Abstract
BACKGROUND/OBJECTIVES
Observational studies suggest that an association between vegetable consumption and coronary heart disease (CHD). However, the results are inconsistent. This study aimed to investigate the daily intake of vegetables on a national level and its effect on the risk of CHD risk, as determined by the Framingham Risk Score (FRS).
SUBJECTS/METHODS
This study was conducted a cross-sectional design of 2,510 male adults 40-64y of age who participated in the 2007-2009 Korean National Health and Nutrition Examination Survey. Daily intake of vegetable was assessed by 24-h recall, and the consumption frequency of vegetables was determined using a food frequency questionnaire. The odd ratio of CHD risk according to daily intake and frequency of vegetables was analyzed.
RESULTS
Total vegetable intake was inversely and significantly associated with the risk of CHD (Model 1: 4th vs. 1st quartile, OR = 0.74, 95% CI = 0.58-0.96, P for trend = 0.0015), and the significant relationship with CHD risk remained even after adjusting for potential confounders (Model 3: 4th vs. 1st quartile, adjusted OR [aOR] = 0.69, 95% CI = 0.49-0.95, P for trend = 0.0492). Subjects in the higher quartiles of non-salted vegetable intake had 31% lower odds of the risk of CHD compared to those in the lowest quartile after adjusting for various potential confounders in model 3 (aOR = 0.69; 95% CI = 0.49-0.97, P for trend = 0.0478). No significant associations between the frequency of vegetable intake (total, green, white and red vegetable) and the risk of CHD were found.
Go to : 
Heart disease is the leading cause of death in South Korea. Heart and cerebrovascular diseases are caused not only by genetic factors but also by environmental factors such as lifestyle and dietary habits [1]. There have been a number of studies reporting relationships between dietary factors and coronary heart disease (CHD); specifically, carbohydrate, dietary fiber, and fat intake as well as nutrient composition have been reported to have an effect on CHD [234].
According to a critical review of CHD, there is convincing evidence that increasing the consumption of vegetables reduces the risk of chronic disease [5]. An intake of > 600 g vegetables and fruits a day reportedly decreases the risk of ischemic heart disease by 31% and ischemic stroke by 19% [6]. Epidemiological research has shown similar results, with prospective studies indicating that vegetable consumption is negatively associated with CHD [78910]. A meta-analysis of cohort studies reported that > 5 servings of fruits and vegetables a day resulted in a pooled relative risk of 0.83 (0.77-0.89, P < 0.0001) for CHD, compared with < 3 servings a day [11]. However, the relationship between vegetable intake and the risk of CHD is slightly different based on the types of vegetables or fruits and intake diversity [89]. An intake consisting of a variety of vegetables was significantly and negatively correlated with inflammatory markers and Framingham Risk Score (FRS) in a previous cross-sectional study [12].
Vegetables reportedly affect CHD risk factors such as hypertension, hypercholesterolemia, and diabetes [13]. The presence of potassium, magnesium, dietary fiber, phytosterols, and vitamins can decrease blood cholesterol, oxidative stress, and inflammation [14151617]. A meta-analysis of 14 studies conducted in Korea and Japan determined that eating raw vegetables significantly decreases the risk of stomach cancer (overall summary OR = 0.62, 95% CI = 0.46-0.85), while the consumption of pickled vegetables significantly increases the risk of stomach cancer (overall summary OR = 1.28, 95% CI = 1.06-1.53) [18]. Unlike vegetables that are not pickled, pickled vegetable intake increases the risk of breast cancer [19]. The results of a previous multivariable-adjusted regression analysis indicate that vegetable intake is negatively associated with the risk of stroke, adjusted for age, sex, body mass index (BMI), and family history of stroke (OR = 0.311, 95% CI = 0.100-0.963) [20]. Therefore, the effect of vegetable intake on chronic disease, particularly CHD, is expected to differ by type; however, studies regarding the relationship between vegetable intake and CHD risk in Koreans are limited, despite the consumption of a variety of vegetables in Korea, such as kimchi, pickled-vegetable and wild vegetables.
