Abstract
BACKGROUND/OBJECTIVES
This study aims to develop a mobile nutritional management program for integration into the already developed web-based program, Diabetes Mellitus Dietary Management Guide (DMDMG) for diabetic patients. Further, we aim to evaluate the amended DMDMG program.
SUBJECTS/METHODS
The mobile application based on an Android operating system includes three parts: 1) record of diet intake, which allows users to take pictures of the meal and save to later add diet records into DMDMG; 2) an alarm system that rings at each meal time, which reminds users to input the data; 3) displays the diet record and the results of nutrient intake, which can be also viewed through the web program. All three parts are linked to the web-based program. A survey was conducted to evaluate the program in terms of nutrition knowledge, dietary attitude, eating behavior and diet intake by non-equivalent control group design among diabetic patients with 14 DMDMG users and 12 non-user controls after a one-month trial of DMDMG.
RESULTS
Non-users did not use the program, but participated in the weekly off-line nutrition classes for one month. The program users showed increased healthful dietary behavior (P < 0.01) and dietary attitude scores (P < 0.05). More DMDMG users had higher nutrition knowledge scores after one-month trial than non-users. However, dietary intake significantly increased in non-user group for calcium and sodium (P < 0.05) while the user group did not show significant changes.
The Korean population has shown rapid increase in the prevalence of chronic diseases during last few decades, among them diabetes mellitus (DM) is the most rapidly increasing chronic disease [12]. DM is a disease with complex causes consisting of both genetics and life style including diet, exercise and stress [345], causing difficulties in finding a complete medical cure. Therefore, routine care and diet management is important [678]. Web-based computer tailored diet management is an innovative health education technique that has become popular during last decade [9]. Dietary intervention programs and health communications are more likely to be effective when they incorporate the relevant concerns, barriers and motivators of individuals, and recently released web-based systems have successfully introduced tailored health and diet information for patients' needs and interests [1011]. To date, many web-based nutrition management programs enable DM patients to improve their health and manage their diets [1213141516].
Modern technology, however, is rapidly changing. Due to fast spread of mobile phones with touch screen technology, the use of mobile applications overtake use of the web-based programs [17]. Mobile programs involve the use of handheld devices to deliver nutrition education and diet information to diabetes patients. This technology is becoming ubiquitous, while the web-based programs are limited locally, since it is available only where computers and on-line services are provided [18]. For diabetic patients, it is important to have current, updated and tailored diet information during each mealtime for systematic diabetic management. Timely tailored information, particularly computer-tailored, is generally found to be more effective in changing health behaviors compared to non-tailored information [1920]. Therefore, with the rapid changing of technology, fast adoption of these learning tools will improve health and management for DM patients, benefit diabetes prevention and may lead to a cure.
The Ubiquitous health (u-Health) care system is an innovative system, facilitated by rapid progress of information technology. In modern society, health care is shifting from 'recovery from illness' to 'maintaining wellness and preventing complications'. This new technology enables us to receive tailored interventions to maintain health in our daily lives.
The present study describes the development and evaluation of mobile u-Health application, from web-based program, aimed to develop an innovative nutrition management program for diabetic patients.
In this study, a mobile u-Health program was developed for integration into the existing web-based self-diet management u-Health program (DMDMG, http://uhdm.dongeunit.com). Then, the integrated u-Health program was evaluated with diabetic patients.
The web-based DMDMG u-Health program was developed by the authors and used as a base to develop u-Health mobile application [21] with the intention of integrating the two programs. The flow chart of the program syntax and the integration of two programs are shown in the flow chart (Fig. 1). The mobile program was developed with three parts, which are mainly for linkage to the web-based program of diet record and assessment section. The QR code was developed and provided through a web-based program to install the mobile DMDMG application into users' smart phones (Fig. 2). The three parts of the mobile application are the record of diet intake, the alarm system to alert the user to input their diet record and the results of nutrient intake. The mobile application is connected to the web-based program through main server. Users can modify and work on their diet record at any time using both mobile and web-based programs.
The evaluation of the program was conducted with 26 diabetic patients using non-equivalent control group design (14 DMDMG users and 12 controls) from October to December 2011. Participants of each group were assigned based on convenient sample allocation of nonequivalent control group study design since the OS of mobile program is limited to the Android phone system. Participants who have non-Android system smart phones were assigned to the control group. The user group used the u-Health program, including the mobile program, for one month, while the non-user control group attended the off-line diabetes diet-management class conducted every week at Bucheon Soonchunhyang Hospital. Four members of the user group used the program with the help of their family members due to the unfamiliarity with web and/or mobile programs. The rest of the user group participants used the program by themselves.
The users input their diet every day and used other sections of the web-based DMDMG regularly. They were encouraged to use the program at least 3-4 times a week. Every week, the participating dietitian checked the record of the participants through the managers' section of web-based program and contacted the participant to encourage them to follow the study protocol. Most users followed the dietitian's guidance and uploaded pictures of their meals every day.
All participants understood the purpose of the study and provided written informed consent. Before starting the one-month trial period, the user group participants met with the researchers to learn the program. One open class was held to explain user's manual and the program. All participants including the non-user control group completed the base line survey and anthropometric measurement. Participants recorded diet intake for three days before the start of the one-month trial period.
Following the one-month trial period, 26 participants gathered to complete post anthropometric measurement and survey to analyze the effectiveness and convenience of the DMDMG program. The questionnaire was developed based on literature searches of similar studies [2223242526]. Cronbach's alpha of the questionnaires for dietary attitude scores was 0.72. A five-point Likert scale was utilized to evaluate questions about dietary attitude.
