Abstract
BACKGROUND/OBJECTIVE
Competent renal dietitians are crucial for better patient compliance and clinical outcomes, specifically in critical settings. The aim of this study was to develop and evaluate an evidence-based course in renal dietetics for dietitians working in health care systems where dietetic specialization is absent.
SUBJECTS/METHODS
Fifteen licensed dietitians working with hemodialysis patients in Lebanon were randomly recruited to participate in the course. The latter was developed by the study's primary investigator, according to evidence-based practice guidelines, and focused on all aspects of renal nutrition. Total course duration was 28 hours spread over a 2 month period. Dietitians' knowledge in renal nutrition was tested pre- and post-training through a 23-item questionnaire; the total score was expressed in percentage (< 60% score indicated insufficient knowledge). Paired-samples t test was used for statistical analysis.
RESULTS
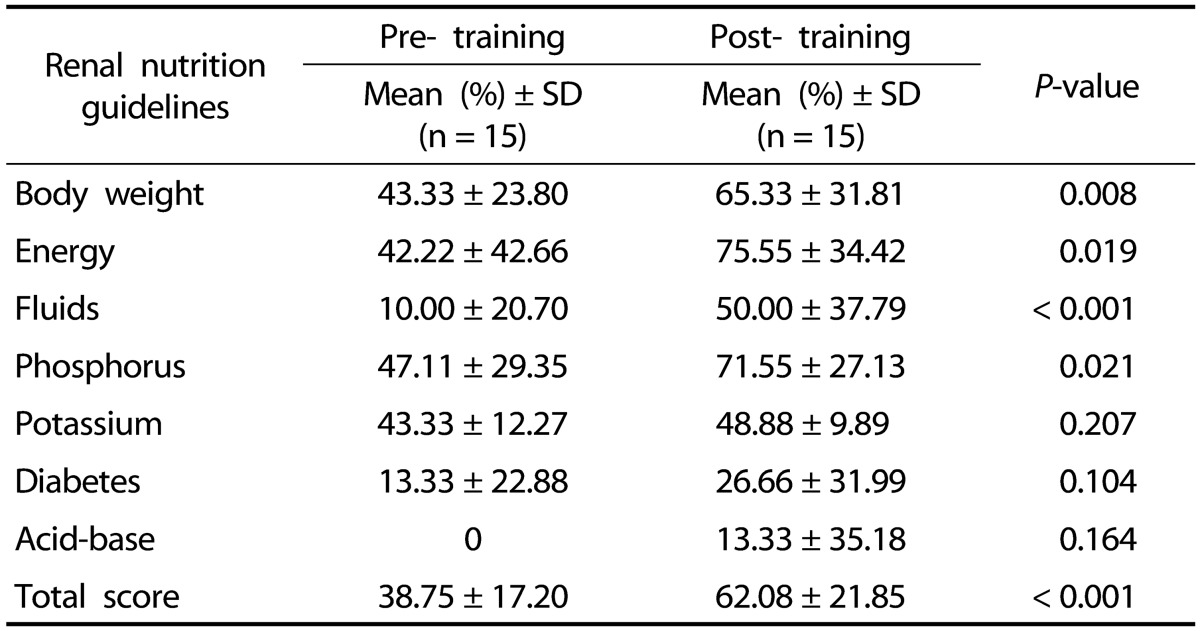
Overall knowledge of the dietitians significantly improved post-training and reached satisfactory levels (pre: 38.75 ± 17.20%, post: 62.08 ± 21.85%). Sub-analysis of the change in the knowledge showed significant and satisfactory improvement only in 3 topics: 1) correct body weight use in calculations, 2) energy estimation method and 3) phosphorus management. Knowledge in the fluid management significantly improved but did not achieve a satisfactory level.
Chronic kidney disease (CKD) is a growing public health problem worldwide, posing serious health and economic burden on individuals as well as on the societal and health care systems [1]. Up-till-now, hemodialysis (HD) remains the dominant form of renal replacement therapy (RRT) [234] with an escalating prevalence worldwide [5]. In Lebanon, hospital-based HD is the major form of RRT, with an estimated incidence of 50 cases per million population [6].
Medical nutrition therapy (MNT) is a crucial part in managing HD patients' health; literature has shown that dietitians are uniquely qualified to deliver MNT and achieve optimal dietary compliance among patients [7]. Specialized dietitian's practice involves comprehensive patient assessment, followed by delivery of effective intervention and ongoing follow up to manage the multidimensional challenges associated with chronic diseases; in renal patients it involves protein-energy malnutrition, electrolyte imbalances and anemia, to name a few [789]. Non-adherence to renal MNT is associated with poor patient outcomes and has tremendous impact on health care systems [1011]. Nevertheless, these are almost reversed when evidence-based practice guidelines (EBPG) of renal nutrition are implemented in HD care [12]. The Academy of Nutrition and Dietetics (AND) has emphasized the need for additional education and training for dietitians to become competent in the management of renal patients [13]. A few select countries have taken this further by integrating additional dietetic training and examination for the renal nutrition specialty into the professional licensing process [1415].
With the current situation where many countries lack specialized training programs for renal dietitians, developing a module to teach dietitians on the EBPG-s, and help them improve their practice, is of utmost importance [16]. This study aims to develop and evaluate an evidence-based course in renal dietetics, to be used in countries where the educational system lacks this edge.
Participants were dietitians working in the HD units selected for another interventional study [17]. The selection of the HD units was done through a computer generated randomization process from the pool of functional HD units in Lebanon according to the governmental reports. After which, an invitation letter was sent to hospital dietitians explaining the study procedure; also attached was the pre-knowledge questionnaire. The dietitians were asked to send back the filled questionnaire to the primary investigator (PI) if they were willing to take part in the study. Upon receiving the filled questionnaires, the PI contacted the dietitian(s) to arrange the conduct of the course. The protocol of the study was approved by the institutional review board (IRB) or the committee on human subjects in research (CHSR) of each participating hospital (MUMK10022011-1).