Therefore, research is needed to assess the intake of vegetables in Korean adult men and investigate its relationship with CHD; this is particularly important in adult men because of the highest prevalence of CHD in adult men than in adult women [21]. The purpose of this study was to evaluate the daily intake of vegetables by type and the effect on CHD risk, as determined by the FRS.
Go to : 
The Korea National Health and Nutrition Examination Survey (KNHANES) is a cross-sectional study that uses a rolling sampling design involving a complex, stratified, multistage, probability-cluster survey of a representative sample of the non-institutionalized civilian Korean population. The survey data are collected via a health interview, health examination (physical examination and clinical measurements), and nutrition survey.
The data sets used in this study originated from the fourth KNHANES (2007-2009). A total of 24,871 individuals from 6,000 households in 200 primary sampling units took part in the 2007-2009 KNHANES (2007, n = 4,594; 2008, n = 9,744; 2009, n = 10,533). We excluded participants aged < 40 years or > 64 years; women; those who reported implausible dietary intakes (< 500 kcal/d or > 5,000 kcal/d); those with a history of myocardial infarction, stroke, or angina; and those for whom we did not have data on blood pressure, cholesterol, high density lipoprotein (HDL)-cholesterol, or health interview questions required for the FRS (i.e., smoking and hypertension treatment). Finally, 2,510 participants were included in the analysis. This study was conducted according to the guidelines laid down in the Declaration of Helsinki and was approved by the Institutional Review Board of the Korea Centers for Disease Control and Prevention, and written consent was obtained from all participants [22]. The subjects were divided into groups using quartile according to their vegetable intake amount (total vegetable, salted vegetable and non-salted vegetable), and their anthropometric characteristics, biochemical characteristics, demographic characteristics, and dietary factors were compared, while odds ratio related to CHD risk was analyzed.
In the health interview, a questionnaire regarding sex, age, education status, household income, smoking history, alcohol intake, and exercise was administered by trained interviewers. Metabolic equivalent of task values (METs) were used to classify physical activity as low (< 600 MET-minutes/week), medium (≥ 600 to <3,000 MET-minutes/week), or high (≥ 3,000 MET-minutes/week). METs are multiples of the resting metabolic rates and were calculated using the short form (version 2.0, April 2004) of the International Physical Activity Questionnaire.
The health examination included anthropometric measurements (height, weight, BMI, and waist circumference), blood pressure measurements, and blood biomarker analyses (total cholesterol, triglycerides, glucose, and HDL-cholesterol). Height was measured within 0.1 cm, and weight was measured with a metric weight scale to the nearest 0.1 kg in light clothing without shoes. BMI was calculated as body weight (kg) divided by height squared (m2). The waist circumference was measured at the smallest circumference between the rib cage and iliac crest with the subject in the standing position. Blood pressure measurements were taken 3 times, and the average of the second and third measurements for both systolic blood pressure (SBP) and diastolic blood pressure (DBP) were used. Fasting serum total cholesterol, triglycerides, glucose, and HDL-cholesterol were measured using an ADVIA 1650 Automatic Analyzer (Siemens, New York, USA) in 2007 and Hitachi Automatic Analyzer 7600 (Hitachi, Tokyo, Japan) in 2008-9. There were differences in HDL-cholesterol levels because of different analysis methods and equipment owing to a change of the clinical inspection agency in 2007 and 2008-2009. Therefore, this study used the following conversion equations to correct these level differences:
1) Conversion equation (2007) = {(raw data × 1.15) + 3.70} × 0.86 + 2.98
2) Conversion equation (2008-2009) = (raw data × 0.86) + 2.98
