Introduction
Vitamin D deficiency has been associated with the prevalence of cardiovascular disease (CVD), suggesting that vitamin D does not participate solely in "classical" calcium metabolism in bone, the intestines, and the kidney [
1,
2]. Indeed, vitamin D receptors are found in most tissues, suggesting that vitamin D may be involved in energy, glucose, and/or lipid metabolism. Both the consumption of vitamin D from foods containing and/or fortified with vitamin D3 (cholecalciferol) and sun light exposure increases vitamin D in the body [
1,
2]. Serum 25-hydroxyvitamin D (25(OH)D), the major storage form of vitamin D, is formed in the liver. Serum level of 25(OH)D is a clinical indicator of overall vitamin D3 status. [
3]. Previous studies in Caucasians have shown that serum levels of 25(OH)D are inversely related to hypertension, diabetes, carotid atherosclerosis, myocardial infarction, congestive heart failure, stroke, microalbuminurea, and kidney dysfunction; however, neither the role of vitamin D deficiency in the development of CVD nor the practical recommendation for its supplementation to prevent CVD has been established. In addition, the effects of ethnicity on vitamin D status and CVD prevalence have not been well studied [
1,
4].
Ethnicity is likely to contribute to CVD, as evidenced by the different pattern of CVD in Asians and Caucasians [
5-
7]. Furthermore, the means by which CVD causes mortality differs between Caucasians and Koreans; in Caucasians, atherosclerotic coronary artery and cerebrovascular diseases are predominant whereas in Koreans, hypertensive heart disease and stroke are responsible for the majority of CVD mortality [
6,
7]. Renzaho et al. [
8] showed that ethnic minorities including Asians had significantly higher rates of vitamin D insufficiency than their Caucasian counterparts and also demonstrated a relationship between vitamin D deficiency and obesity, type 2 diabetes and CVD. In an analysis of data from the Third National Health and Nutrition Survey in the US (1988-1994), Kendrick et al. [
4] also reported that serum 25(OH)D levels were lower in non-Hispanic blacks, Mexican Americans, and other races than in non-Hispanic whites. Since Asians were included in the "other race" category rather than constituting a separate category in the Third National Health and Nutrition Survey, Asians may have a greater risk of vitamin D deficiency. The effects of vitamin D deficiency on CVD prevalence need to be examined in nationwide studies of Asians, including Koreans. The Korean National Health and Nutrition Examination Survey (KNHANES-2008-2009) indicates that the prevalence of CVD is not associated with low serum 25(OH)D levels in the total population. We reexamined the data by stratifying groups according to serum 25(OH)D levels along with the risk of CVD. Additionally, Kim et al. [
9] reported that vitamin D deficiency was directly proportional to the incidence of metabolic syndromes, including obesity, diabetes, and hypertension, in subjects > 40 years old in Chungju, Korea. Thus, we hypothesized that low serum 25(OH)D in adults ≥ 50 increases the risk of CVD. We studied the association of serum 25(OH)D deficiency and clinical CVD syndromes in this age group, including angina, myocardial infarction, and stroke, using the KNHANES 2008-2009 data.
Go to :

Subjects and Methods
Design and data collection
This study was based on cross-sectional data obtained from the KNHANES 2008-2009, representing the second and third years of the KNHANES IV (2007-2009), which used a rolling sampling design that involved a complex, stratified, multistage, probability-cluster survey of a representative sample of the noninstitutionalized civilian population in South Korea. Detailed information on the design of the survey has been provided previously [
10]. To summarize, the survey compiled its data through health interviews, physical examinations, and an examination of the nutritional status of Korean adults.
Since women ≥ 50 years of age are generally post-menopausal and men also experience major physiological changes from 50 years of age, the present analysis was restricted to participants ≥ 50 years old who completed the health examination survey and for whom vitamin D measurements (serum 25(OH)D levels) were available (n = 6,045). After the exclusion of individuals with liver cirrhosis or other chronic liver or renal diseases, the final sample group consisted of 5,559 participants who were divided into groups depending on vitamin D serum levels: < 25 nmol/l (severe deficiency), 25-49 nmol/l (deficiency), 50-74 nmol/l (moderate deficiency), and ≥ 75 nmol/l (sufficient) [
11]. Since serum 25(OH)D levels were relatively low in Koreans, subjects over 75 nmol/l of serum 25(OH)D levels could not be divided further.