Eligible dietitians had to be: 1) holder of a bachelor degree in dietetics, 2) licensed in Lebanon and 3) working with HD patients (irrelevant of years of dietetic practice).
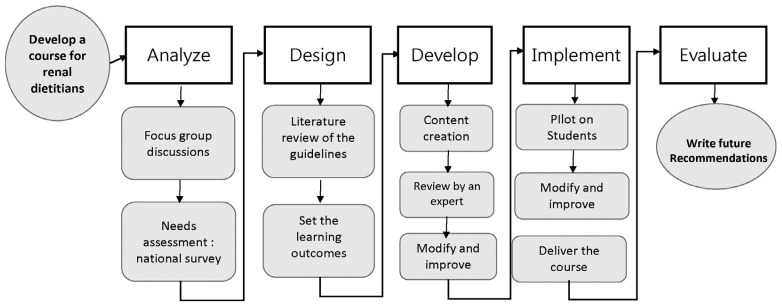
The steps of the course development and evaluation are explained below in detail and illustrated in Fig. 1.
A focus group discussion was set with a group of renal dietitians (n = 3) working in Lebanon, details of which are included in another publications [18]. They were asked to explain their opinion on the barriers to optimal dietetic care in the HD units in Lebanon. The main barriers to a better implementation of Kidney Disease Outcomes Quality Initiative (KDOQI) dietary guidelines, identified by the dietitians were time constraints and lack of supporting policies within the hospitals, in addition to the insufficient amount of education in renal dietetics in the didactic curriculum provided in Lebanon [18]. Moreover, a national survey was conducted on the practice level and knowledge of dietitians working in HD units in Lebanon, detailed methods and results of which are explained elsewhere [19]. However, the main findings exhibited the level of implementation by dietitians of each KDOQI practice guideline ranging from 10 to 59%; and the average knowledge score of KDOQI guidelines was 35.45%±16 [19]. The results of the needs assessment highlighted the necessity for a renal nutrition course to be developed and tailored to the needs of the Lebanese dietitians.
The course was designed by the Principal Investigator (PI) who was a dietitian actively practicing renal dietetics and a teacher in various settings (dietetic internship preceptor and academic instructor). Moreover, the PI had been trained on effective methods for adult learning and communication. The learning objectives of the course were divided into theoretical and practical domains and were set according to 2 factors: 1) the knowledge scores retrieved from the national survey, and 2) the level of background knowledge provided by didactic dietetic programs in Lebanon.
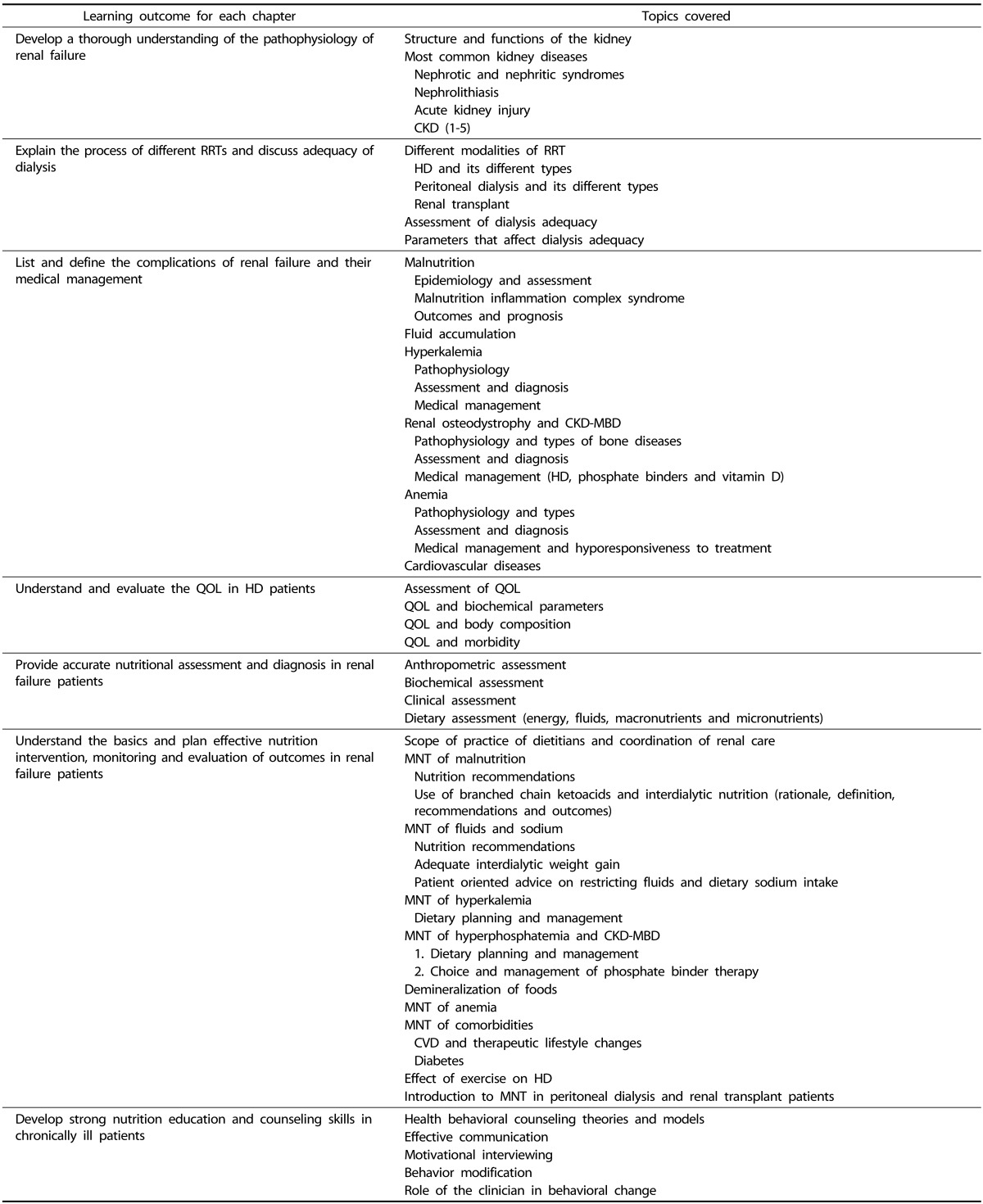
The educational material was elaborated in English and consisted of 7 chapters covering the multidisciplinary aspects of renal MNT, with specific learning outcomes for each chapter, detailed in Table 1. The order of chapters were set to build a logical trend of ideas that would achieve the learning outcomes of the course. Upon the completion of the first draft, the course was reviewed by an expert dietitian for objective evaluation; after which the course underwent minor modifications. The process of preparing the course and its assessment tools took an estimated 120 hours.
As for the methods of teaching, many methods were incorporated including: lectures using power point presentations and videos to be followed by interactive discussions, in addition to a guided analysis of real life cases for each module covered. The latter was added to foster critical thinking and problem solving abilities among the participants. Finally, homework was planned for each module, consisting of a case study to be solved individually; followed by an individual feedback by the PI. Within each lecture, ideas were first introduced in a rather abstract way, after which they were followed with an elaborative and concrete information of the topic.
The revised version of the course was pilot-tested in a class of dietetic students in an academic setting, after which additional minor modifications, specifically related to the level of detail in each chapter were incorporated, leading to the final version of the course.
