Abstract
Compliance with food group and nutrient recommendations, and self-efficacy, stage of change, perceived barriers and benefits for healthy eating were assessed among a convenience sample of college students majoring in health-related disciplines. Dietary and psychosocial data were collected using three-day food records and scales, respectively. Means (SD), frequencies, and percents were calculated on all data, and logistic regressions were used to determine whether any of the psychosocial correlates predicted the stage of change for healthy eating. Noncompliance with food group recommendations ranged from 53% for the meat/meat alternates group to 93% for the vegetables/juice group, whereas noncompliance with nutrient recommendations ranged from 26% for cholesterol to 99% for potassium. A majority of students (57%) self-classified in the preaction and 40% in the action stages of change for eating healthy. The students' self-efficacy to eat healthy was highest in positive/social situations and lowest when experiencing emotional upset. The most important perceived barrier to healthy eating was that friends/roommates do not like to eat healthy foods, and the most important perceived benefit was that eating healthy foods provides the body with adequate nutrients. The difficult/inconvenient self-efficacy subscale predicted the stage of change for healthy eating. These students would benefit from interactive learning opportunities that teach how to purchase and prepare more whole grain foods, fruits, and vegetables, enhance their self-efficacy for making healthy food choices when experiencing negative emotions, and overcome perceived barriers to healthy eating.
Overweight, defined as a body mass index (BMI) between 25.0 to 29.9 kg/m2 and obesity, defined as a BMI of 30.0 kg/m2 or greater, are public health problems in the United States [1]. Ample epidemiologic and clinical evidence has identified excess adiposity as a strong risk factor for coronary heart disease, hypertension, strokes, type 2 diabetes mellitus, and some types of cancers [2]. Among the population groups showing a steady increase in the prevalence of overweight/obesity are college students [3]. Currently, an estimated 11.8 million individuals aged 18 to 24 are enrolled in US colleges and universities [4], and it has been estimated that 26% of Caucasian and 50% of African-American college students are either overweight or obese [3]. Moreover, an estimated 33% of U.S. college students have a total cholesterol level above 200 mg/dL, approximately 20% have HDL cholesterol concentrations below 40 mg/dL, and another 15% to 21% have prehypertension [5].
In addition to the increasing rates of overweight/obesity and risk factors for cardiovascular disease (CVD) reported for college students, this population has long been regarded as nutritionally vulnerable because of their poor eating habits, which include meal skipping, unsound weight reduction strategies, regular use of alcohol, and frequent consumption of fast foods that are high in fats, cholesterol, salt, sugar, and calories, and low in fiber, calcium, iron, vitamin A and carotenoids [6-8]. In this regard, Rosette et al. [9] noted a reduction in healthful food selection and increased body weights among a sample of college students.
The United States Departments of Agriculture (USDA) and Health and Human Services (DHHS) jointly sponsor the MyPyramid interactive website [10] to assist consumers in making healthy food choices to reduce their risk of chronic disease. This website features 12 eating plans ranging from 1,200 to 3,200 daily calories, allowing consumers to tailor their energy intakes to their level of physical activity. Specific amounts are recommended from the five food groups, i.e., grain/cereal, dairy, meat/meat alternates, fruit/juice, and vegetable/juice, and from the fats/oils/sweets group (referred to as discretionary calories). These recommended amounts are tailored to the selected eating plan.
The Dietary Reference Intakes (DRIs) are sets of nutrient standards developed jointly by the United States Institute of Medicine (IOM) and Health Canada to assess nutrient intakes and plan diets for individuals and groups [11-16]. Like the MyPyramid website, the orientation of the DRIs is toward risk reduction rather than disease management. Currently, there are DRIs for the nutrients that promote bone health [11], the B complex vitamins and choline [12], the antioxidant nutrients [13]. other vitamins and minerals [14]. energy and the macronutrients [15], and water and the electrolytes [16]. One theoretical framework that has been used extensively to identify psychosocial correlates associated with dietary compliance is the transtheoretical model™ [17,18].
The TM consists of four dimensions, i.e., the stages of change, the processes of change, situational self-efficacy, and decisional balance. The stages of change represent the temporal, motivational, and consistency constructs of behavior change. These stages are pre-contemplation (no thought is given to adopting a healthy behavior within the next six months), contemplation (serious consideration is given to adopting a healthy behavior within the next six months), preparation (the decision is made to adopt a healthy behavior within the next 30 days), action (the healthy behavior has been practiced for less than six months, and it requires considerable effort to maintain), maintenance (the healthy behavior has been practiced for six months or longer, and it requires less effort to maintain), and termination (the healthy behavior has become automatic). The first three stages are frequently categorized as the preaction and the latter three as the action stages [18,19]. The TM hypothesizes that individuals can transition from the preaction to the action stages through cognitive and behavioral processes of change.
The cognitive processes of the TM focus on gathering information regarding the unhealthy behavior, leading to an attitude change conducive to a positive behavior change. The behavioral processes involve adopting strategies that facilitate the replacement of unhealthy behaviors with healthy ones. The situational self-efficacy dimension measures the degree of confidence toward undertaking healthy behaviors under a variety of circumstances, and the decisional balance component assesses the perceived barriers and benefits associated with the adoption of healthy behavior.