Information on age, education, history of cigarette use, and alcohol intake was collected during the health interview. Height and weight measurements were taken with the participants wearing light clothing and no shoes. Body mass index (BMI) was calculated as weight (in kg) divided by the square of height (in m), and was categorized into three groups: lean (BMI < 18.5), normal (18.5 ≤ BMI < 25), and obese (BMI ≥ 25). The participants were further divided into six groups according to age. Residential areas were categorized as urban (administrative divisions of a city) or rural (not classified as administrative divisions of a city). Regional areas were Seoul, Incheon/Kyunggi/Kangwon, Daejeon/Choongchung, Daegu/Kyungbuk, Busan/Kyungnam, and Kwangju/Honam/Jeju. Education level was categorized into three groups: below high school, high school, and college or higher. Cigarette use was divided into three categories: current smoker, past smoker, and no history of cigarette use, which correlated to fewer than 100 cigarettes ever smoked. Subjects who had smoked 100 or more cigarettes were classified as past or current smokers, based on current use. Alcohol consumption was assessed using subjects' drinking behavior during the month prior to the interview, including average frequency (days per month) of alcoholic beverage consumption and amount (in ml) of alcohol ingested on a single occasion. The responses were converted into the amount of pure alcohol (in g) consumed per day, which was categorized into four groups: non-drinker, light drinker (1-15 g), moderate drinker (16-30 g), and heavy drinker (> 30 g).
Regular walking was defined as walking for ≥ 30 min at a time at least five times per week, either indoors or outdoors. Regular exercise was defined as participating in moderate exercise (slow swimming, team tennis playing, volleyball, occupational or recreational activity carrying light objects) on a regular basis for ≥ 30 min at a time at least five times per week, or in vigorous exercise (running, climbing, rapid cycling, rapid swimming, football, basketball, jumping rope, squash, singles tennis playing, occupational or recreational activity carrying heavy objects) for ≥ 20 min at a time at least three times per week. Diabetes mellitus (DM) was defined as fasting glucose of ≥ 126 mg/dl, current use of anti-diabetic medications, or self-reported physician diagnosis of DM. Insulin resistance was determined using the homeostasis model assessment (HOMA) estimate of insulin resistance [HOMA-IR = fasting insulin (µIU/ml) × fasting glucose (mM) / 22.5] and fasting insulin levels [
12].
Cardiovascular disease
CVD was defined as a history of angina pectoris, myocardial infarction, or stroke, which was determined by subject affirmation of any of these in the health questionnaire. Each condition was inquired about separately.
Clinical laboratory tests
Fasting blood samples for clinical laboratory tests in the KNHANES were taken in the morning after an ≥ 8-h fast. Blood samples were centrifuged, aliquoted, and frozen at -70℃ on site. The frozen plasma and serum samples were transported on dry ice to the designated central laboratory of Neodin Medical Institute (NMI), a laboratory certified by the Korean Ministry of Health and Welfare in Seoul, Korea. Blood samples were analyzed within 24 h after transport. Serum 25(OH)D levels, an indicator of V-D status, were measured with a gamma counter (1470 Wizard; Perkin-Elmer, (San Jose, CA, USA) using a radioimmunoassay kit (DiaSorin, Stillwater, MN, USA) [
13]. Plasma glucose levels were measured using an autoanalyzer (Hitachi 7600; Hitachi, Tokyo, Japan).
Statistical analysis
Statistical analyses were performed using the SAS software (ver. 9.22; SAS Institute, Cary, NC, USA) and SUDAAN (release 10.0; Research Triangle Institute, Research Triangle Park, NC, USA), a software package that incorporated sample weights and adjusted analyses for the complex sample design of the survey. Survey sample weights were used in all analyses to produce estimates that were representative of the noninstitutionalized civilian Korean population.
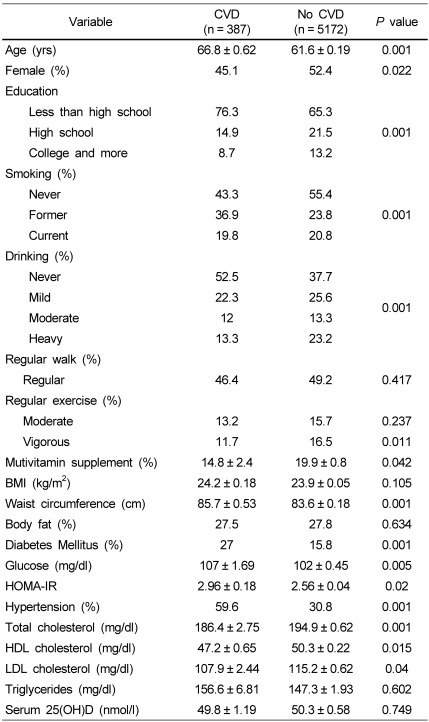
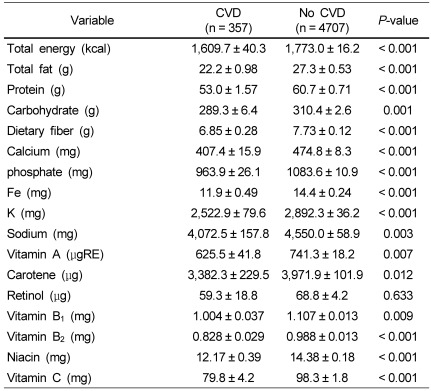
The descriptive statistics of participants were obtained by determining frequency distributions of categorical data and the weighted means and standard errors of continuous variables, such as age, BMI, total cholesterol, high-density lipoprotein (HDL) cholesterol, triglyceride, and serum 25(OH)D. Significant differences in categorical and continuous variables between the CVD and non-CVD groups were analyzed using the chi-squared test and Student's t-test.