The course consisted of 7 sessions (1 session/week). Each session lasted 4 hours: 3 hours of interactive lectures using PowerPoint presentations followed by a 1-hour of case-based teaching and discussion. Overall, the dietitians received a cumulative 28 hours of training over a 2 month period. The dietitians did not receive other professional trainings during the course of the study.
The training was done in groups of 3. All groups followed an identical sequence (pre-training test, training, post-training test) and received the same module, although their trainings started at different times. The groups of 3 were chosen primarily because the training was conducted at the dietitians' worksites (dietary departments of the hospitals) for feasibility purposes. Moreover, small groups were chosen for better interaction. At the end of each session the PI conducted a brief recap of the covered content. All training materials were provided in soft copy to participants at the beginning of the course to enable the dietitians to revise the material after each session.
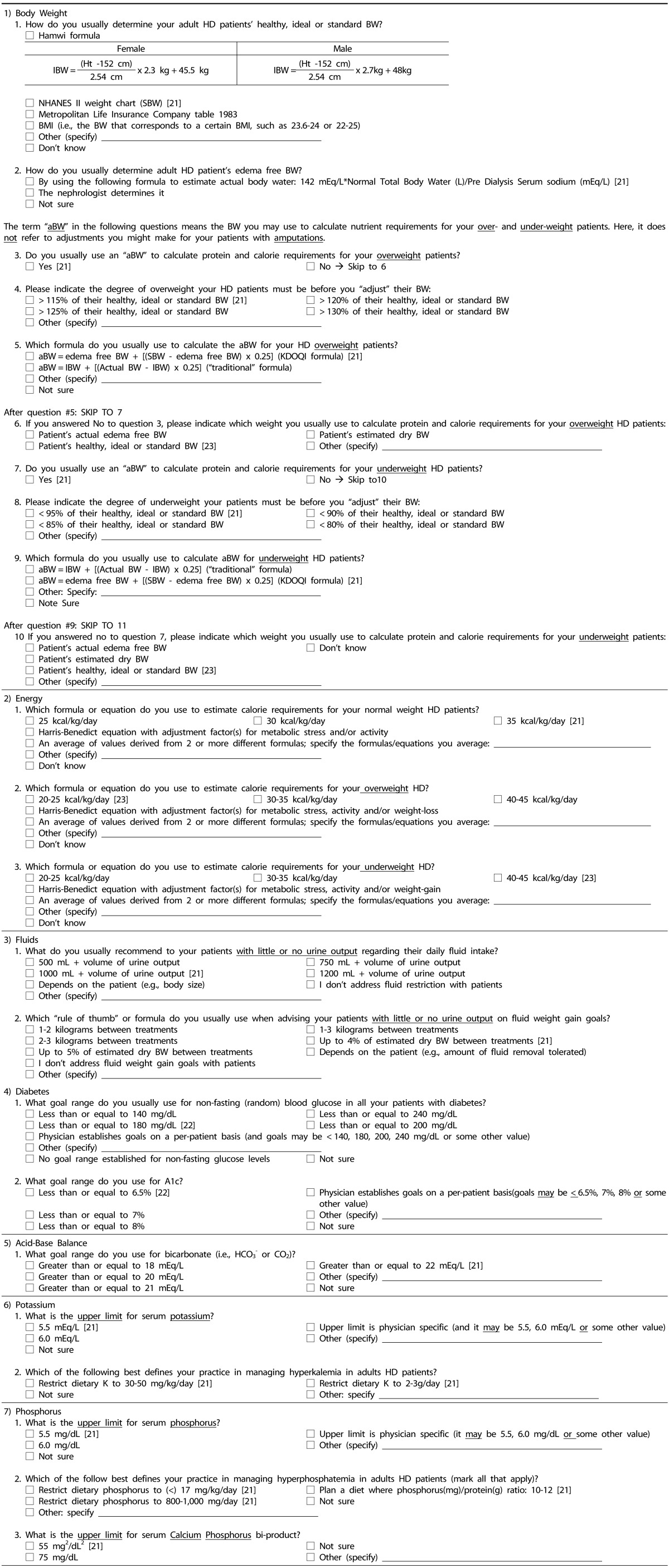
A 23-item questionnaire assessing the knowledge of the dietitians in renal MNT was used (Table 2). The questions were adapted from Vergili & Wolf [26]. The original questionnaire assessed practice patterns of renal dietitians; thus minor modifications were done to adapt it to the current study objectives. All questions that did not address renal nutrition EBPGs were removed; such as questions on demographics, patient workload to name a few. The rest of the questions in the original questionnaire assessed the level of use of each renal nutrition EBPGs in routine practice; thus rewording of each question was done, in order to transform them into knowledge assessors of the EBPGs. The original language (English) of the questionnaire was maintained since dietitians in Lebanon are fluent in English. The modified version was shared with the primary author for review; after which, it was piloted on 3 dietitians working with HD patients. Feedback from the pilot was incorporated to produce the final version.
The questionnaire evaluated the knowledge of dietitians in the following topics: 1) Body weight: assessment of body weight and use of appropriate weight for nutrient calculations; 2) Energy: estimation of energy needs; 3) Fluids: assessment of status and estimation of needs; assessment of 4) Diabetes and 5) Acid-Base Balance (serum bicarbonate); assessment of serum status and estimation of needs for 6) Potassium and 7) Phosphorus. All questions were closed-ended with multiple answer choices.
For each question, a score of 0 or 1 was given indicating a wrong/unanswered or correct answer, respectively. For questions with multiple correct answers, a partial grade was given for each correct answer; whereby the total of correct answers of that question added up to 1. The total score for each participant was calculated by summing the scores received on each question. The total actual score was then divided by the maximal total score and displayed as a percentage: [(total actual score/total maximal score)*100]. A minimum passing grade of 60% was used; this cut-off grade was adapted from academia. Furthermore, a sub-score was calculated for each of the 7 assessed topics, and was displayed as a percentage: [(actual score for the topic/total maximal score for the topic)*100]. Within a topic, each question contributed equally to the subscore, since the knowledge of each is equally important; within the whole questionnaire, topics that were more complex had more questions and thus higher weights on the total score.
Participants filled the questionnaire pre- and post-training. The PI did not review the knowledge questionnaire with any of the dietitians and correct answers were not conveyed during the training.
Data were analyzed using the Statistical Package for the Social Sciences (SPSS) (version 21, 2012, IBM inc., Armonk, New York, United States). Descriptive analysis was conducted for the demographic data. Paired samples t-test was used for the study outcomes. A p-value of 0.05 was used for statistical significance at a 95% confidence interval level.