Trained dietitians interviewed each participant to collect dietary data through 24-hour dietary recalls. Intakes of carbohydrate, protein, fat, and dietary fiber were determined. Total vegetable intake excluding processed foods such as canned food and paste were analyzed, and then divided into salted vegetables and non-salted vegetables. Based on previous study [23], salted vegetables included kimchis (Chinese cabbage kimchi, diced radish kimchi, young radish (Yulmoo) kimchi, etc.) and pickles (cucumber pickle, radish pickle, garlic pickle, onion pickle, etc.). Non-salted vegetables excluded potatoes, mushrooms, seaweeds and salted vegetables, and included leafy and stem vegetables (Chinese cabbage, spinach, leaf beet, curled mallow, lettuce, etc.), tuber vegetables (radish, carrot, onion, balloon flower, etc.) and fruit vegetables (cucumber, tomato, green pepper, etc). Vegetable intake was also collected by food frequency questionnaire (FFQ). The FFQ was quantified using nine categories: "never or seldom", "once a month", "two to three times a month", "one to two times a week", "three to four times a week", "five to six times a week", "once a day", "twice a day" and "three or more times every day". The FFQ requested information regarding the participant's consumption frequency of 63 food items. FFQ did not inquire vegetable intake frequency with considerations how it is cooked, but surveying the total vegetable intake frequently by all cooking ways. Therefore, when analyzing FFQ data in this study, the vegetables were divided into green vegetable and white vegetable. Based on previous study [24], the individual food items in the green vegetable group include radish leaf, spinach, cucumber, and pepper; those in the white and red vegetable group include Korean cabbage, radish, sprout, cabbage, carrot, pumpkin, and tomato. To classify the vegetable intake frequency, it was divided by quartile according to daily intake frequency of each vegetable kind.
The FRS is based on the Framingham cohort study and acts as an index to predict 10-year CHD risk by scoring sex, age, smoking status, SBP, total cholesterol, and HDL-cholesterol and calculating a total score from these individual scores [25]. In this study, FRS was calculated with the standards suggested in the Adult Treatment Panel III guidelines [25]. Age (score range: 0-10) was categorized as 40-44, 45-49, 50-54, 55-59, and 60-64 years for scoring. HDL-cholesterol (score range: -1-1) was categorized as < 40 mg/dL, 40-49 mg/dL, 50-59 mg/dL, and ≥ 60 mg/dL for scoring. Total serum cholesterol (score range: 0-8) was categorized as < 160 mg/dL, 160-199 mg/dL, 200-239 mg/dL, 240-279 mg/dL, and ≥ 280 mg/dL for scoring. Smoking status (score range: 0-5) was categorized as smoker and non-smoker for scoring. SBP (score range: 0-3) was categorized as < 120 mmHg, 120-129 mmHg, 130-139 mmHg, 140-159 mmHg, and ≥ 160 mmHg for scoring. The scoring for total serum cholesterol and smoking status differed by age group, while SBP was scored differently by the status of high blood pressure treatment.
All statistical analyses were performed using SAS software (version 9.3 SAS Institute Inc., Cary, NC, USA) through a "survey procedure". The participants' characteristics were compared according to the vegetable intake quartiles. Differences in anthropometric, biochemical and demographic characteristics, and dietary intake according to vegetable intake quartiles were evaluated using a PROC GLM for continuous variables and Chi-square tests for categorical variables. Multivariable logistic regression analysis was performed to estimate the odds ratio (OR) and 95% confidence interval (CI) of CHD risk according to the vegetable intake quartiles, using the lowest quartile as the reference. To observe the difference of FRS according to the kinds of vegetable intake, the confounding factors were selected referring to the previous study [12] reporting about vegetable intake and its relation with FRS. All statistical tests were two-sided, and a P value < 0.05 was considered significant.
Go to : 
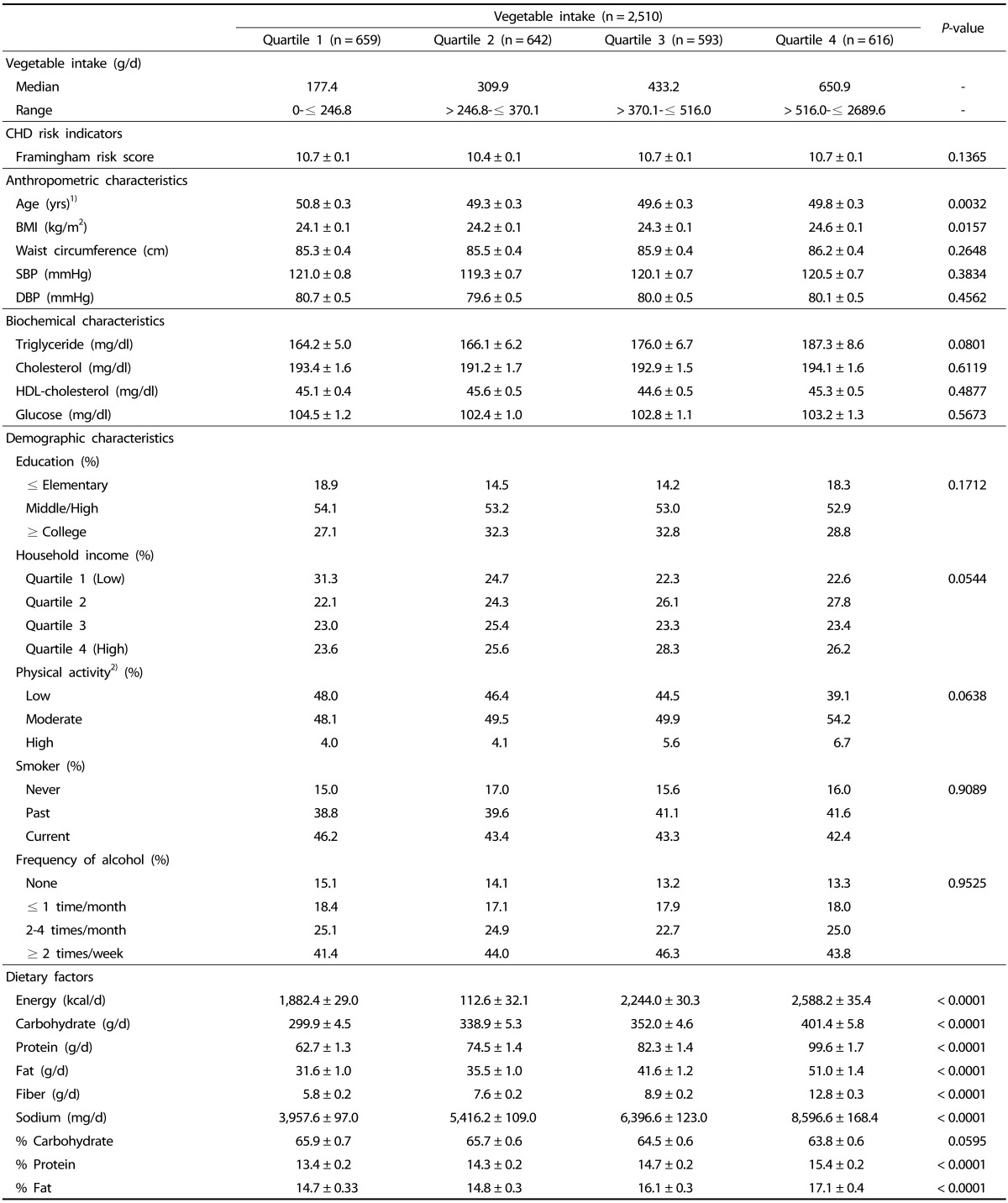
The anthropometric, biochemical and demographic characteristics, and dietary intake by quartile of dietary vegetable intake are shown in Table 1. The median vegetable intake was < 246.8 g/d in the lowest quartile and ≥ 516.0 g/d in the highest total vegetable intake quartile. No difference was observed in FRS among the total vegetable intake quartiles. Age was significantly higher in the lowest quartiles of total vegetable intake (P = 0.0032), however, BMI showed to be the lowest (P = 0.0157). Waist circumference, SBP and DBP were not significantly different among the total vegetable intake quartiles. Also, biochemical and demographic characteristics were not significantly different among the total vegetable intake quartiles. The total energy intake and carbohydrate, protein and fat intakes were significantly higher in the higher quartiles of total vegetable intake (P < 0.0001, respectively).
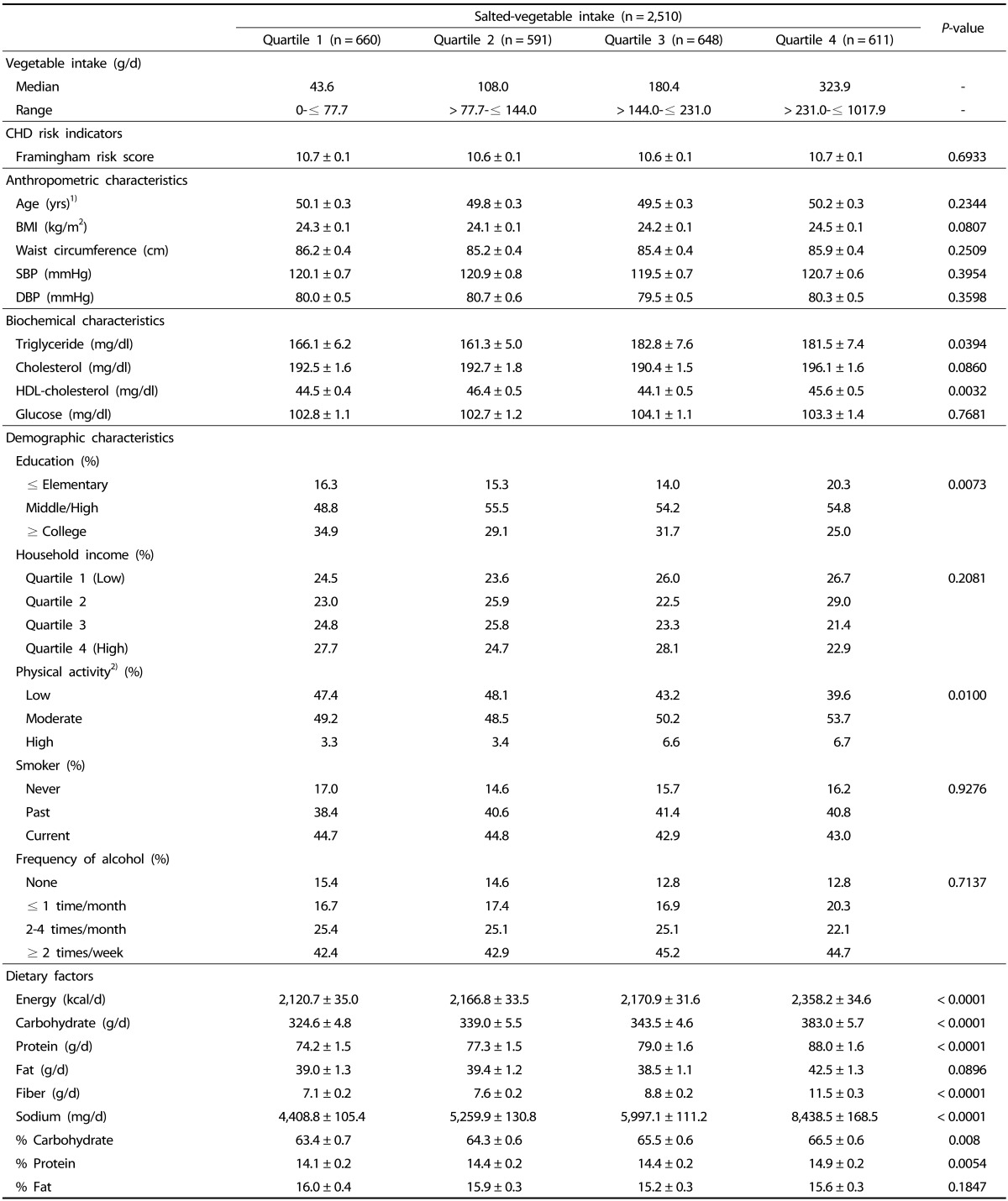