Dietary behaviors were evaluated by frequency of certain behaviors per week. In this case, a three-point scale was used. One point was allotted for 0-2 days of a certain dietary behavior per week, two points for 3-5 days per week and three points for 6-7 days per week. Nutrition knowledge was scored by the count of correct answers of the 20 question in the questionnaire.
To determine the diet intake changes after using the program, a 3-day 24hr recall method was used. The food records for both user and non-user groups were analyzed with the existing web-based DMDMG program [21]. The user group participants also finished a survey on the program by answering questions using a 5-point Likert scale to select the most appropriate answer. They were also asked to comment on the program, including the mobile application with open-ended questions.
The data in this study were analyzed using SAS 9.1.3 (SAS Institute Inc., Cary, NC, USA). Mean ± SD was used to determine the changes in dietary attitudes and behaviors applying five-point and three-point scales, respectively. Nutrition knowledge was scored by assigning one point for each correct answer out of the twenty questions in the questionnaire. The Wilcoxon signed rank test was used to investigate changes before and after using the program. The Chi-square test was used to compare differences between user and non-user groups. The alpha was set at 0.05.
The mobile application using the Android operating system includes three parts and is linked to the web-based DMDMG program. The first part is to record diet intake (Fig. 3) and allows users to take pictures of their meals (Fig. 4). Users can transfer and save the pictures in the web-hard so that they can retrieve them and input their diet records into DMDMG later. This section is for more accurate dietary recall. Recorded data can be corrected anytime through the mobile application or web-based program (Fig. 5). The second part of the u-Health application is the alarm system that rings at each mealtime. The time can be set through both the mobile application and the website. When an alarm rings, users can click the pop-up icon and promptly, take a picture of their meal for the record. The third part displays the diet record and the results of nutrient intake, which can also be viewed through the web-based program (Fig. 6).
The general characteristics of the participants in the survey are shown in Table 1. The average ages were 50.5 and 49.7 years old for users and non-users, respectively. Forty-three (user group) and 33 (non-user group) percent of the participants were patients diagnosed DM less than or equal to 2 years. Perceived health and dietary life were similar and interest in nutrition management for DM was similarly high in both groups. More than half of the participants prepare meals by themselves and 74% of the participants responded that their computer skills were above average for both groups. The majority of the participants (79% users and 67% non-users) responded that they have never used websites for nutrition information in the past.
The base line self-management of DM status did not show differences between two groups. Only about 30% of the participants did not have diseases other than DM in both groups. Thirty percent of user group chose 'diet management' and 31% of control group chose 'exercise' as current self-management for DM. Most of the participants gain DM information through hospitals and/or health centers. More than 70% applied the information in their everyday lives.
Table 2 shows the results of the anthropometric status of the participants before and after the one-month DMDMG u-Health program (mobile application and web-based) trial period. No participants showed any differences in body weight and BMI before and after the one-month trial.
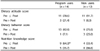
Tables 3 and 4 are the changes of dietary attitude and behavior scores before and after the trial. Total scores of dietary attitudes for both groups significantly improved after one month. The program user group significantly improved dietary behaviors, while the non-user group did not show significant differences in dietary behavior scores.
Table 5 shows the differences of nutrition knowledge scores of the participants before and after the one-month trial period using u-Health program. Both groups did not show statistically significant improvement in mean scores of nutrition knowledge; however, there were more participants with a higher nutrition knowledge score after one month in the user group than in the non-user group (Table 6, P < 0.05). However, no one answered one question about food exchange units ('One exchange unit of grain group is 2/3 bowl of rice') correctly in the user group after one month of using the program, while 50% of non-users answered it correctly. Everyone in the non-user group answered one question ('Mackerel has less fat than frozen pollack') correctly before and after the one-month trial. Before using the program, 64.3% of users answered the Mackerel question correctly, while 92.9% answered correctly after the trial was complete.
According to Table 6, more non-users than users showed - improved dietary attitude scores, while more people showed improved dietary behavior and nutrition knowledge scores (P < 0.05) in the user group than in the non-user group.
The nutrient intake of the participants before and after one month of trial period is shown in Table 7. Nutrient intake levels of application users did not show any differences before and after the one-month trial, while the non-user group showed significantly higher intake of calcium and sodium (P < 0.05).
Table 8 is the overall evaluation of the whole u-Health program (DMDMG), including both web-based and mobile program. The user group participants were asked to answer the question using the 5-point Likert scale and to select the most appropriate answer. Users gave high marks to the DMDMG system in terms of helpfulness and interest; however, the evaluation score was 3.9 concerning how easy the program was to use, suggesting that user-friendliness could be further optimized. All the users evaluated the design of the program as above average, however only 57.1% were satisfied with the content amount of the DMDMG - users thought it contains too much information. The mobile program was evaluated 4.5 out of 5-scale using three questions asking about helpfulness, convenience and interest. One question asking whether the mobile program is easy to use was evaluated at 3.5 out of five.
Three sections out of 5 sections of the DMDMG were evaluated as 'interesting and helpful': diet management (including food record), diet assessment and calories diagnosis. The prevention management section, which includes nutrition information for diabetes, meal assessment and hypertension risk factor analyses, was evaluated as 'easy to understand'. The correction of diet behavior section, composed of learning how to correct diet behavior and planning and achieving goals, was evaluated as 'easy to understand and interesting'. The meal plans section, consisting of understanding food exchange table and learning and planning menu parts, was evaluated as 'interesting and helpful'. However, the information about myself section, including blood glucose levels, height and weight, waist circumference and body fat was not graded highly (3.6-3.7). The last section is mainly for the medical staff, rather than for the patients. According to the final open-ended comments section, the users evaluated the mobile DMDMG as most useful in areas of real-time feedback and tailored intervention delivery.
