Abstract
The study objectives were to increase both the stage of readiness to eat fruit and vegetables as well as the intakes of women who participated in the Expanded Food and Nutrition Education Program (EFNEP) for families with limited incomes. The intervention was to enhance the currently used curriculum, Eating Right Is Basic III (ERIB3), with stage-specific processes based on the Trans-Theoretical Model of readiness to change. Trained EFNEP community workers taught the enhanced curriculum to 90 mothers in the experimental county and to 53 mothers in the control county. Pre- and post-intervention measures included stages of readiness to eat fruit and vegetables and to intake as assessed by 24-hour dietary recalls and staging questions. Most women recruited into EFNEP were in Action and Preparation Stages (53.5%). Fruit and vegetable intakes showed a linear trend along with the Stage of Change for fruit and vegetable. After intervention, some combination of the ERIB3 and the fruit and vegetables-enhanced ERIB3 resulted in a reported 1/2 servings/day increase in fruits and vegetables in both the control and the experimental counties, although changes were not significant. EFNEP women also moved along the Stage of Change Continuum for fruits and vegetables in both counties. The percentage of people who ate 5 or more servings of fruit and vegetables was significant, however, only in the experimental group. We encourage health professionals to apply lessons learned from this intervention and to continue to pursue theoretically based interventions to change dietary behaviors.
In the United States, the current low intakes of fruits and vegetables are considered modifiable dietary factors that contribute to risks for chronic diseases (Briefel & Johnson, 2004), especially in populations with limited education and household incomes (Algert et al., 2006; Havas et al., 1998; Johnson et al., 2004). Reducing such health disparities has been targeted in national policy documents such as Healthy People 2010 (DHHS, 2000). The Dietary Guidelines for Americans places so much importance on increasing consumption of foods of plant origin that the guidelines were given priority position in 2005 (DHHS, 2005). It is clear from market research, national surveys, and studies of limited income populations, however, that typical diets include far too few fruits and vegetables (Cox et al., 1995; Frazao, 1995; Zenk et al., 2005), and interventions to increase these foods have met with limited success, especially in families with limited incomes (Subar et al., 1995).
For the last few decades in the United States, health professionals have been urged to base their health behavioral interventions on theory (Achterberg, 2004; Glanz, 2002; NIH/NCI, 2005). Trans Theoretical Model (TTM), also called Stages of Change, is one such model that has been validated for several health behaviors such as smoking and drug use (Prochaska et al., 1992). The nutrition education community has become interested in TTM due to its promise for tailoring interventions according to the participants' stages of readiness for dietary change as well as, for demonstrating client progress prior to actual dietary changes. Briefly, people change problematic dietary behaviors by advancing through five stages: pre-contemplation, contemplation, preparation, action and maintenance. In the earlier stages, people first deny and then gradually begin to realize and deal with their health problems (Kasila et al., 2003; Van Duyn et al., 1998). Within the last decade, some studies have employed TTM for use for promoting changes in food intake behaviors (Glanz et al., 1994; Greaney et al., 2004; Greene et al., 2004; Sporny et al., 1995). Only a few studies, however, have been conducted using TTM for populations with limited incomes, who generally have lower fruit and vegetable intakes than the general population (Havas et al., 2003; Henry et al., 2006; Perkins-Porras et al., 2005; Wellman et al., 2007), likely because this is not an easy population to reach.
An efficient way to reach families with limited incomes is often to use existing programs that provide food and nutrition education. The Expanded Food and Nutrition Education Program (EFNEP) in the United States is the major program to provide such a nutrition education service for low-income families with children. The United States Department of Agriculture and state and county governments fund EFNEP, which is implemented by the Cooperative Extension Service (New York State Cornell Cooperative Extension, 1998). EFNEP promotes improved dietary habits, food resource management, and food preparation through individual or small group sessions in primarily urban counties with a high prevalence of families with limited incomes. EFNEP hires front-line paraprofessionals or community workers (food and nutrition educators) from among the population served, on the premise that the life experience of indigenous community nutrition educators enhances their rapport and credibility with the program audience (Bremner et al., 1994). Professional home economists supervise the work of and provide community workers with three months of intensive training on food and nutrition education prior to beginning any intervention. The widely used skill based curriculum is called Eating Right Is Basic III (ERIB3); it incorporates food guidance, food label and food safety recommendations, which is considered ideal for teaching adults how to choose and prepare healthy, low cost meals (MSUE, 2005). The curriculum consists of six basic lessons that all participants receive and 10 optional lessons.
The goal of this study was to increase fruit and vegetable intakes of families with limited incomes via EFNEP by enhancing the ERIB3 curriculum to reflect teaching techniques appropriate for homemakers in pre-action stages of readiness (pre-contemplation, contemplation and preparation) to eat more fruits and vegetables or in post action stages (action and maintenance) and to evaluate effectiveness. To this end, the intakes of fruits and vegetables and the readiness to increase of fruits and vegetables in EFNEP women were assessed and any changes evaluated immediately in post intervention.
Two counties in a north central state of the U.S. that had EFNEP programs and similar population demographics of size, household incomes and ethnic diversity were targeted for participation with one county to receive the enhanced intervention and the other the regular ERIB3 intervention. EFNEP community workers from the two counties recruited all EFNEP mothers as participants whom they enrolled into the program over two months during the spring and early summer. The target was 90 women in each county and the incentive for EFNEP participants was $10.00 in cash for completion of questionnaires before and after the intervention. The average age of the participants was 29.3 year in the control county and 25.5 year in the experimental county.
