6] and foods with high salt content increase the risk for gastric cancer [7].
Studies assessing food and nutrient intake of local residents [8] and comparing certain patients against control groups in terms of diet [9] were actively conducted in the 1990s, and the early 2000s in Korea. Since then, studies have been carried out mainly on various nutritive conditions. However, there are an insufficient number of studies on dietary habits of different populations in comparison to countries where gastric cancer incidence is high. Additional intake of salt by 1 g daily increases gastric cancer incidence by approximately 18%, but the same result was not produced in a number of cohort studies [10]. Pham et al. [11] concluded that excessive dairy products in the diet lowers gastric cancer mortality only in males. A new study by Kim et al. [12], which compared Korean and Japanese populations, suggested that only the consumption of fermented beans increases gastric cancer incidence. Thus, fundamental studies need to be conducted continuously to prevent overlooking the causes of gastric cancer based on dietary factors that are already known.
Following a gastric cancer operation, the nutritive intake goals of a patient is set by analyzing the nutritive conditions, size of meals, and dietary balance of the patient prior to the operation. An overall assessment of diet quality is necessary together with a determination of excessive or insufficient supply of individual nutrients rather than simply identifying the dietary habits of the patient. However, related studies have not been conducted targeting patients with gastric cancer.
Accordingly, this study evaluated the nutrition intake and diet quality by surveying the daily dietary habits and food intake of patients with gastric cancer before a gastric cancer diagnosis. The dietary differences between men and women were also analyzed.
We attempted to establish desirable nutritional intake guidelines by assessing the preoperative dietary condition of the patients to aid in the management of their postoperative nutrition.
A total of 948 patients were hospitalized and underwent surgery following a diagnosis of gastric cancer at Soonchunhyang University Hospital Bucheon from January 2003 to December 2010. In total, 812 patients with gastric cancer who received sufficient explanation of the objectives and methods of this study (in accordance with the Institutional Review Board) and who provided informed consent to participate in the study were included. Information on patients were entered prospectively in The Gastric Cancer Patient Registry of the research institute, and some of these data were used in this study. All investigations were made based on daily diets without any changes in food intake or dietary habits caused by the gastric cancer diagnosis. All data were classified by gender (562 men and 250 women) and were analyzed accordingly.
Patient weight and height were measured using an automatic body composition analyzer (Biospace In-body 3.0, Seoul, Korea) and their body mass index (BMI) was calculated. Triceps skin fold thickness (TSF) was measured using a large skin fold caliper (All-Tech Medical, Cleveland, OH, USA). A tape measure was used to measure the thinnest part between the ribs and pelvis while the patient was standing up for the waist measurement.
A self-reported questionnaire was used to examine the dietary habits of the patients with items focusing on appetite, meal regularity, skipping meals, eating speed, alcohol intake, smoking, exercise and taste preferences.
Skilled clinical nutritionists interviewed patients using photographs of food items and a booklet containing eye measurement data as aids for the nutrient intake survey. Data on dietary intake amount were collected using the 24-hr recall method and were analyzed with the CAN program (The Korean Nutrition Society, ver. 3.0).
The nutrient adequacy ratio (NAR) and mean adequacy ratio (MAR) were calculated to assess the appropriateness of nutrient intake by patients. Nutrient density (ND) was calculated by standardizing the nutrient intake per 1,000 kcal based on the individual's intake amount. The index of nutritional quality (INQ), a comparison of the patient's nutrient intake against 12 nutrients, in which the required amounts are set by the Dietary Reference Intakes for Koreans, was analyzed. The dietary variety score (DVS) was calculated to examine the patient's dietary diversity. The food items consumed were categorized into five food groups (grain and starch, meat and poultry, vegetables, milk, fruits). The dietary diversity score (DDS) was investigated by giving a score of 1 point each to an intake of the minimum amount or higher out of a total score of 5.
NAR = nutrient intake of an individual/recommended dietary allowance (RDA) of the nutrient
MAR = sum of the nutrient adequacy ratio (NAR) for each nutrient/number of nutrients
INQ = amount of nutrients in 1,000 kcal/RDA in 1,000 kcal
Means and standard deviations were calculated using SPSS software program ver. 18.0 (SPSS, Inc. Chicago, IL, USA). Frequency per item, significance between discontinuous frequencies, and a comparison of the results between genders were analyzed using the frequency test, χ2-test, and the unpaired t-test, respectively. A P < 0.05 was considered significant.
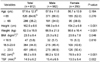
The general characteristics of the study targets are summarized in Table 1. Of the 812 patients, the male to female ratio was 69.2:30.8, indicating that male patients were more than twice females. The average age was 57.6 yr and 35.2% of the subjects were ≥ 65 yr. The average height, weight, and body mass index (BMI) were 162.5 cm, 62.0 kg, and 23.5 kg/m2, respectively, indicating significant differences between males and females. BMI distributions corresponding to underweight, normal, and overweight were 5.8%, 44.8%, and 49.4%, respectively, which indicated that most patients were of normal weight or were overweight prior to the operation. The average waist measurement and TSF were 85.2 cm and 14.9 mm. These measurements were significantly higher in males than those in females.
