Abstract
High sodium intake is one of the risk factors for the development of hypertension. According to 2007 Korean National Health and Nutrition Examination Survey, sodium intake of Korean was three times higher than adequate intake (1.5 g/day) recommended by Korean Dietary Reference Intakes. High sodium intake is related to high threshold and preference of salty taste. And zinc status is known to affect taste acuity. The hypothesis of this study is that zinc status is associated with salty taste acuity, preference, sodium intake and blood pressure. The subjects included in this study were 50 men and 41 women aged 20-29 y who did not smoke and not take supplements or medications regularly. Dietary intake data for 3 days were collected by 24-h recall for 1 day and dietary record for 2-days. Salty taste acuity and preference were determined by sensory test. Fasting serum concentration of zinc, height, weight, body composition and blood pressure data were collected. Salt taste preference in high zinc intake group (≥ estimated average requirement, EAR; men-8.1 mg/day, women-7 mg/day) was higher than that in low zinc intake group (< EAR). Salty taste preference was inversely correlated with serum zinc concentration in people with low concentration of serum zinc (≦ 81µg/dL)(r = -0.3520, p < 0.05). Diastolic blood pressure was higher in high sodium intake group than in low sodium intake group (p < 0.05), positively correlated with salty taste preference (r = 0.3866, p < 0.05) in subjects with daily zinc intake below the EAR. We conclude that low zinc status may be related to high salty taste preference and high blood pressure in Korean young adults.
Figures and Tables
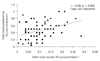
Fig. 4
Relationship between salty taste preference and serum zinc. A: Low serum zinc (n = 46). B: Normal serum zinc (n = 45).

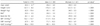
Table 4
Salty taste and blood pressure of subjects by sodium intake

1) < Median (3,500 mg/day)
2) The p-value were calculated by ANCOVA (age, sex adjusted for salty taste; age, sex, BMI adjusted for blood pressure)
3) < Median (1,920 mg/1,000 kcal)
4) Mean ± SD
5) SBP: Systolic blood pressure, DBP: Diastolic blood pressure, MAP: Mean arterial pressure [DBP + (SBP-DBP)/3]
References
1. Korea Centers for Disease Control and Prevention. The Fourth Korea National Health and Nutrition Examination Survey (KNHANES IV). 2008.
2. Korea National Statistical Office. 2008 Annual Report on the Cause of Death Statistics. 2009.
3. Morgan SL, Strong DC, Kitchin EM, Johnston KE, Disilvestro RA, Tamura T. Zinc status of women with low bone mineral density who receive calcium supplements. Biol Trace Elem Res. 2006. 110(3):211–222.

4. He J, Gu D, Chen J, Jaquish CE, Rao DC, Hixson JE, Chen JC, Duan X, Huang JF, Chen CS, Kelly TN, Bazzano LA, Whelton PK. Gender difference in blood pressure responses to dietary sodium intervention in the GenSalt study. J Hypertens. 2009. 27(1):48–54.

5. de Wardener HE, MacGregor GA. Harmful effects of dietary salt in addition to hypertension. J Hum Hypertens. 2002. 16(4):213–223.

6. Sanders PW. Dietary salt intake, salt sensitivity, and cardiovascular health. Hypertension. 2009. 53(3):442–445.

7. McLaughlin B, Kevany J. A pilot investigation into the effect of a shot-term restriction in sodium intake on blood pressure, sodium chloride taste threshold and the problems associated with such a dietary restriction. Ir J Med Sci. 1983. 152(11):399–403.
8. Pimenta E, Gaddam KK, Oparil S, Aban I, Husain S, Dell'Italia LJ, Calhoun DA. Effects of dietary sodium reduction on blood pressure in subjects with resistant hypertension: results from a randomized trial. Hypertension. 2009. 54(3):475–481.

9. The Korean Nutrition Society. Dietary Reference Intakes for Koreans. 2005. Seoul:
10. Kim YS, Paik HY. Measurement of Na intake in Korean Adult Female. Korean J Nutr. 1987. 20(5):341–349.
11. Kim KS, Paik HY. A Comparative Study on Optimum Gustation of Salt and Sodium Intake in Young and Middle-Aged Korean Women. Korean J Nutr. 1992. 25(1):32–41.
12. Bertino M, Beauchamp GK, Engelman K. Long-term reduction in dietary sodium alters the taste of salt. Am J Clin Nutr. 1982. 36(6):1134–1144.