The investigators worked with county staff to develop useful, relevant teaching materials and techniques to help move participants along the stage of change continuum towards eating more fruits and vegetables by selectively enhancing the six basic lessons of ERIB3. State staff, county home economists and EFNEP community workers examined the processes appropriate to use at each stage of change for eating fruit and vegetables and dichotomized them into two groups of pre- and post-action stages for parsimony of teaching materials. Pre-action processes focused on consciousness raising such as providing specific examples of the health benefits--both immediate and long-term--of fruit and vegetables to themselves and to their families. Post-action processes included specific strategies for incorporating more fruit and vegetables such as adding vegetables to soups, mixed dishes and sandwiches. Many action processes were already in the ERIB3 lessons, but examples specific to fruit and vegetables were added. In addition, four half page handouts printed on colored card stock were developed on the following topics: nature's fast foods--fruits and vegetables; $5 a week for 5 servings a day; 5 for fiber; feel good, look good with fruits and vegetables. Each handout contained pre-action information on one side and post-action processes on the other. Participants in each county received six of the 16 lessons, but those in the intervention group also received the TTM enhanced ERIB3 lessons and the four handouts.
Following approval by the university's institutional review board, the enhanced intervention materials were developed and half-day workshops were held with county staff on recruitment techniques and data collection. For the intervention county, an additional half day workshop was held to teach the principals of the TTM, how to assess the participant's stage of readiness to eat fruit and vegetables, and then how to intervene with the appropriate stage based processes pertinent to each lesson. The researchers provided all the community workers with canvas briefcases with the university logo as incentives to participate and to assist with the study.
Upon completion of the EFNEP intervention with participants in both counties, the community workers assessed each participant for stage of change for fruit and vegetables. Two non-consecutive dietary recalls were collected at the baseline and one at the end of the sixth lesson.
Stage of change for fruit and vegetable intakes combined were measured using the staging algorithm beginning with, "How many servings of fruits and vegetables do you eat a day?" (Glanz et al.,1994). Fruit intake included fruit and 100% fruit juice; vegetable intake included fried potatoes and vegetable juice. The serving sizes were defined according to the U.S. Food Guide Pyramid, where ½ cup of cooked vegetables or fruit was a serving (DHHS, 2000). Criteria for fruit and vegetable servings were the minimum recommended intakes from this guideline (DHHS, 2000). Responses were marked 0-4+ for fruits and 0-5+ for vegetables with 4+ and 5+ truncated to 4 and 5, respectively, in the calculations. Investigators categorized subjects for action/maintenance stages, if they answered eating >5 servings for fruit and vegetables per day (Glanz et al., 1994). Then, intention and time period for eating enough fruit and vegetables were asked for further stage divisions (Serdula et al., 1993; Van Duyn et al., 1998). Respondents were classified as in the pre-contemplation stage when they did not intend to eat five or more servings of fruit and vegetables. Participants were in the contemplation stage when the algorithm indicated they intended to eat these amounts within 6 months. They were considered to be in the preparation stage when they intended to eat the recommended servings within 30 days. Thus, the staging items provided both a stage of change for each participant, as well as one of the measured of total of fruit and vegetable intakes.
Demographic data included age, marital status, number of children, status as pregnant or lactating, and participation in other food related government programs. One program of interest was the Special Supplemental Nutrition Program for Women Infants and Children (WIC) that provides coupons for foods high in protein, iron, calcium, vitamin A and vitamin C plus one 30-minute diet counseling session every six months. WIC is a large, federally funded effort to reduce nutrition-related risks in order to improve birth outcomes and early childhood development. The program provides certain foods and nutrition education to pregnant, postpartum, and breastfeeding women and their infants and children up to age five. The other program of interest was Project FRESH (Farm Resources Expanding and Supporting Health), a special summer program available to some women in WIC where they receive $20 of food coupons redeemable for fresh fruits and vegetables at farmers markets. Race was self-identified as Anglo-American, African American, Asian American, or Other.
Fruit and vegetable intakes were extracted from two pre 24-hr recalls and one post dietary recalls collected using the regular EFNEP questionnaire form and following the standardized multiple pass method (Conway, 2003). The county community workers collected the dietary recalls, that were photocopied and mailed to the researchers for tabulation of fruit and vegetable servings according to ½ cup equivalents as defined by the U.S. Food Guide Pyramid (DHHS, 2000). Two days of intakes from the baseline were averaged for the servings of fruit and the serving of vegetables.
The Statistical Package for Social Science (SPSS, version 12.0 for Windows) was used for data analysis. The difference of the pregnant/lactating women and other community nutrition program participation and fruit and vegetable intakes were compared between control and experimental groups at the baseline using χ2-test and student's t-test, respectively. The differences in the servings of fruit and vegetable intakes by stage of readiness to eat fruit and vegetables were tested using Analysis of Variance, followed by Tukey's multiple comparison tests. Linear trend of fruit and vegetable intakes was also tested along with the stage of change. The differences of fruit and vegetable intakes before and after intervention in both control and experimental groups were tested by paired t-tests and MeNemar test. The movements of stage of change after intervention were examined by test of marginal homogeneity.
Community workers in the control county recruited 53 participants over the two month recruitment, and those in the experimental county recruited 90. At the baseline there were significant differences in age and race as well as participation in WIC (Table 1).