The results of the investigation into dietary habits and lifestyle are summarized in Table 2. A total of 42.1% and 50.1% of participants responded that their appetite was good and average before the operation, respectively. Approximately 56% responded that their meal intake was irregular. Although irregularity was more severe in females, no significant difference was observed between genders. As many as 46.6% responded that they skipped meals. The rate of skipping meals was 55.3% in males and 27.2% in females, indicating a significantly lower rate of skipping meals in females. Approximately 42% responded that they skipped breakfast, which was the meal most often skipped. For eating speed, 46.7% responded that their eating speed was fast. The habit of eating fast was reported by 53.2% of males and 32.0% of females. The rates of alcohol intake and smoking were significantly higher in males than those in females. Surprisingly, 88.8% responded that they did not exercise, which was similar in males and females.
As for taste preference, 41.3% of the respondents liked a salty taste. A large difference in taste preference was observed between genders, as 51.8% of males and 17.6% of females responded that they liked salty taste. The results of sweet taste preference by gender was the reverse of the above. A spicy taste was liked by 69.4% of males and 56.4% females, whereas 42.9% of males and 61.2% of females responded that they liked a sour taste. The preference for salty and spicy tastes was higher in males than those in females, whereas the preference for sweet and sour taste was higher in females than those in males. These results indicated significant differences in preferences for salty, spicy, sweet, and sour tastes between genders. About 39% of all respondents disliked a bitter taste, and no significant difference was observed between genders.
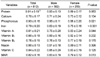
Nutrient intakes derived through the patient diet are analysis of all target are shown in Table 3. The average calorie intake was 1,949.1 kcal, and the intake amounts of protein, fat, sugar, and fiber were 75.3 g, 50.8 g, 282.3 g and 15.9 g, respectively. With the exception of fiber, the intake of nutrients was significantly higher in males. Intake of calcium, phosphorous, iron, and salt was significantly higher in males than those in females. The intake of potassium and zinc was higher in females than those in males. The intake of vitamin B1, vitamin B2, vitamin B6, niacin, and vitamin C was higher in males than those in females, whereas the intake of vitamin A, retinol, carotene, folic acid, and vitamin E was higher in females than those in males. Significantly different amounts of nutrients ingested between genders were seen for vitamin A, retinol, carotene, vitamin B1, vitamin B2, niacin, and folic acid. The average cholesterol intake was 235.1 mg, and males consumed a significantly higher amount than that in females.
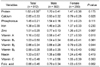
The results of comparing the NAR and MAR per nutrient are shown in Table 4. Most nutrients produced values of 0.7-0.9. NAR and MAR of phosphorous and iron were significantly higher in males than those in females. The values for vitamin A were lower in males than those in females. The MAR for males was 0.83 and for females it was 0.79, which was a significant difference. Nutrients ingested that were lower than the MAR were calcium, vitamin A, vitamin B1, and vitamin B2 for males and calcium, iron, and vitamin B2 for females.
ND and the INQ of male and female patients are shown in Tables 5 and 6. In males, there were no nutrients in which the ND was significantly higher. In females, the ND of fiber, calcium, potassium, zinc, vitamin A, retinol, carotene, vitamin B6, vitamin C, folic acid, and vitamin E were higher than those in males. No significant differences were observed between gender for the other nutrients. The INQ of zinc, vitamin A, vitamin B2, vitamin B6, and folic acid were higher in females than those in males. The INQ was higher in males than that in females for the other nutrients. Qualitatively significant differences were observed between males and females in terms of their calcium, zinc, vitamin A, vitamin B2, and folic acid intake. Six nutrients of males and three of females had an INQ ≤1.0. The ND of females was higher than that in males and the intake of nutrients more closely complied with the Korean average requirements in females.
The results of the DVS and DDS are shown in Table 7. The average DVS was 16.67. The DVS was 17.63 for females and 13.19 for males, indicating that females had more variety in their diet. The average DDS was 3.68. This result also indicated that females had a higher diversity of food in their diet than that of males.
The dietary habits, nutrient intake, and diet quality of patients with gastric cancer were investigated, and the results were compared between genders. According to the Nationwide Gastric Cancer Report 2009 conducted by the Korean Gastric Cancer Association [13], the male to female ratio for gastric cancer incidence has increased gradually from 1.67:1 in 1999 to 2.03:1 in 2009. The male to female ratio among target patients was 2.25:1, indicating that gastric cancer incidence is higher in males than that in females. The average age of a patients with gastric cancer reported by the Nationwide Gastric Cancer Report 2009 [13] was 58.9 yr, which was similar to the 57.6 yr found in the present study. A study conducted by Yang et al. [14] in 1993 reported that the average BMI of patients with gastric cancer was 20.6 kg/m2. It appears that the BMI of patients with gastric cancer has been increasing annually, as a recent study by Jo et al. [15] in 2010 reported that the average BMI was 23.3 kg/m2, which was almost the