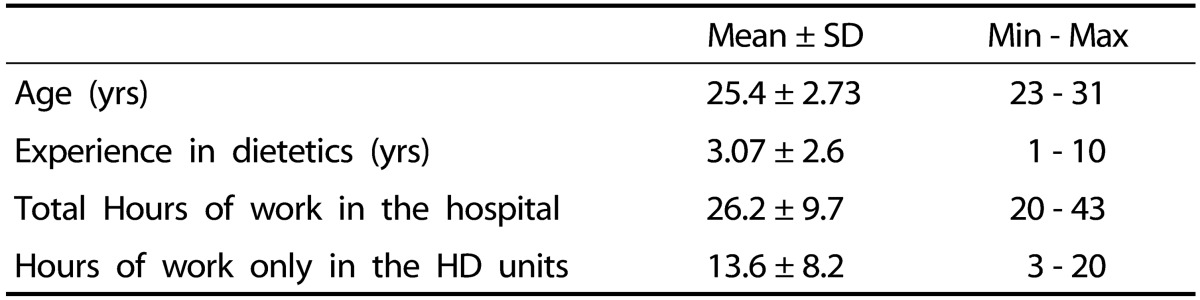
Fifteen dietitians attended and completed the training. They were all Lebanese and females. Their mean age in years was 25.4 and their mean years of experience was 3.07. Twelve of these dietitians had a master's degree in human nutrition and dietetics and none of them was specialized in any domain of nutrition. The characteristics of participating dietitians are available in Table 3.
Following the training, mean knowledge scores of the dietitians improved significantly and were slightly above the cut-off point for satisfactory knowledge (60%) (Table 4). The sub-analysis showed that the knowledge of the dietitians significantly improved only in 4 topics: 1) Body Weight: pre/post: 43.33 ± 23.80%/ 65.33 ± 31.81%; 2) Energy: pre/post: 42.22 ± 42.66%/ 75.55 ± 34.42%; 3) Phosphorus: pre/post: 47.11 ± 29.35%/71.55 ± 27.13% and 4) Fluids: pre/post: 10.00 ± 20.70%/50.00 ± 37.79%), but the latter did not reach the satisfactory knowledge cut-off point.
This study was first of its kind in the region to develop an educational module that covered all aspects of renal dietetics and assess its effect on the knowledge attained. The course material and intensity were tailored to the participating dietitians' academic educational level. In a region where specialized dietetic training is completely absent, and following a recent publication by Karavetian et al. [19] highlighting the inadequate knowledge of Lebanese dietitians in renal nutrition, the current study stands as a potential partial solution to the current situation.
The results of this study showed that the dietitians started with a low knowledge level, which significantly improved posttraining. This highlights the shortfall of the education and training in renal nutrition provided by the dietetic curriculum and internships in Lebanon. The significant improvement in knowledge denotes the effectiveness of the training, but the score of 62% is barely satisfactory. We assume that a 2-month training, consisting of only 7 sessions is adequate in increasing dietitians' knowledge, but is not enough for enabling them to reach advanced knowledge in renal nutrition care and master skills required for the complex management of renal patients. This might be enhanced by increasing the course duration and its practice-based content. The latter has shown to be effective in improving skills and implementation of new guidelines by health-care practitioners [27].
This article describes an effort to address dietetic specialization in Lebanon and the neighboring countries with a similar dietetic educational level. The reason why the study was conducted in this country is due to its regional pioneer position in the field of higher education, specifically in nutrition [28]. Lebanon was the first country in the region to develop a university program and supervised internships in dietetics [29]; and pioneered in initiating the AND-accredited coordinated program in dietetics [30]. After which, this experience has extended to the rest of the Arab world step by step [31]. This leads to the assumption that if a program is validated in Lebanon, it can easily be adopted by the others in the region. For an optimal integration of the module to other countries, the content should be tailored to the specific group. The following are the suggested steps: 1) content should be modified based on the average dietetic educational level of the target dietitian population, 2) adapted to the schedule and language of the dietitians, and to their readiness to engage in an intensive specialized nutrition education, 3) in line with the professional competence standards of the specific health care system, whether it fosters continuing education for licensing renewal or not, 4) adapted to the type of counseling methods for the target patient population, and finally 5) the course should be delivered by local trainers for better acceptability.