Ample literature is currently available regarding the food choices of the general college student population [6-9]. However, little information is available on this topic in regard to the subgroup of college students majoring in health-related fields, or on the psychosocial correlates associated with food selection among these students. Therefore, the objectives of this descriptive, exploratory study were to assess compliance with the MyPyramid and DRI recommendations among a convenience sample of college students majoring in health-related disciplines, and to identify correlates from the TM that predict their stage of change for healthy eating. This information would prove useful for the design of nutrition education interventions tailored to the needs of specific groups of college students who aspire to work as health professionals, e.g. males vs. females, younger vs. older students, or African-Americans vs. Caucasians. Evidence suggests that such tailored learning opportunities offered during the college years can motivate young people to adopt healthy eating habits that can track through adulthood [18], and consuming healthy diets during adulthood would make it easier to model healthy eating throughout their careers for their clients, families, and co-workers.
Convenience sampling was used to recruit students from three sections of an introductory nutrition course at a university in the Southeastern United States. The selected course is required of health-related majors (e.g., dietetics, nursing science, exercise physiology, athletic training, worksite wellness, and community health). The objectives of the study and the stipulations of informed consent were explained to the students orally and in a cover letter which they signed if they agreed to participate. Anonymity was assured by collecting these letters separately and placing them in a sealed envelope. Confidentiality was protected by filing the cover letters and completed questionnaires in a locked filing cabinet in the office of one of the investigators. Students were offered 10 extra credit course points for participating, and an alternative assignment of equal point value was offered to nonparticipants. This study was approved by the Committee on Human Research in the Behavioral Sciences at the study site.
An anonymous, self-administered questionnaire developed by the researchers was administered in class during the second week of the semester, before teaching about MyPyramid and DRI recommendations. Information was collected regarding gender, race/ethnicity, year in school, academic major, on- or off-campus residence, self-reported height and weight (for calculating BMI), stage of change and self-efficacy for eating healthy, and perceived barriers and benefits associated with healthy eating. The students also indicated whether they had previously taken a college-level nutrition course, and identified, from a list, the sources of nutrition information they relied on most heavily.
The students' stage of change for eating healthy was assessed with a single item based on Prochaska's descriptors for the preaction and action stages [17]. A definition for the term "healthy diet" was provided immediately above the response options to guide the students in selecting the stage that most accurately reflected their readiness to eat a healthy diet. A healthy diet was defined as one that: includes a variety and an adequate amount of fruits, vegetables, grains, dairy products, and protein-rich foods; provides enough calories to maintain a healthy weight; is moderate in total fat, and low in saturated fat, trans fat, and cholesterol; provides adequate amounts of dietary fiber; is low in added sugars; is not high in salt; contains adequate amounts of potassium; and contains moderate or no alcohol [10].
The students' self-efficacy with regard to consuming a healthy diet was assessed using modified versions of Ounpuu, Woolcott, and Rossi's situational self-efficacy subscales [18]. The negative/affective subscale (seven items) focuses on emotionally upsetting circumstances, the positive/social subscale (five items) focuses on celebratory situations, and the difficult/inconvenient subscale (six items) focuses on circumstances in which accessing healthy foods is challenging. Each item was rated on a five-point scale where 1 meant "not at all confident" and 5 meant "very confident." The Cronbach alpha coefficients for the present sample were 0.93 for the negative/affective, 0.81 for the positive/social, and 0.80 for the difficult/inconvenient subscale. The students also rated the importance of 11 potential barriers and six potential benefits to eating healthy, compiled from a review of pertinent literature [6-10], on a five-point scale where 1 meant "not at all important" and 5 meant "very important." Six of the barriers focused on practical concerns and five on internal cues, whereas the five benefits focused on adequate nutrient intakes for health maintenance. The Cronbach alpha coefficients for the two barriers subscales were 0.61 and 0.79, respectively, and the coefficient for the benefits subscale was 0.72.
The demographic and psychosocial questionnaire was pilot tested at the study site with six students who did not participate in the final study, and was revised on the basis of their input. Face and content validity of all measures were determined by a panel of three nutrition professors who were experienced with questionnaire design and familiar with the TM.
Compliance with MyPyramid and DRI recommendations was also assessed during the second week of the semester to minimize an expectation bias. The students completed a three-day food record that reported the types and amounts of all foods (including snacks), beverages, and dietary supplements consumed, and entered their data into the Diet Analysis Plus software (Thomson/Wadsworth, version 8.0, 2007). In-class instruction was offered regarding data entry, how to calculate their three-day mean intakes of each food group, total and saturated fat, cholesterol, fiber, sodium, potassium, and calcium, and how to determine their compliance with food groups and DRI recommendations from their computer-generated reports. The extent of compliance with the 2005 Dietary Guidelines for Americans and the Institute of Medicine reports was expressed as a percentage of the recommendations [10-16]. The three-day computer-generated compliance reports were subsequently used by the investigators to calculate aggregate food group and nutrient intakes and compliance with dietary recommendations.