Prevention is the best strategy to reduce healthcare costs due to DM complications. Changing daily routines to encourage healthy eating and exercising behavior can significantly improve health and reduce healthcare costs of DM patients over time. Nontheless, most patients do not know how to practice correct preventive behaviors or cannot adhere to the corrected manner. Therefore, preventive behavioral interventions for DM patients are very important.
Most interventions are based on face-to-face counseling models, but they are not often applied due to high costs, logistical barriers and the negative stigma associated with counseling [27]. Consequently, medical practitioners are advocating for self-management and self-directed interventions to address these challenges [28]. Self-management interventions have a positive impact with a wide range of behaviors such as improved eating behavior, physical activity and stress management for people managing DM [293031]. For effective DM self-management, the capacity for self-monitoring and feedback are essential components [32]. There are few web-based nutrition education and counseling programs developed for DM patients in Korea. These programs do not include a section for selfmonitoring [13141516]. Moreover, web-based programs have the limitation that the users must be near a computer connected to the web site. A health care service system for DM patients providing both self-monitoring and feedback has been developed using RFID (Radio Frequency Identification) [33], however, RFID is not widely used to manage DM due to limitations in cost and actigraphy. Mobile phones, specifically smartphones, offer the potential to broadly and cheaply disperse intensive self-monitoring and feedback. Furthermore, this new technology not only provides self-management and clinical support, but also supports a diverse set of streaming data.
Therefore, we aim to ameliorate the shortcomings of the existing u-Health system, by proposing a u-Health self-nutrition management program for DM patients (DMDMG), which was extended from a web-based program [21] into a more comprehensive program, including the newly developed mobile application. As expected, taking and sending meal images to the web-based program and inputting data through both mobile and web-based programs were easily performed. All users graded the mobile program as helpful, convenient and interesting, however, they evaluated the 'easy to use' question with a relatively low score (3.5 ± 0.7). The part that the users liked most in mobile application is the real-time feedback of dietary intake. Since mobile phones are always with the owner, the effectiveness of real-time feedback is not comparable with other tools.
Dietary behavior and nutrition knowledge scores improved only in DMDMG user groups while non-user group did not show any differences. However, the dietary attitude score improved in both groups. The non-users participated the weekly off-line nutrition classes for one month and showed significant improvement in the total dietary attitude score, although no specific attitudes in the 13 questions showed significant changes. In comparison, DMDMG users showed a significant improvement in the total score, as well as, improved dietary attitude scores in two of specific attitude questions concerning: "I will eat some foods that I dislike if it is good for my health" and "I count calories of the food I eat". The differences observed may be attributable to the different education patterns of DMDMG and off-line classes. DMDMG provides the food calories promptly whenever the users want. Meanwhile the participants were used to the classical off-line education. The results of this study showed that although people can get information effectively from the both types of education, the new technology was introduced successfully and is a more convenient education tool.
DMDMG incorporated two main components: a web-based interactive self-management program and a mobile device that provided feedback about diet with nutrient intake information. The impact of these two components cannot be separated presently. Nonetheless, the results show that the combined strategy is more helpful for the DM patients than the conventional off-line classes. The portability and programmability of smart phones simplify data collection. In a food intake study, electronic PDA diaries were suitable for collecting dietary reports [34]. Since the new technologies of smart phones retain enhanced functionalities of a PDA and are on track to be used by most of the population, especially in Korea, these technological advancements can greatly enhance effectiveness of nutrition management of DM patients.
Although our results showed positive changes in dietary attitude, dietary behavior and nutrition knowledge scores, the anthropometric and nutrient intake data did not show any changes. The study period was relatively short to expect such changes. Moreover, some of the participants had problems using the computers and/or mobile phones causing them to rely on younger family members for assistance. It is possible that the participants had hard time completely engaging with the new technology tools. As shown in previous research [3637], to properly utilize and adopt self-monitoring tool technologies, an approach through a gradual adoption process is essential for older adults. In our case, a one-month adoption period was not enough time for positive changes in actual behaviors rather than the knowledge and perception. As found in the recent review [38], studies longer than 8 weeks showed positive behavioral changes using electronic self-monitoring devices. Therefore, we can also expect more positive changes in dietary behaviors and attitudes, and consequently in anthropometric data if we conducted the trial for longer period.
Another limitation our study faced involved the question concerning 'One exchange unit of grain group is 2/3 bowl of rice'. No one in user group gave the correct answer after using the program. Most of people think the concept of portion size difficult. Users either had hard time estimating portion sizes and made substantial errors [3940] or gave improper portion size estimation for data-base application, as indicated from the previous study [41]. Even if most application users had trouble understanding the portion size and food exchange table, the non-user group did not have problems with the portion-size question. In this regard, face-to-face education is more effective than the self-interactive program, since a more detailed explanation can be provided.
Despite the limitations, this study also showed strength for the future of scalable modern technology for self-nutrition monitoring of DM patients. The average age of the participants of this study is 50 y. This age group represents a population subgroup that has been slow to adopt new technology [37]. Our participants showed high interest in both the web program and mobile application and used the technology effectively after a brief training session prior to the initiation of the study. Smart phones have become accessible to a degree, and therefore, interventions that use technology to augment an existing DM managing system hold great potential to advance population health. Technology can offer new channels to reconfigure the delivery of effective components of self-management strategy for DM patients such as real-time feedback, self-monitoring and delivering individualized and tailored interventions.
Figures and Tables
Table 4
Changes in dietary behaviors