The training module in this study can only be considered a small step towards creating and maintaining a strong dietetic workforce in the region to support the ever-expanding need for managing chronic diseases. A sustainable dietetic specialization system that could be adopted is the one proposed in the Unites States, which encourages registered dietitians who wish to be renal specialists to receive their board certification in renal nutrition after fulfilling several requirements: 1) intensive education in renal nutrition, 2) training and work experience in the field, 3) successful completion of the specialty examination, and 4) repeating the examination every 5 years for those who wish to be recertified [32]. A similar path is also proposed for registered dietitians in Canada [33]. Moreover, renal practice groups could be established in the region as premium sources for specializations in dietetics; similar to the Renal Practice Group of AND [34], the National Kidney Foundation Council on Renal Nutrition (NKF-CRN) [35] and the Renal Nutrition Group of the British Dietetic Association [36]. A less structured professional development model, as the one adopted in Australia, is also proposed, where a post graduate short course in renal nutrition is offered for dietitians [37]. Finally, web-based (online) learning could be a novel means for dietitians willing to specialize in renal nutrition, such as AND's Online Certificate in CKD Nutrition Management [38] or the Nutrition Management Training Program provided by the National Kidney Disease Education Program (NKDEP) [39].
Although the dietitians were given the option to opt out of the study at any time, the 100% completion rate may indicate that participants were satisfied by the module; however, follow-up studies are needed to provide a rigorous assessment of the overall satisfaction and self-efficacy following this training. The current study assessed the knowledge of the dietitians regarding international EBPG-s. Some of the answers in the questionnaire might not be directly applicable to the Lebanese patients. However, these answers were retained as they represent the best possible solution, considering the scarcity of renal nutrition guidelines in this part of the world. The wide spread of answers exhibited by large standard deviations might be attributed to the small sample size (large samples tend to have smaller standard errors). Adequately powered sample with further statistical analysis should be also used to ensure validity and to generalizability of the module to the region. Future studies should also assess whether improved knowledge of the dietitians will lead to improved implementation of EBPG-s in their routine practice and better patient outcomes. This was previously questioned in the literature; a barrier-analysis survey of renal dietitians reported that almost all of them were aware of the KDOQI guidelines, yet only 5% succeeded in implementing them all [40].
In conclusion, this study pioneers in suggesting a key solution for the enhancement of renal nutrition practice and the dietetic profession, in the Arab region.
As a step forward in this mission to ensure high quality care to HD patients and their families, authors of this study suggest the following roadmap to developing renal dietetic specialization: 1) integrating this module within a specialized post-baccalaureate internship, 2) establishing a health practice accreditation system that periodically audits the knowledge and standards of practice of dietitians working with renal patients and 3) establish a system of obligatory continuing education to maintain license to practice in this field.
References
1. Schoolwerth AC, Engelgau MM, Hostetter TH, Rufo KH, Chianchiano D, McClellan WM, Warnock DG, Vinicor F. Chronic kidney disease: a public health problem that needs a public health action plan. Prev Chronic Dis. 2006; 3:A57. PMID: 16539798.
2. Anand S, Bitton A, Gaziano T. The gap between estimated incidence of end-stage renal disease and use of therapy. PLoS One. 2013; 8:e72860. PMID: 24023651.