Data were analyzed using SPSS for Windows (Version 16.0, SPSS, Inc., Chicago, IL, 2007). Frequency counts and percentages were obtained on demographic and stage-of-change data, and means (SD) were obtained on self-efficacy, barriers, and benefits data. As recommended by the DRI committee [11-16], the percentages of students who were noncompliant with food group and nutrient recommendations are reported. Chi-square analysis was performed to compare the proportion of students who were compliant with MyPyramid and DRI recommendations based on selected demographic variables. Logistic regression modeling was performed to determine whether any of the psychosocial correlates from the TM predicted the self-classified stage of change for healthy eating. The level of statistical significance was set at P < 0.05.
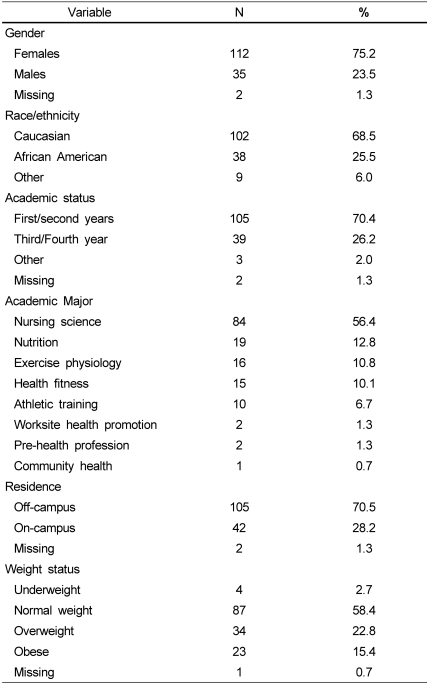
The demographic and psychosocial questionnaire was completed by 149 students. The students' mean age was 20.9 (SD 5.5) years. Other demographics are reported in Table 1. In summary, three-fourths of the students were females, and approximately 70% were Caucasian, first/second-year students, and off-campus residents. Additionally, approximately half the students had previously taken a college-level nutrition course, and the most frequently used sources of nutrition information were personal trainers, the Internet, and athletic coaches.
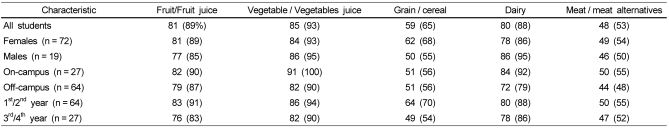
Computer-generated food group and nutrient intake reports were received from 91 students (61% of the 149 students who completed the demographic and psychosocial questionnaire). Data showing compliance with food group recommendations are presented in Table 2.
Approximately 53% of the students were noncompliant with the meat/meat alternates recommendation (mean ± SD = 5.9 ± 3.8 servings/day, range 0 to 20.4 servings/day), 65% did not meet the recommendation for the grain/cereal group (mean ± SD = 6.0 ± 3.7 servings/day, range 0 to 26.4 servings/day), 88% were noncompliant with the dairy recommendation (mean ± SD = 1.6 ± 1.4 servings/day, range 0 to 10.6 servings/day), 89% did not meet the recommendation for the fruit/juice group (mean ± SD = 0.8 ± 0.9 servings/day, range 0 to 3.7 servings/day), and 93% were noncompliant with the vegetable/juice recommendation (mean ± SD = 1.0 ± 1.0 servings/day, range 0 to 5.9 servings/day). Only 1% of the students met the recommendations for all food groups.
Adherence to food group recommendations based on gender revealed that 50% of the males and 54% of the females were noncompliant with the recommendations for the meat/meat alternates group, 55% of the males and 68% of the females were noncompliant with the grain/cereal recommendation, 95% of the males and 86% of the females were noncompliant with the dairy recommendation, 85% of the males and 89% of the females did not meet the recommendation for the fruit/juice group, and 95% of the males and 93% of the females were noncompliant with the vegetable/juice recommendation. None of these differences were statistically significant. Among the females, 99% were noncompliant with the recommendations for all five food groups, while among the males 100% were noncompliant with the recommendations for all five food groups.
Greater proportions of on-campus than off-campus residents were noncompliant with the fruit/juice (90% vs. 87%), vegetable/juice (100% vs. 90%), and fats/oils/sweeteners (21% vs. 17%) recommendations. Noncompliance with the grain/cereal recommendation was detected in 56% of the on and off-campus residents; fewer off-campus residents met the dairy recommendation (92% vs. 79%) and the meat/meat alternates recommendation (55% vs. 48%). The only statistically significant difference was for the vegetable/juice group (P = 0.002).
Greater proportions of first/second- than third/fourth-year students did not meet the recommendations for the fruit/juice (91% vs. 83%), vegetable/juice (94% vs. 90%), grain/cereal (70% vs. 54%), and dairy (88% vs. 86%) groups. Additionally, greater proportions of the third/fourth-year than the first/second-year students were noncompliant with the recommendations for the meat/meat alternates group (55% vs. 52%) and for the fats/oils/sweeteners group (21% vs. 18%). These differences were only significant for the grain/cereal (P = 0.039) and vegetable/juice (P = 0.002) groups.
Three-day average macronutrient intake data revealed that 26% of the students were noncompliant with the cholesterol recommendation of 300 mg/day or less, 44% did not adhere to the recommendation for total fat of 20% to 35% of daily calories, 45% did not meet the saturated fat recommendation of less than 10% of daily calories, and 95% were noncompliant with the fiber recommendation of 25 to 35 g/day. With regard to the micronutrient recommendations, 66% of the students did not meet the sodium recommendation of no more than 2,300 mg/day, 85% were noncompliant with the calcium recommendation of 1,000 mg/day, and 99% did not meet the potassium recommendation of 4,700 mg/day.
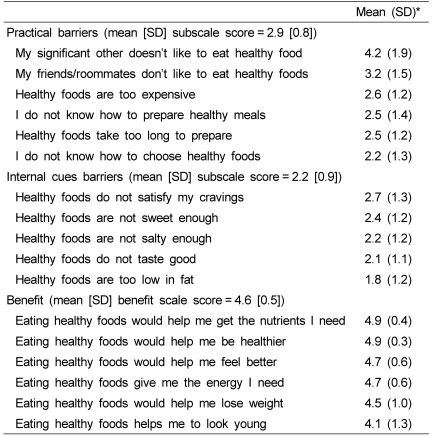
Among the 149 students who completed the demographic and psychosocial questionnaire, 57% self-classified in the preaction and 40% in the action stages of change for eating healthy. The students were most confident in their ability to choose healthy foods in positive/social situations, less confident when gaining access to healthy foods was challenging, and least confident when they were emotionally upset (Table 3).
The most important perceived barriers to healthy eating were that their significant others, friends, or roommates did not like to eat healthy foods, while the least important perceived barriers were that healthy foods are too low in fat and do not taste good. The most important perceived benefits to eating healthy foods were that these foods could help keep them in good health and provide them with adequate amounts of nutrients (Table 4).
The results from the Hosmer and Lemeshow test of model fit was not significant (Hosmer and Lemeshow Chi-square = 7.19 (df = 8) P = 0.516). The model accounted for 17.5% of the variance (Nagelkerke R square = 0.175). Only the difficult/inconvenient self-efficacy subscale predicted stage of change for compliance with current dietary recommendations (β = 1.05, P = 0.001; [Exp(β) = 2.54, 95% CI]). When the perceived barriers and benefits variables were added to the regression model, these variables accounted for 20.4% of the variance, and none of these variables independently predicted the stage of change for dietary compliance.