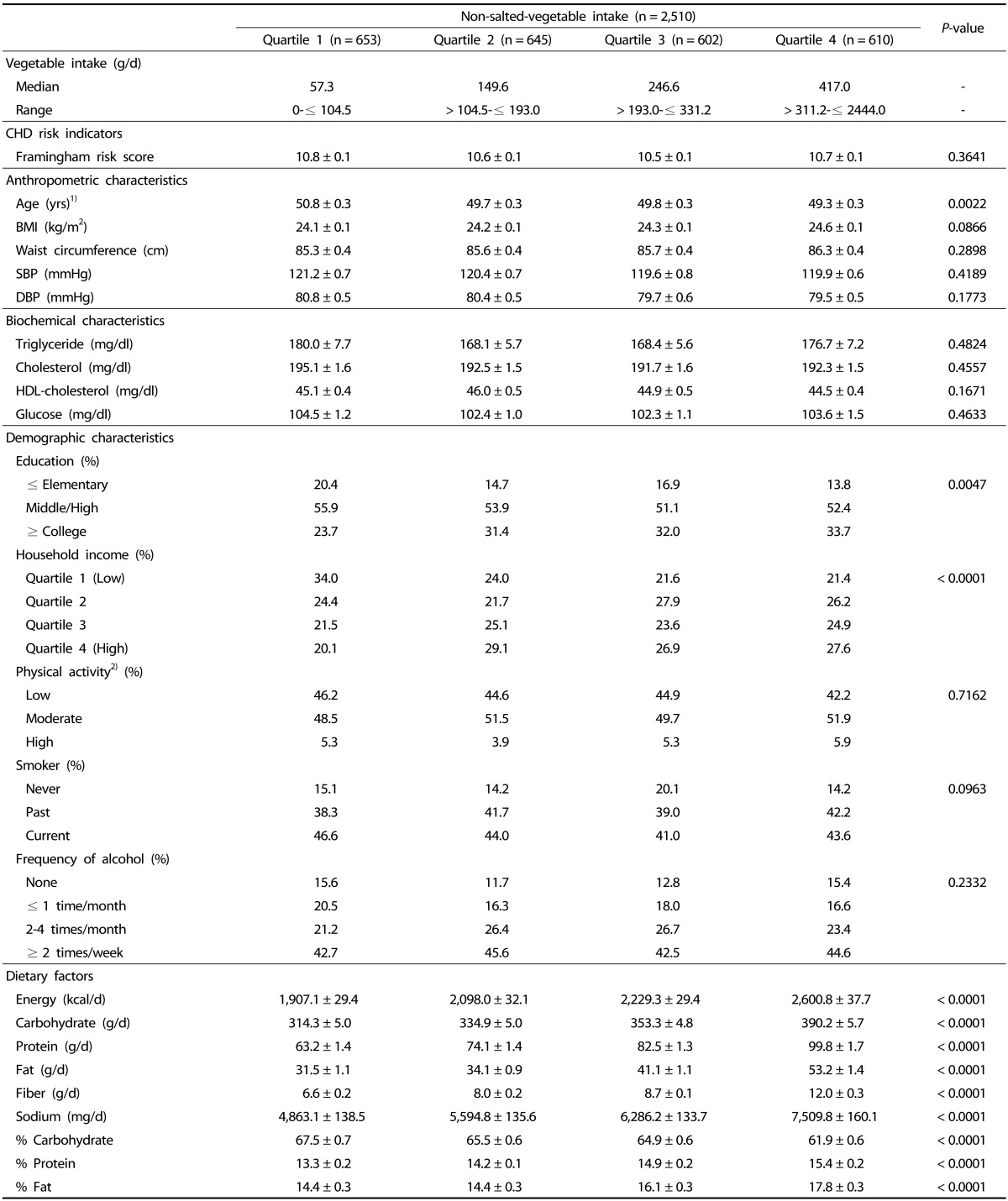
The anthropometric, biochemical and demographic characteristics, and dietary intake by quartile of dietary salted vegetable intake and non-salted vegetable intake are shown in Table 2, 3. No differences were observed in FRS among the salted vegetable intake or non-salted vegetable intake quartiles. However, in the case of serum indices, serum triglyceride was significantly higher in the highest quartiles of salted vegetable intake (P = 0.0394)
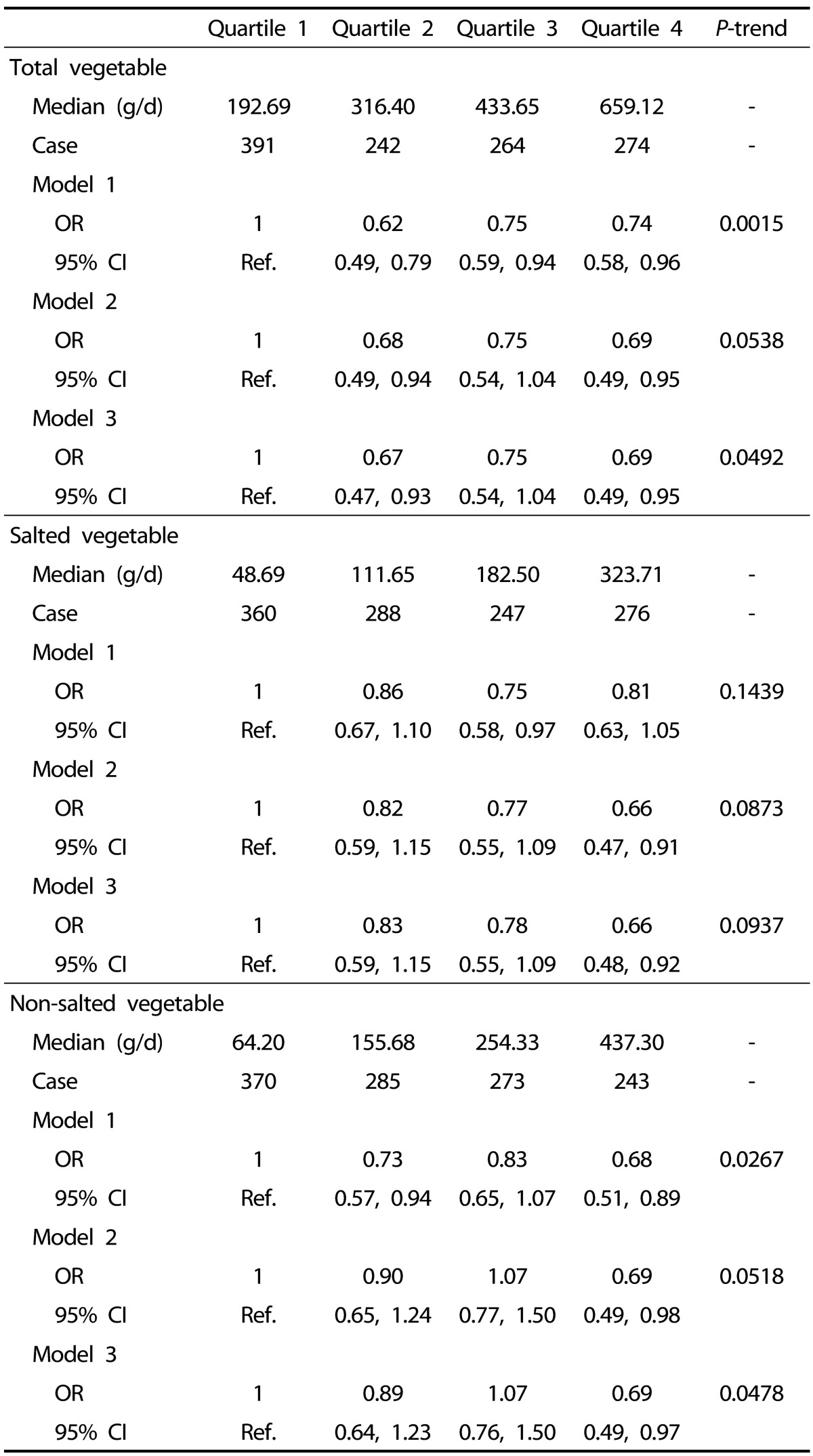
The relationships between vegetable intake and the risk of CHD are shown in Table 4. No significant association between salted vegetable intake and the risk of CHD was found. Total vegetable intake was inversely and significantly associated with the risk of CHD (Model 1: 4th vs. 1st quartile, OR = 0.74, 95% CI = 0.58-0.96, P for trend = 0.0015), and the significant relationship with CHD risk remained even after adjusting for potential confounders (Model 3: 4th vs. 1st quartile, OR = 0.69, 95% CI = 0.49-0.95, P for trend = 0.0492). Subjects in the higher quartiles of non-salted vegetable intake had 31% lower odds of the risk of CHD compared to those in the lowest quartile after adjusting for various potential confounders in model 3 (adjusted OR [aOR] = 0.69; 95% CI = 0.49-0.97, P for trend = 0.0478).
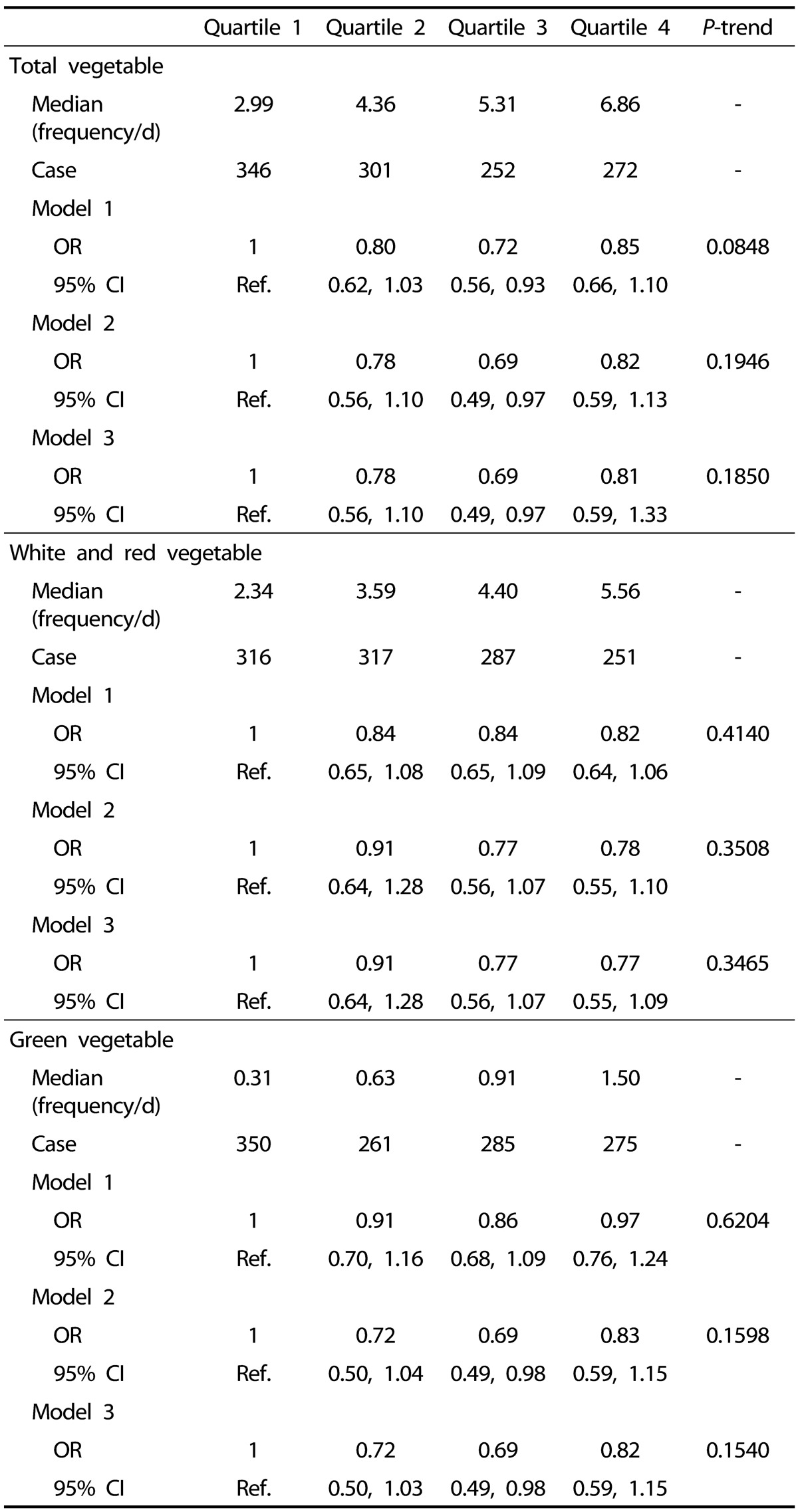
The relationships between vegetable intake frequency and the risk of CHD are shown in Table 5. No significant associations between total vegetable intake frequency, green and white vegetable intake frequency and the risk of CHD were found.
Go to : 
In the present study, the effect of vegetable intake on CHD risk, as determined by the FRS, was evaluated in Korean men using nationwide data; as a result, the intakes of total vegetables and non-salted vegetable significantly decreased CHD risk. And, no significant associations between vegetable intake frequency and the risk of CHD were found.
Previous reviews have reported that diet leads to intermediary biological mechanisms such as inflammatory processes, oxidative stress, and increased homocysteine concentrations, which increase the risk of CHD [26]. The nutrients and non-nutritive components in vegetables are likely to be important for controlling the risk of disease. Vegetables can increase the ability to control blood vessel enlargement, prevent platelet aggregation, and decrease inflammatory markers [2728].
In this study, there was no meaningful difference of metabolic indicators in blood between groups divided by vegetable intake. The Korean diet is primarily composed of plant food, accounting for 79.4% (1,143.1 g) of the total daily food intake in people aged > 1 year old [22]. The ratio of intake that is plant food increases with older age (82.6%, 40-49 years; 85.1%, 50-64 years), and older age is considered a risk factor in the calculation of the FRS. In addition, in Korea, vegetables are taken through various cooking ways in daily meals. According to a research based on 2005 KNHANES it is reported for those above 7 years old, vegetable intake is 335.9 g (26.2% of total food intake), and while the age increases the proportion of vegetable intake among total food intake [29]. In this study, quartile 1 group actually did show low vegetable intake amount, the age was the highest among 4 groups. In the case of quartile 1 group plant food or vegetable took the highest proportion of total food intake (data not shown), so it seemed like there were not much difference shown for the metabolism indicators due to biological activity strength plant food or vegetable had.
Koreans reportedly eat more pickled (or salted) vegetables, which are preserved by soaking and storing in vinegar or brine [30], than fresh vegetables [22]. In Korea, pickling can be used for kimchi, while kimchi made using salt (traditional fermented cabbage) accounts for 5.7% of daily dietary intake and is the second most commonly consumed food in Korea [22]. In addition, it is reported that jangajji, which is preserved in salt or soy sauce, is highly consumed in Korea [31]. Both the Koreans and Japanese eat vegetables preserved in salt, such as kimchi and jangajji. According to the International Study of Macro and Micro-Nutrients and Blood Pressure, the main food sources of sodium (Na) in Japan are soy sauce (20.0%), fruits and vegetables preserved in salt (e.g., jangajji) (9.8%), and miso soup (9.7%) [32]. Overconsumption of Na is a dietary habit that is suggested to increase the risk of CHD, as reported by a meta-analysis of 14 cohort studies [33]. Excessive Na intake increases blood volume; then, adrenomedullary hormones interfere with blood vessel contraction, which increases peripheral vessel resistance, leading to high blood pressure [34].