*P < 0.05, **P < 0.01 by Wilcoxon signed rank test
1)Mean ± SD, The total score is a sum of 3-point scale of frequencies of the behavior per a week (1 point for 0-2 days, 2 points for 3-5 days and 3 points for 6-7 days per a week).
2)Questions showed significant differences between pre and post-test out of 19 total questions.
ACKNOWLEDGMENTS
The authors thank Mr. Soo Keun Yoon, Mr. J.T. Kong and Mr. S.I. Song for their valuable efforts in the development of the program.
References
2. Statistics Korea. Annual Report on the Cause of Death Statistics. Daejeon: Statistics Korea;2011.
3. Stevens MJ, Feldman EL, Greene DA. The etiology of diabetic neuropathy. The combined roles of metabolic and vascular defects. Diabet Med. 1995; 12:566–579.

4. Medalie JH, Papier CM, Goldbourt U, Herman JB. Major factors in the development of diabetes mellitus in 10,000 men. Arch Intern Med. 1975; 135:811–817.

5. Par YS, Lee HK, Kim SY, Koh CS, Min HK, Lee CG, Ahn MY, Kim YI, Shin TS. Risk factors for non-insulin dependent diabetes mellitus. J Korean Diabetes Assoc. 1996; 20:14–24.
6. Franz MJ, Horton ES Sr, Bantle JP, Beebe CA, Brunzell JD, Coulston AM, Henry RR, Hoogwerf BJ, Stacpoole PW. Nutrition principles for the management of diabetes and related complications. Diabetes Care. 1994; 17:490–518.