Unlike previous studies that have assessed the dietary patterns of U.S. college students, our entire sample consisted of students majoring in various health fields with the objective of joining the health care professions. A majority of the younger and older male and female students in the present study were noncompliant with the recommendations for the five food groups depicted on the MyPyramid, and subsequently on the MyPlate graphic, and for the DRIs examined. Compliance was particularly low for the grain/cereal, fruit/juice, and vegetables/juice groups, particularly among on-campus residents and first/second-year students, as reported previously [6-9]. Findings of particular concern for the present sample were that large proportions of the students exceeded the recommendations for total fat, saturated fat, and sodium, and consumed inadequate amounts of fiber, calcium, and potassium, increasing their risk for such debilitating conditions as heart disease, hypertension, and osteoporosis [2,5].
Forty percent of the students self-classified in the action stages of change for healthy eating. Moreover, noncompliance data among those students who provided the 3-day food records reflect a strong need among these students for learning opportunities with regard to the importance of regular consumption of nutrient-dense diets for long-term health promotion and maintenance. The unfavorable health outcomes associated with consuming energy-dense diets could be conveyed through interactive exhibits similar to those described by Byrd-Bredbenner and Finckenor, which illustrates the atherosclerotic process [19]. This exhibit could also be expanded to demonstrate the cholesterol-binding ability of soluble fiber [20]. Additionally, since college students are frequently preoccupied with weight reduction [21], these interventions should emphasize the low-calorie nature of fiber-rich foods such as grains/cereals, fruits, and vegetables, and the central role these foods could play in achieving a healthy weight.
Since the majority of the students lived off-campus, it is likely that they would have access to food preparation, as well as storage equipment and facilities. Thus, enjoyable and interactive food purchasing and preparation interventions could also be offered during supermarket tours, at student dining halls, and as part of on-campus health fairs. These programs should focus on teaching students how to include fruits, vegetables, and whole grains in palatable meal and snack recipes [22]. These recipes should employ affordable, familiar ingredients and basic preparation techniques, and should include recipes for snacks that can be conveniently and safely transported in a backpack. Such interventions would reinforce the students' most important perceived benefits of eating healthy, i.e., health maintenance and nutrient adequacy. Additionally, food purchasing interventions should teach students how to make healthy choices from vending machines, convenience stores, fast food restaurants, and grocery stores, since these food outlets may offer options that differ widely in their nutrient profiles [22].
It is acknowledged that educating these students regarding the importance of consuming nutrient-dense foods may not be sufficient to bring about favorable dietary change. Hence, translating knowledge of healthy foods into healthy food selection might occur more readily if health professionals identified the psychosocial factors that might prevent students from adopting healthy eating habits. To illustrate, the students in the present study felt least confident in choosing healthy foods when feeling emotionally upset (Table 3). It has been reported that individuals often turn to high-calorie foods for comfort, which can lead to unwanted weight gain in the long-term [23]. Additionally, the students perceived that important people in their lives do not enjoy consuming healthy foods (Table 4), and this apparently affects their own food choices. Therefore, these students would benefit from interventions designed to enhance their confidence to make healthy food choices when experiencing negative emotions, and to choose healthy food options when the important people in their lives choose less healthy foods.
This study has limitations that restrict the generalizability of the findings to the population of U.S. college students majoring in health-related fields. Dietary and anthropometric data were self-reported, introducing the possibility of recall and estimation errors [24]. Additionally, the dietary data were based only on three-day food records, and were generated by a small convenience sample of students attending a single university located in the southeastern United States; the sample consisted principally of females, whites, and off-campus residents. Thus, little information was gained regarding dietary compliance among college students from other regions of the country, men, non-whites, and on-campus residents.
In conclusion, the college students in the present study exhibited relatively poor compliance in regard to the recommended number of daily servings from the five food groups depicted on the MyPyramid, and subsequently on the MyPlate graphic, and with the DRIs for selected nutrients. If larger, more diverse probability samples of college students majoring in health-related disciplines confirm our findings, future research should focus on the design, implementation, and evaluation of educational interventions that emphasize the long-term health benefits of consuming nutrient-dense foods. Since the overweight/obese students are at particular risk of developing several chronic diseases, it is important that they know how to identify and prepare such foods, and that they recognize the health risks of making poor food choices on a regular basis [2,5]. Moreover, if future studies corroborate our findings, these students should be instructed in how to select healthy foods when experiencing emotional upset, and also in how to overcome their perceived barriers to healthy eating.
References
1. United States Department of Health and Human Services. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. 1998. Washington, DC: US DHHS;p. 98–4083.
2. Gaziano TA, Galea G, Reddy KS. Scaling up interventions for chronic disease prevention: the evidence. Lancet. 2007; 370:1939–1946. PMID: 18063028.