In this study, the intakes of total vegetables and non-salted vegetables were significantly and negatively correlated with CHD risk. On the other hand, in the case of salted vegetable, there was no significant relation with CHD risk. In the European Prospective Investigation into Cancer and Nutrition-Italy cohort study, which was a 7.85-year follow up study, the total intake of fruits and vegetables was not associated with CHD risk, but the intake of leafy vegetables was a strong factor for decreased CHD risk [35]. These results indicate that the type of vegetable intake and the relationship with CHD risk can differ by country, which may be related with the different diet patterns in each country. Especially, in this study, vegetable was divided into non-salted vegetable and salted vegetable to consider the effect of sodium intake on metabolism indicators related to CHD risk, and as a result salted vegetable did not show meaningful relation with CHD. According to the study of Jaacks et al. [36], dietary patterns such as low intakes of wheat products and high-fat cakes, and high intakes of beans and pickled vegetables is related with the increase of LDL cholesterol. In addition, in a study conducted on Korean men, fruits and non-pickled vegetable intake significantly has negative correlation with blood pressure, while sodium and kimchi intake significantly has positive correlation [37]. According to these kinds of preceding researches, it can be considered to recommend higher intake of total vegetable including mainly non-salted vegetable to prevent CHD, since sodium intake from non-salted vegetable is relatively lower. This suggestion through present study reflect the nutritional recommendations of the European Society of Cardiology [38] and American Heart Association [39], which recommend eating fruits and vegetables to decrease CHD risk. Therefore, strategies recommending vegetables to prevent CHD and additional specific research are necessary.
This study has several limitations. First, the present study only included a quantitative evaluation of the relationship between vegetable intake and CHD risk, while a qualitative evaluation of fruit and vegetable intake (e.g., servings, regularity, and variety) and CHD risk should be conducted. However, it is meaningful that, to the best of our knowledge, this is the first study conducted in Korea to analyze the relationship between different types of vegetable intake and CHD risk using nationwide data. Koreans especially eat vegetables in various ways in their daily basic meals, and this study is meaningful since it is suggesting the benefit related to health according to not only vegetable intake amount but also by its type. Second, owing to the cross-sectional design, a cause and effect relationship could not be determined. Retrospective method based on 24 hours was used to collect dietary intake data, so accurate reflection of the subject's intake condition may have been difficult. However in this study, FFQ data was also used to analyze the relation of vegetable intake frequency and risk of CHD, so the limitation was supplemented. Third, FRS is developed based on US population, and previous studies pointed out that CHD risk might be over or underestimated when it the Risk Score is used on other population that are not US [4041]. There is no prospective cohort study verifying the validity of FRS in Korea, so it is considered that systematic and long-term research on this is necessary.
In conclusion, total vegetable intake was inversely and significantly associated with the risk of CHD, and the significant relationship with CHD risk remained even after adjusting for potential confounders. Subjects in the higher quartiles of non-salted vegetable intake had 31% lower odds of the risk of CHD compared to those in the lowest quartile after adjusting for various potential confounders. These results indicate that higher vegetable intake may help decrease CHD risk in Korean men.
Go to : 
References
1. Kafatos A, Diacatou A, Voukiklaris G, Nikolakakis N, Vlachonikolis J, Kounali D, Mamalakis G, Dontas AS. Heart disease risk-factor status and dietary changes in the Cretan population over the past 30 y: the Seven Countries Study. Am J Clin Nutr. 1997; 65:1882–1886. PMID: 9174487.