3. Kramer A, Stel VS, Abad Diez JM, de la Torre RA, Caamano EB, Cala S, Baduell HC, Castro de la Nuez P, Cernevskis H, Collart F, Couchoud C, de Meester J, Djukanovic L, Ferrer-Alamar M, Finne P, Fogarty D, García Bazaga Mde L, Garneata L, Golan E, González Fernández R, Heaf JG, Hoitsma A, Ioannidis GA, Kolesnyk M, Kramar R, Leivestad T, Limido A, Lopot F, Macario F, Magaz A, Martín-Escobar E, Metcalfe W, Noordzij M, Ots-Rosenberg M, Palsson R, Piñera C, Postorino M, Prutz KG, Ratkovic M, Resic H, Hernández AR, Rutkowski B, Serdengeçti K, Yebenes TS, Spustová V, Stojceva-Taneva O, Tomilina NA, van de Luijtgaarden MW, van Stralen KJ, Wanner C, Jager KJ. Renal replacement therapy in Europe-a summary of the 2010 ERA-EDTA Registry Annual Report. Clin Kidney J. 2013; 6:105–115.

4. Collins AJ, Foley RN, Chavers B, Gilbertson D, Herzog C, Johansen K, Kasiske B, Kutner N, Liu J, St Peter W, Guo H, Gustafson S, Heubner B, Lamb K, Li S, Li S, Peng Y, Qiu Y, Roberts T, Skeans M, Snyder J, Solid C, Thompson B, Wang C, Weinhandl E, Zaun D, Arko C, Chen SC, Daniels F, Ebben J, Frazier E, Hanzlik C, Johnson R, Sheets D, Wang X, Forrest B, Constantini E, Everson S, Eggers P, Agodoa L. 'United States Renal Data System 2011 Annual Data Report: atlas of chronic kidney disease & end-stage renal disease in the United States. Am J Kidney Dis. 2012; 59:A7e1–e420. PMID: 22177944.
5. Eggers PW. Has the incidence of end-stage renal disease in the USA and other countries stabilized? Curr Opin Nephrol Hypertens. 2011; 20:241–245. PMID: 21422925.