3. Behavioral risk factor surveillance system. Centers for disease Control and Prevention (CDC) [Internet]. 2006. Retrieved 2010 February 11. Available from: http://apps.nccd.cdc.gov/brfss/index.asp.
4. 2006 American Community Survey (S1401: School Enrollment). United States Census Bureau [Internet]. Retrieved 2009 April 8. Available from: http://factfinder.census.gov/servlet/STTable?_bm=y&-geo_id=01000US&-qr_name=ACS_2006_EST_G00_S1401&-ds_name=ACS_2006_EST_G00_&-redoLog=false.
5. Spencer L. Results of a heart disease risk-factor screening among traditional college students. J Am Coll Health. 2002; 50:291–296. PMID: 12701654.

6. Kolodinsky J, Harvey-Berino JR, Berlin L, Johnson RK, Reynolds TW. Knowledge of current dietary guidelines and food choice by college students: better eaters have higher knowledge of dietary guidance. J Am Diet Assoc. 2007; 107:1409–1413. PMID: 17659910.

7. Yeh MC, Matsumori B, Obenchain J, Viladrich A, Das D, Navder K. Validity of a competing food choice construct regarding fruit and vegetable consumption among urban college freshmen. J Nutr Educ Behav. 2010; 42:321–327. PMID: 20655281.