2. Clark ML, Butler LM, Koh WP, Wang R, Yuan JM. Dietary fiber intake modifies the association between secondhand smoke exposure and coronary heart disease mortality among Chinese non-smokers in Singapore. Nutrition. 2013; 29:1304–1309. PMID: 23911218.
3. Similä ME, Kontto JP, Männistö S, Valsta LM, Virtamo J. Glycaemic index, carbohydrate substitution for fat and risk of CHD in men. Br J Nutr. 2013; 110:1704–1711. PMID: 23534456.

4. Yu D, Shu XO, Li H, Xiang YB, Yang G, Gao YT, Zheng W, Zhang X. Dietary carbohydrates, refined grains, glycemic load, and risk of coronary heart disease in Chinese adults. Am J Epidemiol. 2013; 178:1542–1549. PMID: 24008907.

5. Boeing H, Bechthold A, Bub A, Ellinger S, Haller D, Kroke A, Leschik-Bonnet E, Müller MJ, Oberritter H, Schulze M, Stehle P, Watzl B. Critical review: vegetables and fruit in the prevention of chronic diseases. Eur J Nutr. 2012; 51:637–663. PMID: 22684631.

6. Lock K, Pomerleau J, Causer L, Altmann DR, McKee M. The global burden of disease attributable to low consumption of fruit and vegetables: implications for the global strategy on diet. Bull World Health Organ. 2005; 83:100–108. PMID: 15744402.
7. Oude Griep LM, Geleijnse JM, Kromhout D, Ocké MC, Verschuren WM. Raw and processed fruit and vegetable consumption and 10-year coronary heart disease incidence in a population-based cohort study in the Netherlands. PLoS One. 2010; 5:e13609. PMID: 21049053.