same as the BMI of 23.5 kg/m2 found in the present study. In Japan, where gastric cancer incidence is high, BMI has been increasing gradually as a result of improvement in overall physical condition of patients. The average BMI of Japanese patients before the operation increased from 20.8 kg/m2 in 1971 to 22.6 kg/m2 in 2001 [16]. BMI is a key factor among the nutritional evaluation indices and is widely used as an indicator to express the degree of obesity. Yoshikawa et al. [17] reported that the incidence of postoperative complications, and mean blood loss of an obese group were significantly higher than those of a normal group. Murphy et al. [18] reported that underweight patients experience delays in recovery of their nutritive condition after a surgical operation and that overweight patients with a BMI ≥ 30 kg/m2 have a high incidence of complications. Therefore, it is very important to maintain a normal BMI in patients with gastric cancer. In this study, 44.8% of patients had a normal weight and 49.4% were overweight or obese. The BMI distribution was similar in male and female patients.
A number of studies [8,9] have reported the relevance of an irregular meal schedule and the habit of eating fast on gastric cancer outbreak. In this study, the rates of irregular meal intake, skipping meals, and eating fast were 55.7%, 46.6% and 46.7%, respectively. As a whole, dietary habits of males were poorer than those of females. The increased risk of developing gastric cancer with alcohol intake is explained by the carcinogenic effects of acetaldehyde, a product of alcohol metabolism [19]. A cohort study by Steevens et al. [4] reported that consuming 30 g of alcohol daily is highly relevant to the incidence of gastric cancer and that there were differences between gender and the type of alcohol consumed. In the present study, 89.3% of males and 16.8% of females drank alcohol, indicating a large difference between genders. Smoking, one of the more important factors contributing to cancer deaths, is a widely known risk factor for gastric cancer. Smoking in the past or at present has strong relevance to gastric and esophageal cancer [4]. A study by Shin et al. [3] reported that the smoking rate among patients with gastric cancer was 63.8%, which was significantly different from the 49.7% in the control group. In our study, the overall smoking rate was 60.0% and there was a significant difference between genders. The smoking rate among males was 81.7% and that in females was 11.2%. A cohort study conducted in Europe [20], reported that physical activity, among dietary and health-related factors, had no relevance on the outbreak of gastric cancer. In the present study, only 11.2% of target patients exercised regularly and no difference between genders was found. It may be necessary to emphasize the importance of wholesome dietary habits to prevent gastric cancer, particularly among Korean males,.
Continued intake of salty and spicy flavors can irritate the stomach wall and increase the risk of developing gastric cancer. In particular, salty food increases the risk of gastric cancer in men more than that in women by 1.1 times [10]. In our study, 51.8% of males and 17.6% of females responded that they preferred a salty taste, indicating a large difference between genders. The preference for spicy taste was > 50% in both genders. A large number of studies have been conducted about gastric cancer and taste preferences. However, none have quantitatively investigated the amount of preferred type of food consumed, as affected by the preference for a particular taste, in relation to gastric cancer. It may be meaningful to pursue a study on the effect of limiting the intake of salty or spicy food items on gastric cancer incidence.
The average calorie intake of patients in this study was 1949.1 kcal. Males consumed approximately 500 kcal more than that of females. This was similar to the 2,076.0 kcal reported by Suh et al. [8] in Korea. Referring to the estimated calorie requirements of 2,200 kcal for males and 1,800 kcal for females aged 50-64 yr, as specified in the 2010 Dietary Reference Intakes for Koreans [21], a patient's daily caloric intake in this study was appropriate for males, but slightly lower for females; although the difference was not large. The average protein intake was 75.3 g, which was higher than the recommended intake of 50 g for males and 45 g for females. The average intake of calories and protein were similar compare to the 2008 Korean National Health and Nutrition Examination Survey [22]. The average fiber intake was 15.9 g. Fiber intake by females was significantly higher than that by males. Fiber intake was very low when compared to the recommended intake of 25 g for males and 20 g for females. Bravi et al. [23] reported that high fiber intake lowers gastric cancer incidence by 0.47 times. In particular, that study reported that insoluble and soluble fiber lower gastric cancer incidence by 0.39 and 0.50 times, respectively. They also reported differences according to the type of food item, such as vegetables, fruits and cereals, as a source of dietary fiber. Even if the nutritive conditions for minerals are satisfactory before an operation in patients with gastric cancer, their conditions may deteriorate, as overall nutritive condition become poorer after the operation due to insufficient meal intake, weight loss, and loss of appetite. In addition, intake of minerals through the diet can also change. Therefore, it is recommended that patients with gastric cancer and an inferior mineral balance before after an operation must be actively treated [24]. The total calcium intake was 476.2 mg, which was much lower than the recommended intake of 700 mg. Intake of phosphorous and iron were in excess of the recommendation. Additionally, the average intake of calcium, phosphorus, and iron were lower than the result of the 2008 Korean National Health and Nutrition Examination Survey [22]. The average amount of Na intake was 5937.4 mg per day. Male patients took in 6,488.5 mg per day which was higher than that of females, and was almost three times the recommended intake of 2000 mg. This result was also higher than the result of the 2008 Korean National Health and Nutrition Examination survey [22]. Therefore, lowering of Na in the diet must be strongly emphasized. Intake of sodium by both men and women was higher in comparison to the Korean average intake. Vitamin C, carotene, vitamin E, selenium, falconoid and leucopenia are widely known antioxidant nutrients that can help in preventing gastric cancer [18]. Compared to the 2010 Dietary Reference Intakes for Koreans [21] the intake of vitamin A, vitamin B, vitamin C, niacin, and vitamin E by the study patients was slightly insufficient. Carotene, falconoid, and vitamin E, contained in fresh vegetables and fruits, suppress carcinogenic substances and prevent them from converting to mutable substances in the gastro-intestinal tract. The intake of green and yellow vegetables by patients with gastric cancer in Korea is generally low [9]. Cholesterol has been tagged as a factor in the development of gastric cancer, colon cancer, rectal cancer, lung cancer, breast cancer, renal cancer, and gall bladder cancer [25]. In particular, as the level of cholesterol intake increases, so does the risk of prostate cancer [25]. In this study, cholesterol intake by males was 246.0 g, which was significantly different from the 198.5 g by females. These results were higher than the 191.9 mg reported by Suh et al. [8]. Eating is a process that supplies all nutrients needed by the body, and numerous diseases can be prevented by a balanced diet [26]. Effort must be exerted to achieve balanced intake of all nutrients to maintain satisfactory nutritive conditions after a surgical operation as well as to prevent gastric cancer. A balanced diet should include an appropriate amount of protein with fiber, vitamins and minerals from vegetables and fruits, and a limit on salt and cholesterol intake.
Various tools were used to analyze diet quality to evaluate the typical daily nutrition and the food intake status of patients diagnosed with gastric cancer prior to surgery. The MAR of subjects was measured as 0.82. Significant difference was found between men (0.83) and women (0.79). Nutrients below MAR included calcium and vitamins A, B1 and B2 for men and calcium, iron, and vitamin B2 for women. Phosphorus and iron were significantly higher in men than those in women, whereas vitamin A was low; thus, showing a difference according to nutrient. Nutrient density, which is a measure of nutrition intake per 1,000 kcal, reports individual calorie intake variations. According to the results, had presented a significantly lower intake of most nutrients, in particular anti-oxidative nutrients, such as fiber, zinc, vitamin, and folic acid than that of men. Thus, greater emphasis must be placed on intake of food products that possess high densities of the above nutrients. In addition, according to the INQ analysis, which was performed as a qualitative assessment of nutrients excluding the effect of calories, the INQ value was < 1 for calcium and vitamins B1 and B2 among women and calcium, zinc, and vitamins A, B2, B6, and folic acid among men. By comparing the nutrients that were significantly different by gender, it men had significantly higher INQ values in calcium and vitamin B2, whereas women showed significantly higher values in zinc, vitamin A, and folic acid. Based on these results, the quantitative increase in the diet and sufficient intake of deficient nutrients must be achieved in both men and women. The DVS and DDS were analyzed to assess diet diversity. DVS is based on the fact that various nutrients can be absorbed in meals as provided by a large number of food products. Previous results indicate that the number of absorbed food products and the diversity of food products are both significantly higher in women than those in men. Thus, the assessment of diet quality showed gender differences according to the tools used in this study and continuous research must be conducted to gain accurate results. Diet quality investigations have been conducted on a variety of targets, and Studies are being conducted on diverse diseases centering on metabolic syndrome [27], diabetes [28], atopic dermatitis [29], and Parkinson's disease [30].
The limitations of this study are as follows. This study surveyed preoperative daily dietary habits and nutrition intake of patients with gastric cancer who were in need of surgical treatment, and because there was no control group, it was difficult to draw definite conclusions on factors having a direct effect on gastric cancer occurrence. Nevertheless, as there have been few studies on the preoperative daily food intake of patients with gastric cancer in contrast to the various studies that have been conducted on postoperative nutritional condition, it is necessary to survey patient preoperative daily nutrition intake and evaluate their typical daily diet quality to develop a desirable postoperative dietary management program.
This study showed that male patients had more undesirable dietary habits and had more unbalanced nutrition intake than those of females. Accordingly, adequate nutrition management is necessary for both men and women to prevent cancer, and the importance of education on healthy dietary life should be emphasized particularly for men. In addition, evaluations should be made continuously to prevent poor preoperative nutrition from continuing postoperatively, and this effort should be supplemented by an analysis of various aspects of the case including age and pre/post/intra operative factors.
Figures and Tables
References
1. Jung KW, Park S, Kong HJ, Won YJ, Boo YK, Shin HR, Park EC, Lee JS. Cancer statistics in Korea: incidence, mortality and survival in 2006-2007. J Korean Med Sci. 2010. 25:1113–1121.