8. Ha EJ, Caine-Bish N. Effect of nutrition intervention using a general nutrition course for promoting fruit and vegetable consumption among college students. J Nutr Educ Behav. 2009; 41:103–109. PMID: 19304255.
9. Racette SB, Deusinger SS, Strube MJ, Highstein GR, Deusinger RH. Weight changes, exercise, and dietary patterns during freshman and sophomore years of college. J Am Coll Health. 2005; 53:245–251. PMID: 15900988.

10. MyPyramid. United States Departments of Agriculture and Health and Human Services [Internet]. Retrieved 2009 April 8. Available from http://www.mypyramid.gov.
11. Institute of Medicine. Dietary Reference intakes for calcium, phosphorus, magnesium, vitamin D, and fluoride. 1997. Washington, DC: National Academies Press.
12. Institute of Medicine. Dietary Reference intakes for thiamin, riboflavin, niacin, vitamin B6, folate, vitamin B12, pantothenic acid, biotin, and choline. 1998. Washington, DC: National Academies Press.
13. Institute of Medicine. Dietary Reference intakes for vitamin C, vitamin E, selenium, and carotenoids. 2000. Washington, DC: National Academies Press.
14. Institute of Medicine. Dietary Reference intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc. 2001. Washington, DC: National Academies Press.
15. Institute of Medicine. Dietary Reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. 2002. Washington, DC: National Academies Press.
16. Institute of Medicine. Dietary Reference intakes for water, potassium, sodium, chloride, and sulfate. 2005. Washington, DC: National Academies Press.
17. Prochaska JO. Systems of psychotherapy: A transtheoretical analysis. 1979. Homewood, IL: Dorsey Press.
18. Ôunpuu S, Woolcott DM, Rossi SR. Self-efficacy as an intermediate outcome variable in the transtheoretical model: Validation of a measurement model for applications to dietary fat reduction. J Nutr Educ. 1999; 31:16–22.