6. Hatoum A, Kabalan S, Elzein H, Elhaj E. National kidney registry for Lebanon. Hum Health. 2011; 15:50–52.
7. Joint Standards Task Force of the American Dietetic Association Renal Dietitians Practice Group. National Kidney Foundation Council on Renal Nutrition. Brommage D, Karalis M, Martin C, McCarthy M, Benner D, Goeddeke-Merickel CM, Wiesen K, Byham-Gray L, House JL, Pavlinac J, McCann L. American Dietetic Association and the National Kidney Foundation Standards of Practice and Standards of Professional Performance for registered dietitians (generalist, specialty, and advanced) in nephrology care. J Ren Nutr. 2009; 19:345–356. PMID: 19712866.

8. McCann L. K/DOQI practice guidelines for bone metabolism and disease in chronic kidney disease: another opportunity for renal dietitians to take a leadership role in improving outcomes for patients with chronic kidney disease. J Ren Nutr. 2005; 15:265–274. PMID: 15827902.

9. Thelen B, Byham-Gray L, Touger-Decker R, O'Sullivan Maillet J, Khan H. Survey of current job functions of renal dietitians. J Ren Nutr. 2009; 19:450–461. PMID: 19616455.

10. Denhaerynck K, Manhaeve D, Dobbels F, Garzoni D, Nolte C, De Geest S. Prevalence and consequences of nonadherence to hemodialysis regimens. Am J Crit Care. 2007; 16:222–235. PMID: 17460313.

11. Saran R, Bragg-Gresham JL, Rayner HC, Goodkin DA, Keen ML, Van Dijk PC, Kurokawa K, Piera L, Saito A, Fukuhara S, Young EW, Held PJ, Port FK. Nonadherence in hemodialysis: associations with mortality, hospitalization, and practice patterns in the DOPPS. Kidney Int. 2003; 64:254–262. PMID: 12787417.

12. Campbell KL, Ash S, Zabel R, McFarlane C, Juffs P, Bauer JD. Implementation of standardized nutrition guidelines by renal dietitians is associated with improved nutrition status. J Ren Nutr. 2009; 19:136–144. PMID: 19218040.

13. O'sullivan-Maillet J, Skates J, Pritchett E. American Dietetic Association. American Dietetic Association: scope of dietetics practice framework. J Am Diet Assoc. 2005; 105:634–640. PMID: 15800568.
14. O'Sullivan-Maillet J. A historical perspective on specialty and advanced-level practice in dietetics. Top Clin Nutr. 2009; 24:236–242.
15. Winterfeldt EA, Bogle ML, Ebro LL. Credentialing of dietetic practitioners. Dietetics: Practice and Future Trends. 3rd ed. Sudbury (MA): Jones and Bartlett Publishers;2011. p. 51–64.
16. Moore H, Reams SM, Wiesen K, Nolph KD, Khanna R, Laothong C. National Kidney Foundation Council on Renal Nutrition. National Kidney Foundation Council on Renal Nutrition survey: past-present clinical practices and future strategic planning. J Ren Nutr. 2003; 13:233–240. PMID: 12874750.

17. Karavetian M, Abboud S, Elzein H, Haydar S, de Vries N, El Zein H. Nutritional education for management of osteodystrophy (NEMO) trial: Design and patient characteristics, Lebanon. Nutr Res Pract. 2014; 8:103–111. PMID: 24611112.

18. Karavetian M, de Vries N, Elzein H, Rizk R, Bechwaty F. Effect of behavioral stage-based nutrition education on management of osteodystrophy among hemodialysis patients, Lebanon. Patient Educ Couns. 2015; 98:1116–1122. PMID: 26070468.

19. Karavetian M, Elzein H, Hwalla N, de Vries N. Dietetic practices in hemodialysis units in Lebanon and their conformity with KDOQI nutrition guidelines. Int J Health Nutr. 2013; 4:1–8.
20. National Kidney Foundation. K/DOQI Work Group, Clinical practice guidelines for nutrition in chronic renal failure. I. Adult Guidelines. Am J Kidney Dis. 2000; 35:S17–S104.
21. Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, Hogg RJ, Perrone RD, Lau J, Eknoyan G. National Kidney Foundation. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003; 139:137–147. PMID: 12859163.

22. Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int Suppl. 2009; (113):S1–S130.
23. McCann L. Pocket Guide to Nutritional Assessment of the Patient with Chronic Kidney Disease. 4th ed. New York (NY): National Kidney Foundation Council on Renal Nutrition;2009.
24. American Diabetes Association. Standards of medical care in diabetes--2011. Diabetes Care. 2011; 34:S11–S61. PMID: 21193625.
25. Byham-Gray L, Wiesen K. American Dietetic Association Renal Practice Group. National Kidney Foundation Council on Renal Nutrition. A Clinical Guide to Nutrition Care in Kidney Disease. Chicago (IL): American Dietetic Association;2004.
26. Vergili JM, Wolf RL. Nutrition practices of renal dietitians in hemodialysis centers throughout the United States: a descriptive study. J Ren Nutr. 2010; 20:8.e1–8.e16. PMID: 19796966.

27. Zaher E, Ratnapalan S. Practice-based small group learning programs: systematic review. Can Fam Physician. 2012; 58:637–642. PMID: 22859626.
28. Turnlund JR, Tannous RI. Hospital dietetics and food service in developing countries: I. The Middle East. J Am Diet Assoc. 1983; 83:311–315. PMID: 6886267.

29. Hwalla N, Koleilat M. Dietetic practice: the past, present and future. East Mediterr Health J. 2004; 10:716–730. PMID: 16335757.

30. American University of Beirut (LB). Accreditation at the American University of Beirut [Internet]. Beirut: American University of Beirut;2014. cited 2015 August 25. Available from: http://www.aub.edu.lb/accreditation/Pages/index.aspx.
31. Academy of Nutrition and Dietetics (US). Accreditation Council for Education in Nutrition and Dietetics (ACEND®) [Internet]. Chicago (IL): Academy of Nutrition and Dietetics;2014. cited 2015 August 25. Available from: http://www.eatrightacend.org/ACEND/.
32. Commission on Dietetic Registration (US). Board certified specialist in renal nutrition eligibility requirements and application [Internet]. Chicago (IL): Commission on Dietetic Registration;2014. cited 2015 August 15. Available from: http://www.cdrnet.org/certifications/board-certified-specialist-in-renal-nutrition-eligibility-requirementsand-application.
33. Commission on Dietetic Registration (US). Obtaining board certified specialties as an RD from Canada [Internet]. Chicago (IL): Commission on Dietetic Registration;2014. cited 2015 August 25. Available from: http://www.cdrnet.org/board-certified-specialtiescanada.
34. Renal Dietitians (US). About renal dietitians (RPG) [Internet]. Chicago (IL): Renal Dietitians;2014. cited 2015 August 25. Available from: https://www.renalnutrition.org/about-renal-dietitians/.
35. National Kidney Foundation (US). Council on Renal Nutrition (CRN) [Internet]. New York (NY): National Kidney Foundation;2014. cited 2015 September 8. Available from: http://www.kidney.org/about/crn.
36. British Dietetic Association (GB). Renal Nutrition Group (RNG) [Internet]. Birmingham: British Dietetic Association;2014. cited 2015 August 25. Available from: http://www.bda.uk.com/regionsgroups/groups/renal/home.
37. Dietitians Association of Australia. Renal nutrition programme distance modules [Internet]. Deakin: Dietitians Association of Australia;2014. cited 2015 August 25. Available from: http://www.daa.asn.au/events/renal-nutrition-programme-distance-modules/.
38. Academy of Nutrition and Dietetics (US). Online learning [Internet]. Chicago (IL): Academy of Nutrition and Dietetics;2014. cited 2015 September 8. Available from: http://www.eatright.org/cpd/online/.
39. National Kidney Disease Education Program (US). Chronic kidney disease (CKD) nutrition management training program [Internet]. Bethesda (MD): National Kidney Disease Education Program;2014. cited 2015 September 10. Available from: http://www.nkdep.nih.gov/identify-manage/ckd-nutrition/training-modules.shtml.
40. Burrowes JD, Russell GB, Rocco MV. Multiple factors affect renal dietitians' use of the NKF-K/DOQI Adult Nutrition Guidelines. J Ren Nutr. 2005; 15:407–426. PMID: 16198933.

Table 2
The knowledge questionnaire (correct answers are indicated with their reference)
Adapted with permission from Vergili & Wolfe [24]
HD, hemodialysis: BW, body weight: IBW, ideal body weight: SBW, standard body weight: BMI, body mass index: aBW, adjusted body weight: aBWef, adjusted edema free body weight: E, energy: A1c, glycated haemoglobin: K, potassium




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download