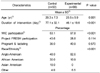
The age ranged from 17-65 years in the control country and 14-41 years in the experimental county. Women in the control county were older than those in the experimental county by about 4 years (p<0.001). The percentages of pregnant or lactating women were 36.0% in control and 40.9% in the experimental counties. About half (48.0%) of the women in the control county were Anglo-American (30.0% African-American and 18.0% Asian) compared to 82.6% in the experimental county (10.0% African American and no Asian). Nearly all of the women in the experimental county participated in WIC compared to 46% in the control county (p<0.001). Although there were differences in age, race, intervention duration and other community nutrition program participation between the control and experimental counties, the fruit and vegetable intakes from 2 dietary recalls did not significantly differ at the baseline (Table 2). Before intervention, the average servings of fruit and vegetables were 3.9 in the control and 4.1 in the experimental county. The percentages of subjects eating less than 5 servings of fruits and vegetables were 75.5% in the control and 61.4% in the experimental county. In dietary recall data not shown, the women who were pregnant or lactating did eat significantly more fruit and vegetables than those who were not pregnant or lactating by about one serving per day.
The intakes of fruit and vegetables differed among stages by ANOVA (Table 3) and between those in pre-contemplation, contemplation and preparation versus those in maintenance. There was a linear trend in consumption of fruit and vegetables with the Stage of Change (p<0.001). After intervention, participants in both counties significantly advanced in their stage of change by test of marginal homogeneity (Table 4). The percentage of people eating equal to or more than 5 servings was significantly increased in the experimental county (p<0.05, by McNemar test) but not in the control country. However, the average number of servings of fruit and vegetables were not significantly increased although about 1/2 serving of intakes were increased in both counties.
This study demonstrated that the ERIB3 curriculum enhanced with TTM derived processes to promote eating fruit and vegetables was effective in increasing the percentage of participants eating 5 or more servings of fruits and vegetables. The percentage of participants who advanced stages after the program increased, however, in both counties, demonstrated mixed results. Fruit and vegetable intakes were not increased significantly, although in both counties intakes were about ½ serving per day larger after intervention. There are several possible explanations such as unexpected baseline differences between counties, lack of power due to small sample size, and that the ERIB3 curriculum, either regular or TTM enhanced, was not intensive enough to produce the desired change specific to fruit and vegetables.
Our finding of an average baseline intake of about 4.0 servings of fruit and vegetables in the present study is similar to that reported by another study for WIC participants, but higher than that reported for young adults (Havas et al., 1998; Richards et al., 2006). Our findings of only 24-38% of women eating 5 or more servings of fruit and vegetables was somewhat lower than the 40% from the 1999-2000 National Health and Nutrition Examination Survey using 24 hour recall data (Guenther PM et al., 2006). Such findings support that women from limited income families are indeed a high risk group for low intakes of fruit and vegetables.
The linear trend observed in servings of fruit and vegetables from pre-contemplation to maintenance stage supports the validity of the TTM staging instrument. Recent studies using TTM to increase fruit and vegetables have expanded other aspects of the theoretical model to promote change such as the processes of change, self-efficacy and decisional balance (Greaney et al., 2004; Greene et al., 2004; Nitzke et al., in press; Henry et al., 2006). Interventions to promote eating fruits and vegetables based on TTM have been found to be effective in several studies (Havas et al., 2003; Perkins-Porras et al., 2005; Richards et al., 2006; Steptoe et al., 2003). Richards and colleagues reported a one serving increase of fruit and vegetable consumption in young adults (Richards et al., 2006). Two other studies with larger samples reported increased consumption by approximately 0.5 servings per day (Havas et al., 1998; Nitzke, in press) which was similar in size to our findings.
There were several strengths to this study. The study adapted an existing intervention program for use with limited income families with children having potential for wide replication and distribution. The intervention was based on a theory of health behavior change and used established instruments, facilitating comparisons and targeting curriculum improvements. The intervention enhancements were developed based not only on the literature but also in conjunction with county community level practitioners. The baseline differences were unanticipated given the similarity in county demographics. Upon reflection, this might have been due to striking differences in the demographics of the community workers. Community workers in the intervention county were 8 Anglo-American and one African American in contrast to those in the control county with 4 Anglo-American; 3 African American, one Hispanic and one Asian American. The greater diversity of participants in the control county likely reflected the greater diversity of community workers there. The high percentage of pregnant and lactating mothers in the sample was not anticipated and might have also influenced the findings. Another limitation was the inability to control the duration of intervention, so that it was three-fourths longer in the control than in the experimental county. Finally, although we used an instrument well accepted at the time, assessing stage of change separately for fruit and for vegetables is now a more accepted practice in nutrition education.
In conclusion, we encourage health professionals to apply lessons learned from this intervention and continue to pursue theoretically based interventions to change dietary behaviors. More intensive programs enhancing access to low cost fruit and vegetables and/or reducing barriers to intake are likely to be needed to improve intakes enough to reduce dietary risk for chronic diseases.
Figures and Tables
Table 2
EFNEP participants" fruit and vegetable intakes from dietary recalls and from stage of change instrument (Glanz, 1994) at baseline (n=143)
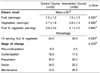
Table 3
Total servings of fruit and vegetables from two dietary recalls by stage of change at baseline (n=143)