2. Forman D, Burley VJ. Gastric cancer: global pattern of the disease and an overview of environmental risk factors. Best Pract Res Clin Gastroenterol. 2006. 20:633–649.

3. Shin CM, Kim N, Yang HJ, Cho SI, Lee HS, Kim JS, Jung HC, Song IS. Stomach cancer risk in gastric cancer relatives: interaction between Helicobacter pylori infection and family history of gastric cancer for the risk of stomach cancer. J Clin Gastroenterol. 2010. 44:e34–e39.
4. Steevens J, Schouten LJ, Goldbohm RA, van den Brandt PA. Alcohol consumption, cigarette smoking and risk of subtypes of oesophageal and gastric cancer: a prospective cohort study. Gut. 2010. 59:39–48.

6. Navarro Silvera SA, Mayne ST, Risch HA, Gammon MD, Vaughan T, Chow WH, Dubin JA, Dubrow R, Schoenberg J, Stanford JL, West AB, Rotterdam H, Blot WJ. Principal component analysis of dietary and lifestyle patterns in relation to risk of subtypes of esophageal and gastric cancer. Ann Epidemiol. 2011. 21:543–550.

7. Peleteiro B, Lopes C, Figueiredo C, Lunet N. Salt intake and gastric cancer risk according to Helicobacter pylori infection, smoking, tumour site and histological type. Br J Cancer. 2011. 104:198–207.