13. Kim JY, Kang YR, Lee MY, Paik HY. Sodium Intake and Preference for Salty Taste in Elementary School Children Residing in Rural and Urban Areas of Korea. Korean J Nutr. 1990. 23(4):248–256.
14. Isezuo SA, Saidu Y, Anas S, Tambuwal BU, Bilbis LS. Salt taste perception and relationship with blood pressure in type 2 diabetics. J Hum Hypertens. 2008. 22(6):432–434.

15. Rabin M, Poli de Figueiredo CE, Wagner MB, Antonello IC. Salt taste sensitivity threshold and exercise-induced hypertension. Appetite. 2009. 52(3):609–613.

16. Ueda C, Takaoka T, Sarukura N, Matsuda K, Kitamura Y, Toda N, Tanaka T, Yamamoto S, Takeda N. Zinc nutrition in healthy subjects and patients with taste impairment from the view point of zinc ingestion, serum zinc concentration and angiotensin converting enzyme activity. Auris Nasus Larynx. 2006. 33(3):283–288.

17. McDaid O, Stewart-Knox B, Parr H, Simpson E. Dietary zinc intake and sex differences in taste acuity in healthy young adults. J Hum Nutr Diet. 2007. 20(2):103–110.

18. Do MS, Lomeda RAR, Cho YE, Kwun IS. Original Research: The decreased molar ratio of phytate: zinc improved zinc nutriture in South Koreans for the past 30 years (1969-1998). Nutr Res Pract. 2007. 1(4):356–362.

19. Fisher S, Hendricks DG, MaHoney AW, Nutritional assessment. Nutritional assessment of senior rural Utahans by biochemical and physical measurements. Am J Clin Nutr. 1978. 31(4):667–672.

20. Koo NS. Sensory evaluation. 2006. Seoul: Kyomunsa.
21. Human Nutrition Lab Department of Food and Nutrition, Seoul National University and AI/DB Lab, Sookmyung Womens University. DS24. 1996.
22. Stewart-Knox BJ, Simpson EE, Parr H, Rae G, Polito A, Intorre F, Meunier N, Andriollo-Sanchez M, O'Connor JM, Coudray C, Strain JJ. Zinc status and taste acuity in older Europeans: the ZENITH study. Eur J Clin Nutr. 2005. 59:Suppl 2. S31–S36.

23. Stewart-Knox BJ, Simpson EE, Parr H, Rae G, Polito A, Intorre F, Andriollo Sanchez M, Meunier N, O'Connor JM, Maiani G, Coudray C, Strain JJ. Taste acuity in response to zinc supplementation in older Europeans. Br J Nutr. 2008. 99(1):129–136.

24. Yoon JS, Lee JH, Park PS. Zinc Status and Taste Acuity of Old and Young Women. Korean J Community Nutr. 2000. 5(3):484–492.
25. Pangborn RM, Pecore SD. Taste perception of sodium chloride in relation to dietary intake of salt. Am J Clin Nutr. 1982. 35(3):510–520.

26. Kusaba T, Mori Y, Masami O, Hiroko N, Adachi T, Sugishita C, Sonomura K, Kimura T, Kishimoto N, Nakagawa H, Okigaki M, Hatta T, Matsubara H. Sodium restriction improves the gustatory threshold for salty taste in patients with chronic kidney disease. Kidney Int. 2009. 76(6):638–643.

27. Blais CA, Pangborn RM, Borhani NO, Ferrell MF, Prineas RJ, Laing B. Effect of dietary sodium restriction on taste responses to sodium chloride: a longitudinal study. Am J Clin Nutr. 1986. 44(2):232–243.

28. Li N, Prescott J, Wu Y, Barzi F, Yu X, Zhao L, Neal B. The effects of a reduced-sodium, high-potassium salt substitute on food taste and acceptability in rural northern China. Br J Nutr. 2009. 101(7):1088–1093.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download