Table 4
Percentages in stage of change for fruit and vegetables plus fruit and vegetable servings from dietary recalls before (2 days) and after intervention (1 day) (n=143)

1)p value between before and after intervention by test of marginal homogeneity in control
2)p value between before and after intervention by test of marginal homogeneity in experimental
3)p value between before and after intervention by McNemar test in control
4)p value between before and after intervention by McNemar test in experimental
5)p value between before and after intervention by paired t-test in control
6)p value between before and after intervention by paired t-test in experimental
Acknowledgements
The authors would to thank Gayle Coleman, MS, RD, Nutrition Education Program Specialist at University of Wisconsin Extension (at Michigan State University Extension at the time of the study) for her assistance with developing intervention materials and Won O Song, PhD, RD, MPH, professor at Michigan State University, as co-investigator on the project. We are grateful to the Extension Home Economists and EFNEP paraprofessionals in Ingham and Kent Counties, Michigan, USA, for assistance with development and delivery of the intervention and the data collection. This research was supported, in part, by a grant from the Michigan Public Health Institute (MPHI) and the Michigan Department of Community Health (MDCH). The second author was supported in part by the Michigan Agricultural Experiment Station.
References
1. Achterberg C, Miller C. Is one theory better than another in nutrition education? A viewpoint: more is better. J Nutr Educ Behav. 2004. 36:40–42.