8. Suh SW, Koo BK, Choi YH, Lee HS. The nutritional intakes of the stomach cancer patients in the Daegu and Gyeongbuk areas, Korea. Korean J Community Nutr. 2003. 8:202–219.
9. Youm PY, Kim SH. A case-control study on dietary and other factors related to stomach cancer incidence. Korean J Nutr. 1998. 31:62–71.
10. Kim J, Park S, Nam BH. Gastric cancer and salt preference: a population-based cohort study in Korea. Am J Clin Nutr. 2010. 91:1289–1293.

11. Pham TM, Fujino Y, Kikuchi S, Tamakoshi A, Matsuda S, Yoshimura T. Dietary patterns and risk of stomach cancer mortality: the Japan collaborative cohort study. Ann Epidemiol. 2010. 20:356–363.

12. Kim J, Kang M, Lee JS, Inoue M, Sasazuki S, Tsugane S. Fermented and non-fermented soy food consumption and gastric cancer in Japanese and Korean populations: a meta-analysis of observational studies. Cancer Sci. 2011. 102:231–244.

13. Korean Gastric Cancer Association Information Committee. Nationwide Survey of Gastric Cancer in Korea. 2009. Seoul:
14. Yang EJ, Kim WY. A study on dietary factors related to the incidence of stomach cancer and colon cancer in Korean. Korean J Nutr. 1993. 26:603–614.
15. Jo DH, Jeong O, Sun JW, Jeong MR, Ryu SY, Park YK. Feasibility study of early oral intake after gastrectomy for gastric carcinoma. J Gastric Cancer. 2011. 11:101–108.

16. Kubo M, Sano T, Fukagawa T, Katai H, Sasako M. Increasing body mass index in Japanese patients with gastric cancer. Gastric Cancer. 2005. 8:39–41.