8. Oude Griep LM, Verschuren WM, Kromhout D, Ocké MC, Geleijnse JM. Colours of fruit and vegetables and 10-year incidence of CHD. Br J Nutr. 2011; 106:1562–1569. PMID: 21676275.

9. Bhupathiraju SN, Wedick NM, Pan A, Manson JE, Rexrode KM, Willett WC, Rimm EB, Hu FB. Quantity and variety in fruit and vegetable intake and risk of coronary heart disease. Am J Clin Nutr. 2013; 98:1514–1523. PMID: 24088718.

10. Yu D, Zhang X, Gao YT, Li H, Yang G, Huang J, Zheng W, Xiang YB, Shu XO. Fruit and vegetable intake and risk of CHD: results from prospective cohort studies of Chinese adults in Shanghai. Br J Nutr. 2014; 111:353–362. PMID: 23866068.

11. He FJ, Nowson CA, Lucas M, MacGregor GA. Increased consumption of fruit and vegetables is related to a reduced risk of coronary heart disease: meta-analysis of cohort studies. J Hum Hypertens. 2007; 21:717–728. PMID: 17443205.

12. Bhupathiraju SN, Tucker KL. Greater variety in fruit and vegetable intake is associated with lower inflammation in Puerto Rican adults. Am J Clin Nutr. 2011; 93:37–46. PMID: 21068354.

13. Dauchet L, Amouyel P, Dallongeville J. Fruits, vegetables and coronary heart disease. Nat Rev Cardiol. 2009; 6:599–608. PMID: 19652655.

14. John JH, Ziebland S, Yudkin P, Roe LS, Neil HA. Oxford Fruit and Vegetable Study Group. Effects of fruit and vegetable consumption on plasma antioxidant concentrations and blood pressure: a randomised controlled trial. Lancet. 2002; 359:1969–1974. PMID: 12076551.

15. Thompson GR, Grundy SM. History and development of plant sterol and stanol esters for cholesterol-lowering purposes. Am J Cardiol. 2005; 96:3D–9D.

16. Hamer M, Chida Y. Intake of fruit, vegetables, and antioxidants and risk of type 2 diabetes: systematic review and meta-analysis. J Hypertens. 2007; 25:2361–2369. PMID: 17984654.

17. Oude Griep LM, Stamler J, Chan Q, Van Horn L, Steffen LM, Miura K, Ueshima H, Okuda N, Zhao L, Daviglus ML, Elliott P. INTERMAP Research Group. Association of raw fruit and fruit juice consumption with blood pressure: the INTERMAP Study. Am J Clin Nutr. 2013; 97:1083–1091. PMID: 23553162.

18. Kim HJ, Lim SY, Lee JS, Park S, Shin A, Choi BY, Shimazu T, Inoue M, Tsugane S, Kim J. Fresh and pickled vegetable consumption and gastric cancer in Japanese and Korean populations: a meta-analysis of observational studies. Cancer Sci. 2010; 101:508–516. PMID: 19860848.

19. Yu H, Hwang JY, Ro J, Kim J, Chang N. Vegetables, but not pickled vegetables, are negatively associated with the risk of breast cancer. Nutr Cancer. 2010; 62:443–453. PMID: 20432165.

20. Park Y. Intakes of vegetables and related nutrients such as vitamin B complex, potassium, and calcium, are negatively correlated with risk of stroke in Korea. Nutr Res Pract. 2010; 4:303–310. PMID: 20827346.

21. Statistics Korea. A Statistical Table of the Cause of Death, 2012. Daejeon: Statistics Korea;2013.
22. The Ministry of Health and Welfare, Korean Center for Disease Control and Prevention. Korea Health Statistics 2012: Korea National Health and Nutrition Examination Survey (KNHANESV-3). Cheongju: Korea Center for Disease Control and Prevention;2013.
23. Kwon JH, Shim JE, Park MK, Paik HY. Evaluation of fruits and vegetables intake for prevention of chronic disease in Korean adults aged 30 years and over: using the Third Korea National Health and Nutrition Examination Survey (KNHANES III). Korean J Nutr. 2009; 42:146–157.
24. Park S, Ham JO, Lee BK. Effects of total vitamin A, vitamin C, and fruit intake on risk for metabolic syndrome in Korean women and men. Nutrition. 2015; 31:111–118. PMID: 25466654.

25. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002; 106:3143–3421. PMID: 12485966.
26. Hu FB, Willett WC. Optimal diets for prevention of coronary heart disease. JAMA. 2002; 288:2569–2578. PMID: 12444864.

27. Kelley DS, Rasooly R, Jacob RA, Kader AA, Mackey BE. Consumption of Bing sweet cherries lowers circulating concentrations of inflammation markers in healthy men and women. J Nutr. 2006; 136:981–986. PMID: 16549461.

28. Erlund I, Koli R, Alfthan G, Marniemi J, Puukka P, Mustonen P, Mattila P, Jula A. Favorable effects of berry consumption on platelet function, blood pressure, and HDL cholesterol. Am J Clin Nutr. 2008; 87:323–331. PMID: 18258621.

29. Lee JS, Kim J. Vegetable intake in Korea: data from the Korean National Health and Nutrition Examination Survey 1998, 2001 and 2005. Br J Nutr. 2010; 103:1499–1506. PMID: 20128936.

30. Wikipedia. Pickling [Internet]. cited 2015 March 5. Available from: http://en.wikipedia.org/wiki/Pickled_vegetables.
31. Song DY, Park JE, Shim JE, Lee JE. Trends in the major dish groups and food groups contributing to sodium intake in the Korea National Health and Nutrition Examination Survey 1998-2010. Korean J Nutr. 2013; 46:72–85.

32. Anderson CA, Appel LJ, Okuda N, Brown IJ, Chan Q, Zhao L, Ueshima H, Kesteloot H, Miura K, Curb JD, Yoshita K, Elliott P, Yamamoto ME, Stamler J. Dietary sources of sodium in China, Japan, the United Kingdom, and the United States, women and men aged 40 to 59 years: the INTERMAP study. J Am Diet Assoc. 2010; 110:736–745. PMID: 20430135.

33. Strazzullo P, D'Elia L, Kandala NB, Cappuccio FP. Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. BMJ. 2009; 339:b4567. PMID: 19934192.

34. Blaustein MP. How salt causes hypertension: the natriuretic hormone-Na/Ca exchange--hypertension hypothesis. Klin Wochenschr. 1985; 63(Suppl 3):82–85. PMID: 4039776.
35. Bendinelli B, Masala G, Saieva C, Salvini S, Calonico C, Sacerdote C, Agnoli C, Grioni S, Frasca G, Mattiello A, Chiodini P, Tumino R, Vineis P, Palli D, Panico S. Fruit, vegetables, and olive oil and risk of coronary heart disease in Italian women: the EPICOR Study. Am J Clin Nutr. 2011; 93:275–283. PMID: 21177799.

36. Jaacks LM, Crandell J, Mendez MA, Lamichhane AP, Liu W, Ji L, Du S, Rosamond W, Popkin BM, Mayer-Davis EJ. Dietary patterns associated with HbA1c and LDL cholesterol among individuals with type 1 diabetes in China. J Diabetes Complications. 2015; 29:343–349. PMID: 25630525.

37. Kim MK, Kim K, Shin MH, Shin DH, Lee YH, Chun BY, Choi BY. The relationship of dietary sodium, potassium, fruits, and vegetables intake with blood pressure among Korean adults aged 40 and older. Nutr Res Pract. 2014; 8:453–462. PMID: 25110567.

38. Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R, Dallongeville J, De Backer G, Ebrahim S, Gjelsvik B, Herrmann-Lingen C, Hoes A, Humphries S, Knapton M, Perk J, Priori SG, Pyorala K, Reiner Z, Ruilope L, Sans-Menendez S, Op Reimer WS, Weissberg P, Wood D, Yarnell J, Zamorano JL, Walma E, Fitzgerald T, Cooney MT, Dudina A, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Funck-Brentano C, Filippatos G, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Altiner A, Bonora E, Durrington PN, Fagard R, Giampaoli S, Hemingway H, Hakansson J, Kjeldsen SE, Larsen ML, Mancia G, Manolis AJ, Orth-Gomer K, Pedersen T, Rayner M, Ryden L, Sammut M, Schneiderman N, Stalenhoef AF, Tokgözoglu L, Wiklund O, Zampelas A. European Society of Cardiology (ESC). European Association for Cardiovascular Prevention and Rehabilitation (EACPR). Council on Cardiovascular Nursing; European Association for Study of Diabetes (EASD). International Diabetes Federation Europe (IDF-Europe). European Stroke Initiative (EUSI). International Society of Behavioural Medicine (ISBM). European Society of Hypertension (ESH). European Society of General Practice/Family Medicine (ESGP/FM/WONCA). European Heart Network (EHN). European guidelines on cardiovascular disease prevention in clinical practice: executive summary. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur J Cardiovasc Prev Rehabil. 2007; 14(Suppl 2):E1–E40. PMID: 17726406.
39. Pearson TA, Blair SN, Daniels SR, Eckel RH, Fair JM, Fortmann SP, Franklin BA, Goldstein LB, Greenland P, Grundy SM, Hong Y, Miller NH, Lauer RM, Ockene IS, Sacco RL, Sallis JF Jr, Smith SC Jr, Stone NJ, Taubert KA. American Heart Association Science Advisory and Coordinating Committee. AHA Guidelines for Primary Prevention of Cardiovascular Disease and Stroke: 2002 Update: Consensus Panel Guide to Comprehensive Risk Reduction for Adult Patients Without Coronary or Other Atherosclerotic Vascular Diseases. Circulation. 2002; 106:388–391. PMID: 12119259.
40. Brindle P, Emberson J, Lampe F, Walker M, Whincup P, Fahey T, Ebrahim S. Predictive accuracy of the Framingham coronary risk score in British men: prospective cohort study. BMJ. 2003; 327:1267. PMID: 14644971.

41. Liu J, Hong Y, D'Agostino RB Sr, Wu Z, Wang W, Sun J, Wilson PW, Kannel WB, Zhao D. Predictive value for the Chinese population of the Framingham CHD risk assessment tool compared with the Chinese Multi-Provincial Cohort Study. JAMA. 2004; 291:2591–2599. PMID: 15173150.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download