8. The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993; 329:977–986.
9. Kreuter M, Farrell D, Olevitch L, Brennan L. Tailoring Health Messages: Customizing Communication with Computer Technology. Mahwah (NJ): Lawrence Erlbaum Associates Inc.;2000.
10. Witte K. Fishing for success: using the persuasive health message framework to generate effective campaign messages. In : Maibach E, Parrott RL, editors. Designing Health Messages: Approaches from Communication Theory and Public Health Practice. Thousand Oaks (CA): Sage Publications, Inc.;1995. p. 145–166.
11. Skinner CS, Siegfried JC, Kegler MC, Strecher VJ. The potential of computers in patient education. Patient Educ Couns. 1993; 22:27–34.

12. Rollo ME, Ash S, Lyons-Wall P, Russell A. Trial of a mobile phone method for recording dietary intake in adults with type 2 diabetes: evaluation and implications for future applications. J Telemed Telecare. 2011; 17:318–323.

13. Park SY, Han JS. Effects of web-based nutrition counseling on nutrient intake and blood glucose in type II diabetic patients. J Korean Soc Food Sci Nutr. 2005; 34:1398–1406.

14. Kim HS. Effects of Web-based diabetic education in obese diabetic patients. J Korean Acad Nurs. 2005; 35:924–930.

15. Park SY, Han JS. Effects of web-based nutrition counseling on dietary behavior and food intake of type II diabetic patients. J Korean Soc Food Sci Nutr. 2006; 35:430–439.

16. Oh JA, Kim HS, Park MJ, Shim HS. Effects of Web-based health education on blood glucose and blood pressure improvement in postmenopausal women with impaired fasting blood glucose. J Korean Acad Nurs. 2011; 41:724–731.

17. Diem KG, Hino J, Martin D, Meisenbach T. Is extension ready to adopt technology for delivering programs and reaching new audiences? J Extension. 2011; 49:6FEA1.
18. Sørensen C, Yoo Y, Lytinen K, Degross JI. Designing ubiquitous information environments: Socio-technical Issues and Challenges. New York (NY): Springer;2005.
19. Brug J, van Assema P. Differences in use and impact of computer-tailored dietary fat-feedback according to stage of change and education. Appetite. 2000; 34:285–293.

20. Brug J, Campbell M, van Assema P. The application and impact of computer-generated personalized nutrition education: a review of the literature. Patient Educ Couns. 1999; 36:145–156.

21. Ahn Y, Bae J, Kim HS. Development of web-based u-Health self-nutrition management program for diabetic patients. Korean J Community Nutr. 2014; 19:372–385.