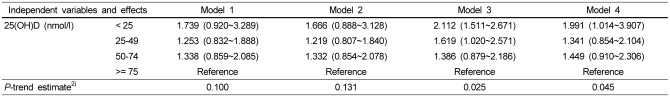
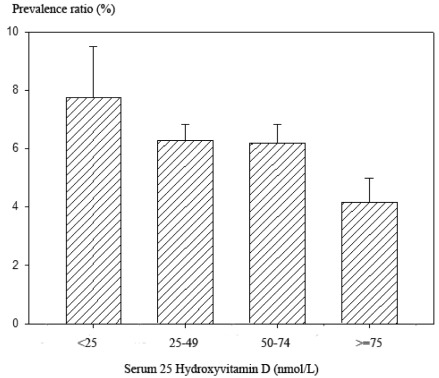
Next, odds ratios (ORs) and 95% confidence intervals (CIs) for having CVD were calculated using serum 25(OH)D as a categorical variable (< 25 nmol/l, 25-49 nmol/l, 50-74 nmol/l, ≥ 75 nmol/l), while controlling for covariates (model 1: age, gender, BMI; model 2: model 1 + diabetic status; model 3: model 2 + education level, residence location, region, caloric intake; model 4: model 3 + smoking, drinking, regular exercise, regular walking) using the Proc Rlogist function to incorporate the sample weights and adjust the analyses for the complex sample design of the survey. Covariate-adjusted prevalence ratios were calculated using model 4 data and their difference was compared among serum 25(OH)D categories. Additionally, analysis of covariance (ANCOVA) was used to compare the risk factors contributing to CVD among the four serum 25(OH)D categories from model 4. Multiple comparisons among the groups were performed by the contrast test in comparison with the reference group (the lowest 25(OH)D group).
Go to :

Discussion
The present study revealed that serum 25(OH)D levels (average, 50 nmol/l) were relatively low in subjects aged ≥ 50 years, in comparison with the total population (75 nmol/l) of the US Third National Health and Nutrition Examination Survey [
4]. Furthermore, serum 25(OH)D levels were much lower in all age groups of the Korean population than in the US population [
4]. Fortunately, the prevalence of CVD (7.9%) was much lower than that in other countries: for example, 23.5% of the Portuguese population aged > 40 years had CVD, as did 36% of the US population aged > 45 years [
15,
16]. Unlike other studies, we found that, without adjusting parameters, serum 25(OH)D levels in Koreans aged ≥ 50 years did not differ significantly between the CVD and non-CVD groups [
4,
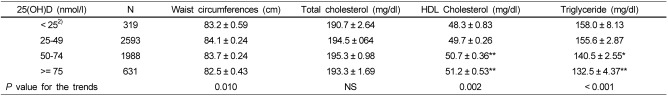
10]. However, after adjusting for age, gender, BMI, education level, residence location, region, and energy intake, subjects in the lowest category (< 25 nmol/l) of serum 25(OH)D levels had a higher prevalence of CVD, about two-fold higher than subjects in the highest category (≥ 75 nmol/l). Additionally, subjects in the lowest category had additional risk factors for CVD, such as higher waist circumference, fasting glucose and triglyceride levels, and lower HDL cholesterol levels, compared with those in the highest category. These findings suggest that serum 25(OH)D levels may be clinically relevant to the risk of CVD in the older Korean population.