2. Algert SJ, Agrawal A, Lewis DS. Disparities in access to fresh produce in low-income neighborhoods in Los Angeles. Am J Prev Med. 2006. 30:365–370.

3. Briefel RR, Johnson CL. Secular trends in dietary intake in the United States. Annu Rev Nutr. 2004. 24:401–431.

4. Bremner B, Campbell CC, Sobal J. Comparison of the beliefs and practices of EFNEP clients with staff perceptions of clients. J Nutr Educ. 1994. 26:123–130.

5. Conway JM, Ingwerson LA, Vinyard BT, Moshfegh AJ. Effectiveness of the US Department of Agriculture 5-step multiple pass method in assessing food intake in obese and nonobese women. Am J Clin Nutr. 2003. 77:1171–1187.
6. Department of Health & Human Services. Healthy People 2010. 2000. 2nd ed. Washington DC, US: US Government Printing Office, USA.
7. Dietray Guidelines for Americans 2005. Department of Health & Human Services & Department of Agriculture. 2005. Accessed on 3/20/2007.
www.healthierus.gov/dietaryguidelines.
8. Frazao E. The American diet, health and economic consequences (AIB-711). 1995. Washington. USA: Economic Research Service.
9. Glanz K, Rimer BK, Lewis FM, editors. Health Behavior and Health Education-Theory, Research and Practice. 2002. San Francisco. USA: Josey-Bass.
10. Glanz K, Patterson RE, Kristal AR, DiClemente CC, Heimendinger J, Linnan L, McLerran DF. Stage of change in adopting healthy diets: fat, fiber, and correlates of nutrient intake. Health Educ Q. 1994. 21:499–519.

11. Greaney ML, Less FD, Greene GW, Clark PG. What older adults find useful for maintaining health eating and exercise habits. J Nutr Elder. 2004. 24:19–35.

12. Greene GW, Fey-Yensan N, Padula C, Rossi S, Rossi JS, Clark PG. Differences in psychosocial variables by stage of change for fruits and vegetables in older adults. J Am Diet Assoc. 2004. 104:1236–1243.

13. Guenther PM, Dodd KW, Reedy J, Krebs-Smith SM. Most Americans eat much less than recommended amounts of fruits and vegetables. J Am Diet Assoc. 2006. 106:1371–1379.

14. Havas S, Anliker J, Damron D, Langenberg P, Ballesteros M, Feldman R. Final results of the Maryland WIC 5-A-Day Promotion Program. Am J Pub Health. 1998. 88:1161–1167.

15. Havas S, Anliker J, Greenberg D, Block G, Block T, Blik C, Langenberg P, DiClemente C. Final results of the Maryland WIC Food for Life Program. Prev Med. 2003. 37:406–416.