22. Ahn Y, Bae J, Youn JE, Kim HS. Needs assessment for web-based self-management program by the nutrition knowledge levels of diabetic patients. Korean J Community Nutr. 2011; 16:155–168.

23. Choe SJ, Park HR, Park DY, Ahn HS. A study on the sociopsychological factors influencing the dietary compliance of diabetics by using focus group interview. Korean J Community Nutr. 2000; 5:23–35.
24. Kang HJ, Shin EM, Kim KW. Evaluation of nutrition education for diabetes mellitus management of older adults. Korean J Community Nutr. 2009; 14:734–745.
25. Lim HS, Chyun JH, Kim YS, Nam MS. Effect of nutrition education on diabetic management in diabetic patients. Korean J Nutr. 2001; 34:69–78.
26. Park DY, Choe SJ, Park HR, Ahn HS. A study on the sociopsychological factors influencing the dietary compliance of diabetics using questionnaire. Korean J Community Nutr. 2000; 5:36–49.
27. Miller RL, Shinn M. Learning from communities: overcoming difficulties in dissemination of prevention and promotion efforts. Am J Community Psychol. 2005; 35:169–183.

28. Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002; 288:2469–2475.

29. Glasgow RE, La Chance PA, Toobert DJ, Brown J, Hampson SE, Riddle MC. Long-term effects and costs of brief behavioural dietary intervention for patients with diabetes delivered from the medical office. Patient Educ Couns. 1997; 32:175–184.

30. Gillett M, Dallosso HM, Dixon S, Brennan A, Carey ME, Campbell MJ, Heller S, Khunti K, Skinner TC, Davies MJ. Delivering the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cost effectiveness analysis. BMJ. 2010; 341:c4093.

31. Steed L, Lankester J, Barnard M, Earle K, Hurel S, Newman S. Evaluation of the UCL diabetes self-management programme (UCL-DSMP): a randomized controlled trial. J Health Psychol. 2005; 10:261–276.

32. Chodosh J, Morton SC, Mojica W, Maglione M, Suttorp MJ, Hilton L, Rhodes S, Shekelle P. Meta-analysis: chronic disease self-management programs for older adults. Ann Intern Med. 2005; 143:427–438.

33. Lee Y, Lee M. Design of healthcare service system for diabetes patients using RFID. Proc Korean Inf Sci Soc Conf. 2006; 33:43–47.
34. Collins LM, Baker TB, Mermelstein RJ, Piper ME, Jorenby DE, Smith SS, Christiansen BA, Schlam TR, Cook JW, Fiore MC. The multiphase optimization strategy for engineering effective tobacco use interventions. Ann Behav Med. 2011; 41:208–226.

35. Beasley JM, Riley WT, Davis A, Singh J. Evaluation of a PDA-based dietary assessment and intervention program: a randomized controlled trial. J Am Coll Nutr. 2008; 27:280–286.

36. Demiris G. Privacy and social implications of distinct sensing approaches to implementing smart homes for older adults. Conf Proc IEEE Eng Med Biol Soc. 2009; 2009:4311–4314.

37. Daugherty BL, Schap TE, Ettienne-Gittens R, Zhu FM, Bosch M, Delp EJ, Ebert DS, Kerr DA, Boushey CJ. Novel technologies for assessing dietary intake: evaluating the usability of a mobile telephone food record among adults and adolescents. J Med Internet Res. 2012; 14:e58.

38. Lieffers JR, Hanning RM. Dietary assessment and self-monitoring with nutrition applications for mobile devices. Can J Diet Pract Res. 2012; 73:e253–e260.

39. Rumpler WV, Kramer M, Rhodes DG, Moshfegh AJ, Paul DR. Identifying sources of reporting error using measured food intake. Eur J Clin Nutr. 2008; 62:544–552.

40. Poslusna K, Ruprich J, de Vries JH, Jakubikova M, van't Veer P. Misreporting of energy and micronutrient intake estimated by food records and 24 hour recalls, control and adjustment methods in practice. Br J Nutr. 2009; 101:Suppl 2. S73–S85.




 PDF
PDF ePub
ePub Citation
Citation Print
Print














 XML Download
XML Download