There has been much discussion about the definition of vitamin D deficiency. Most researchers have agreed that a serum 25(OH)D concentration of < 50 nmol/l is an indicator of vitamin D deficiency and a concentration of 51-74 nmol/l indicates vitamin D insufficiency [
1,
3,
11]. In the present study, most older Koreans were considered vitamin D-deficient or -insufficient on the basis of these serum 25(OH)D levels: 52.8%, 35.8%, and 11.4% of the subjects were vitamin D-deficient, vitamin D-insufficient, and sufficient, respectively. This finding may be related to the limited food sources of vitamin D. Most Koreans have low consumption of vitamin D-rich foods, such as fatty fish (300 IU/100 g), eggs (25 IU/egg), and liver (30 IU/100 g) [
17]. Additionally, in Korea, most milk products are not fortified with vitamin D, whereas nearly all milk and milk products are fortified with vitamin D3 in many countries, including the USA. Vitamin D3 is inefficiently synthesized in individuals with dark skin and many Koreans, especially women, use sunscreen to protect against further skin darkening [
18]. However, sunscreen of SPF15 reduces vitamin D3 production by 99% [
18]. Older Koreans also typically engage in less outdoor physical activity than do younger people [
7]. Thus, Koreans, especially the older population, are at increased risk of vitamin D deficiency. KNHANES did not calculate vitamin D intake and few studies have investigated this intake in the Korean population because the computer program typically used in Korea for nutrient analysis does not include the vitamin D contents of the listed foods. Heo et al. [
19] investigated vitamin D intakes in post-menopausal women aged > 50 years (n = 189) and found that daily vitamin D intakes were 6.07 µg (60% of the Korean Dietary Reference Intake). Additionally, the subjects had < 60 min of daily sun exposure. Thus, most post-menopausal Korean women had vitamin D deficiency. Lee et al. [
20] have shown that post-menopausal women (n = 322) have an average serum 25(OH)D level of 40 ± 18 nmol/l, indicating vitamin D deficiency. These recent studies indicate that post-menopausal Korean women may have vitamin D deficiency due to low consumption of vitamin D-rich foods and low sunlight exposure. Thus, it is important to promote regular consumption of vitamin D3-fortified foods and to encourage regular outdoor activity.
Several studies have found an association between serum 25(OH)D levels and CVD [
4,
13,
21,
22]. The Framingham Offspring Study revealed that low serum 25(OH)D (< 38 nmol/l) was independently associated with an increased incidence of CVD in Caucasians during a 5.4-year follow-up period [
21]. Additionally, European studies have shown that serum 25(OH)D levels are inversely associated with the prevalence of CVD and carotid intima-medial thickening in patients with type 2 DM [
22]. Furthermore, the Third National Health and Nutrition Examination Survey in the US reported that serum 25(OH)D levels of < 75 nmol/l were associated with an increased prevalence of CVD in participants, including those of different ethnic backgrounds [
4]. However, that study included Asians in the "other race" category rather than designating them as a separate group. The present study showed that subjects in the lowest category of serum 25(OH)D levels had nearly double the prevalence of CVD than did those in the highest category when adjusting age, gender, BMI, diabetic status, education levels, residence location, region, and caloric intake. However, differences were evident between the Caucasian and Korean populations: serum 25(OH)D levels were lower in Koreans than in Caucasians and the prevalence of CVD did not differ significantly in the Korean population when vitamin D deficiency was defined as a serum 25(OH)D level of < 50 nmol/l [
4].
The present study revealed that the lowest serum 25(OH)D category was associated with other risk factors for CVD, such as waist circumference, BMI, and serum HDL cholesterol, triglyceride, and glucose levels. Thus, the lower level of serum 25(OH)D that is a risk factor for developing CVD can be defined as 25 nmol/l in the older Korean population. The reason for this lower limit for the risk of developing CVD may be due to differences between Caucasians and Koreans in the pathophysiology of CVD. However, the prevalence of CVD and vitamin D deficiency may increase markedly in Korea due to changes in dietary patterns, such as trends of increasing fat and cholesterol intake and decreasing physical activity. Therefore, the pathophysiology of CVD in Koreans may begin to resemble that seen in Caucasians more closely due to lifestyle changes. Thus, vitamin D intake and light exposure need to be increased.
The present study has a few limitations. First, since this study was cross-sectional, the ability to establish a causal relationship between serum 25(OH)D levels and the prevalence of CVD was limited. Second, incidence of CVD could incorporate misclassification bias because they were based on participants' reports of their physicians' diagnosis. Third, the participants may have made efforts to reduce risk factors to prevent symptoms associated with CVD. For example, the intake of energy and all nutrients were lower in the CVD group than the non-CVD group, presumably because the participants who had been diagnosed with CVD had reduced their caloric intake to control body weight. Fourth, data on sun exposure and dietary vitamin D intake were not available. Although the present study has limitations, this is the first reported study to determine the relationship between the prevalence of CVD and vitamin D deficiency in an older Asian population. Future studies are needed to determine whether the correction of vitamin D deficiency could contribute to CVD prevention, and to identify potential mechanisms of vitamin D replacement for reducing the development of CVD.
In summary, the present study revealed that severe vitamin D deficiency, defined as serum 25(OH)D < 25 nmol/l, was positively associated with the prevalence of CVD in a representative sample of the adult Korean population, independent of age, BMI, diabetic status, education level, residence location and region, smoking, drinking, and regular exercise such as walking. The results of this study suggest that increasing serum 25(OH)D to the sufficient level (≥ 75 nmol/l) may reduce the risk of CVD, and that vitamin D replacement in persons with vitamin D deficiency may decrease their risk of CVD.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download