16. Henry H, Reimer K, Smith C, Reicks M. Associations of decisional balance, processes of change, and self-efficacy with stages of change for increased fruit and vegetable intake among low-income, African-American mothers. J Am Diet Assoc. 2006. 106:841–849.

17. Johnson DB, Beaudoin S, Smith LT, Beresford SA, LoGerfo JP. Increasing fruit and vegetable intake in homebound elders: the Seattle Senior Farmers' Market Nutrition Pilot Program. Prev Chronic Dis. 2004. 1:A03.
18. Kasila K, Poskiparta M, Karhila P, Kettunen T. Patients' readiness for dietary change at the beginning of counseling: a transtheoretical model-based assessment. J Hum Nutr Diet. 2003. 16:159–166.

19. Eating Right is Basic III, 1995. Michigan State University Extension. 2005. Accessed on 3/20/2007.
http://www.fcs.msue.msu.edu/EFNEP/catalog/index.htm.
20. Nitzke S, Kritsch K, Boeckner L, Greene G, Hoerr S, Kattelmann K, Lohse B, Oakland MJ, Phillips B, White A. A stage-tailored multi-modal intervention increases fruit and vegetable intakes f low-income young adults. American Journal of Health Promotion. (in press).
21. New York State Cornell Cooperative Extension. EFNEP Guidelines Cornell Cooperative Extension. 1998. Ithaca. NY:
22. Theory at a Glance. National Institutes of Health, National Cancer Institute. 2005. 09. Accessed on 3/20/2007.
http://cancer.gov/cancerinformation/theory-at-a-glance.
23. Perkins-Porras L, Cappuccio FP, Rink E, Hilton S, McKay C, Steptoe A. Does the effect of behavioral counseling on fruit and vegetable intake vary with stage of readiness to change? Prev Med. 2005. 40:314–320.

24. Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: Applications to addictive behaviors. Am Psychol. 1992. 47:1102–1114.

25. Richards A, Kattelmann KK, Ren C. Motivating 18- to 24-year-olds to increase their fruit and vegetable consumption. J Am Diet Assoc. 2006. 106:1405–1411.

26. Serdula M, Coates R, Byers T, Mokdad A, Jewell S, Chavez N, Mares-Perlman J, Newcomb P, Ritenbaugh C, Treiber F, Block G. Evaluation of a brief telephone questionnaire to estimate fruit and vegetable consumption in diverse study populations. Epidemiology. 1993. 4:455–463.

27. Sporny LA, Contento IR. Stages of Change in dietary fat reduction: social psychological correlates. J Nutr Educ. 1995. 27:191–199.

28. Steptoe A, Perkins-Porras L, McKay C, Rink E, Hilton S, Cappuccio FP. Psychological factors associated with fruit and vegetable intake and with biomarkers in adults from a low-income neighborhood. Health Psychol. 2003. 22:148–155.

29. Subar AF, Heimendinger J, Patterson BH, Krebs-Smith SM, Pivonka E, Kessler R. Fruit and vegetable intake in the United States: The baseline survey of the Five a Day for better health program. Am J Health Promot. 1995. 9:352–360.

30. Van Duyn MA, Heimendinger J, Russek-Cohen E, DiClemente CC, Sims LS, Subar AF, Kreb-Smith SM, Pivonka E, Kahle LL. Use of the transtheoretical model of change to successfully predict fruit and vegetable consumption. J Nutr Educ. 1998. 30:371–380.

31. Wellman NS, Kamp B, Kirk-Sanchez NJ, Johnson PM. Eat better & move more: a community-based program designed to improve diets and increase physical activity among older Americans. Am J Public Health. 2007. 97:710–717.

32. Zenk SN, Schulz AJ, Hollis-Neely T, Campbell RT, Holmes N, Watkins G, Nwankwo R, Odoms-Young A. Fruit and vegetable intake in African Americans : income and store characteristics. Am J Prev Med. 2005. 29:1–9.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download