Abstract
This study aims to investigate the nutritional status of night eaters using the data from 2005 Korean National Health and Nutrition Examination Survey. A total of 3,903 subjects aged 20 and above were divided into 3 groups by using 24-hr recall data according to the night snack calorie intake: non-night snack, night snack less than 500 kcal and 500 kcal and more. Their data were analyzed to find out the difference on the socio-demographic, anthropometric, blood pressure, blood parameters and dietary characteristics. Among the subjects, non-night eaters were 66.0%, night eaters of less than 500 kcal were 28.4% and 500 kcal and above were 5.6%. Male adults, young-aged, higher educated, higher income earner, breakfast skipper and frequent dine-outer (3 times and more a day) were found more in the night eaters with 500 kcal and above. Night eaters above 500 kcal showed higher waist circumference, Glu-FBS, Glu-PP120 and also showed higher daily intake of fat and alcohol per 1,000 kcal and food groups of meat & eggs, beverages and alcohol drinks (p < 0.05), while they showed the lowest carbohydrate energy ratio of 58.3 ± 13.7 among the three groups. These results suggest that habitual night snack intake above 500 kcal could lead to abdominal obesity and diabetes due to higher intake of meat, fat and alcohol.
Figures and Tables
Table 2
Anthropometric characteristics of the subjects by night snack calorie intake and their correlation coefficients
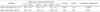
Table 4
Blood pressure and concentration of blood parameters of the subjects by night snack calorie intake and their correlation coefficients
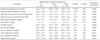
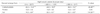
Table 6
Monthly frequency of food group intake by night snack calorie intake of the subjects and their correlation coefficients

Table 7
Daily mean nutrients intake per 1,000 kcal by night snack calorie intake of the subjects and their correlation coefficients

1) Measured by ANOVA test 2) Measured by ANCOVA test adjusted by age and gender 3) Partial correlation coefficients adjusted by age and gender 4) Mean ± SD 5) Different small alphabet letters are significantly different by Duncan's multiple range test 6) Not adjusted by energy intake
*: p < 0.05, **: p < 0.01, ***: p < 0.001
References
1. Hubert HB, Feinleib M, McNamara PM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation. 1983. 67(5):968–977.

2. Posner BM, Franz M, Quatromoni P. Nutrition and the global risk for chronic diseases: the INTERHEALTH nutrition initiative. The INTERHEALTH Steering Committee. Nutr Rev. 1994. 52(6):201–207.

3. Ministry of Health and Welfare, Korea Health Statistics 2009: Korean National Health and Nutrition Examination Survery. 2010. Cheongwon: Korea Centers for Disease Control and Prevention;442–444.
4. Kim K, Lee W, Lee S, Ann N, Oh H, Sin Y, Park J, Hong C, Kim S, Kim E, Lee J, Kim E, Jang J. Health status and lifestyle including diet, exercise, and daily activities in obese adults. Korean J Sports Med. 2005. 23(1):54–63.
5. Stunkard AJ, Grace WJ, Wolff HG. The night-eating syndrome; a pattern of food intake among certain obese patients. Am J Med. 1955. 19(1):78–86.
6. Birketvedt GS, Florholmen J, Sundsfjord J, Osterud B, Dinges D, Bilker W, Stunkard A. Behavioral and neuroendocrine characteristics of the night-eating syndrome. JAMA. 1999. 282(7):657–663.

7. Vetrugno R, Manconi M, Ferini-Strambi L, Provini F, Plazzi G, Montagna P. Nocturnal eating: sleep-related eating disorder or night eating syndrome? A videopolysomnographic study. Sleep. 2006. 29(7):949–954.

8. Lundgren JD, Allison KC, Crow S, O'Reardon JP, Berg KC, Galbraith J, Martino NS, Stunkard AJ. Prevalence of the night eating syndrome in a psychiatric population. Am J Psychiatry. 2006. 163(1):156–158.

9. Lundgren JD, McCune A, Spresser C, Harkins P, Zolton L, Mandal K. Night eating patterns of individuals with eating disorders: implications for conceptualizing the night eating syndrome. Psychiatry Res. 2011. 186(1):103–108.

10. Allison KC, Stunkard AJ. Obesity and eating disorders. Psychiatr Clin North Am. 2005. 28(1):55–67.

11. Striegel-Moore RH, Franko DL, Thompson D, Affenito S, Kraemer HC. Night eating: prevalence and demographic correlates. Obesity (Silver Spring). 2006. 14(1):139–147.

12. Adami GE, Meneghelli A, Scopinaro N. Night eating syndrome in individuals with Mediterranean eating-style. Eat Weight Disord. 1997. 2(4):203–206.

13. Marshall HM, Allison KC, O'Reardon JP, Birketvedt G, Stunkard AJ. Night eating syndrome among nonobese persons. Int J Eat Disord. 2004. 35(2):217–222.

14. Stunkard AJ, Allison KC. Two forms of disordered eating in obesity: binge eating and night eating. Int J Obes Relat Metab Disord. 2003. 27(1):1–12.

15. Jung HJ, Park KH, Cho YG, Cho JJ, Paek YJ, Song HJ, Byun JS. Night eating tendency and related health risk factors. Korean J Obes. 2006. 15(2):98–105.
16. Birketvedt GS, Sundsfjord J, Florholmen JR. Hypothalamic-pituitary-adrenal axis in the night eating syndrome. Am J Physiol Endocrinol Metab. 2002. 282(2):E366–E369.
17. Aronoff NJ, Geliebter A, Zammit G. Gender and body mass index as related to the night-eating syndrome in obese outpatients. J Am Diet Assoc. 2001. 101(1):102–104.

18. Gluck ME, Geliebter A, Satov T. Night eating syndrome is associated with depression, low self-esteem, reduced daytime hunger, and less weight loss in obese outpatients. Obes Res. 2001. 9(4):264–267.

19. Lee SH, Kim KJ. The comparison of the physical fitness and eating habits between abdominal obese and lower limb obese in middle-aged women. Korean J Sports Sci. 2004. 13(1):585–600.
20. Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. In-depth analysis on the 3rd Korea National Health and Nutrition Examination Survey. 2005. Cheongwon: Korea Centers for Disease Control and Prevention.
21. Spaggiari MC, Granella F, Parrino L, Marchesi C, Melli I, Terzano MG. Nocturnal eating syndrome in adults. Sleep. 1994. 17(4):339–344.

22. Greeno CG, Wing RR, Marcus MD. Nocturnal eating in binge eating disorder and matched-weight controls. Int J Eat Disord. 1995. 18(4):343–349.

23. Park JG, Jang CJ, Lee TY, Park YS. Health statistics. 2008. Seoul: Gyechuk Cultural Press.
24. Grilo CM, Masheb RM. Night-time eating in men and women with binge eating disorder. Behav Res Ther. 2004. 42(4):397–407.

25. Choi MK, Kim JM, Kim JG. A study on the dietary habit and health of office workers in Seoul. Korean J Food Cult. 2003. 18(1):45–55.
26. Colles SL, Dixon JB, O'Brien PE. Night eating syndrome and nocturnal snacking: association with obesity, binge eating and psychological distress. Int J Obes (Lond). 2007. 31(11):1722–1730.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download