19. Byrd-Bredbenner C, Finckenor M. Dietary fat and heart disease intervention strategies. J Nutr Educ. 2000; 32:60–61.

20. Reppas C, Swidan SZ, Tobey SW, Turowski M, Dressman JB. Hydroxypropylmethylcellulose significantly lowers blood cholesterol in mildly hypercholesterolemic human subjects. Eur J Clin Nutr. 2009; 63:71–77. PMID: 17882138.

21. Strong KA, Parks SL, Anderson E, Winett R, Davy BM. Weight gain prevention: identifying theory-based targets for health behavior change in young adults. J Am Diet Assoc. 2008; 108:1708–1715. PMID: 18926139.

22. Kicklighter JR, Koonce VJ, Rosenbloom CA, Commander NE. College freshmen perceptions of effective and ineffective aspects of nutrition education. J Am Coll Health. 2010; 59:98–104. PMID: 20864435.

23. Locher JL, Yoels WC, Maurer D, van Ells J. Comfort foods: An exploratory journey into the social and emotional significance of food. Food Foodways. 2005; 13:273–297.

24. Marks GC, Hughes MC, van der Pols JC. Relative validity of food intake estimates using a food frequency questionnaire is associated with sex, age, and other personal characteristics. J Nutr. 2006; 136:459–465. PMID: 16424128.

Table 2
Frequencies and percentages of students (n = 91) non-complying with food group recommendations (N (%))




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download