17. Yoshikawa K, Shimada M, Kurita N, Iwata T, Nishioka M, Morimoto S, Miyatani T, Komatsu M, Mikami C, Kashihara H. Visceral fat area is superior to body mass index as a predictive factor for risk with laparoscopy-assisted gastrectomy for gastric cancer. Surg Endosc. 2011. 25:3825–3830.

18. Murphy PM, Blackshaw GR, Paris HJ, Edwards P, Barry JD, Lewis WG. Prospective evaluation of nutritional status related to body mass indices and outcomes after modified D2 gastrectomy for carcinoma. Clin Nutr. 2004. 23:477–483.

19. Yoon EY. Dietary risk factors of gastric cancer & nutrition intervention. Korean J Community Nutr. 2004. 9:353–365.
20. Huerta JM, Navarro C, Chirlaque MD, Tormo MJ, Steindorf K, Buckland G, Carneiro F, Johnsen NF, Overvad K, Stegger J, Tjønneland A, Boutron-Ruault MC, Clavel-Chapelon F, Morois S, Boeing H, Kaaks R, Rohrmann S, Vigl M, Lagiou P, Trichopoulos D, Trichopoulou A, Bas Bueno-de-Mesquita H, Monninkhof EM, Numans ME, Peeters PH, Mattiello A, Pala V, Palli D, Tumino R, Vineis P, Agudo A, Ardanaz E, Arriola L, Molina-Montes E, Rodríguez L, Lindkvist B, Manjer J, Stenling R, Lund E, Crowe FL, Key TJ, Khaw KT, Wareham NJ, Jenab M, Norat T, Romaguera D, Riboli E, González CA. Prospective study of physical activity and risk of primary adenocarcinomas of the oesophagus and stomach in the EPIC (European Prospective Investigation into Cancer and nutrition) cohort. Cancer Causes Control. 2010. 21:657–669.

21. The Korean Nutrition Society. Dietary Reference Intakes for Koreans. 2010. 1st revision. Seoul:
22. Korea Health Industry Development Institute. National Food & Nutrition Statics: Based on 2008 Korean National Health and Nutrition Examination Survey. 2010. Cheongwon:
23. Bravi F, Scotti L, Bosetti C, Bertuccio P, Negri E, La Vecchia C. Dietary fiber and stomach cancer risk: a case-control study from Italy. Cancer Causes Control. 2009. 20:847–853.

24. Kang I, Kim YS, Kim C. Mineral deficiency in patients who have undergone gastrectomy. Nutrition. 2007. 23:318–322.

25. Hu J, La Vecchia C, de Groh M, Negri E, Morrison H, Mery L. Canadian Cancer Registries Epidemiology Research Group. Dietary cholesterol intake and cancer. Ann Oncol. 2012. 23:491–500.

26. Azadbakht L, Mirmiran P, Azizi F. Dietary diversity score is favorably associated with the metabolic syndrome in Tehranian adults. Int J Obes (Lond). 2005. 29:1361–1367.

27. Kim M, Kim J, Bae W, Kim S, Lee Y, Na W, Sohn C. Relationship between nutrients intakes, dietary quality, and serum concentrations of inflammatory markers in metabolic syndrome patients. Korean J Community Nutr. 2011. 16:51–61.

28. Lim HJ, Woo MH, Moon SK, Choue R. Comparative study of diabetes mellitus patients with cerebral infarction or without cerebral infarction -focused on nutrient intakes and dietary quality-. Korean J Nutr. 2008. 41:621–633.
29. Kim BS, Kim YY, Park JH, Kim NI, Choue RW. Effects of medical nutrition therapy on dietary quality, plasma fatty acid composition and immune parameters in atopic dermatitis patients. Korean J Community Nutr. 2008. 13:80–90.
30. Lee JY, An TB, Jeon BS, Kim YY, Choue RW. Nutrients intake and dietary quality of Korean Parkinson's disease patients according to the duration of disease. Korean J Community Nutr. 2008. 13:582–591.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download