Abstract
A 62-year-old woman has been suffered from cavernous sinus thrombophlebitis which was confirmed by four-vessel angiography, orbit magnetic resonance imaging, and blood culture. Three weeks after recovery of cavernous sinus thrombophlebitis, right eye proptosis and complete third, fourth, and sixth cranial nerve palsies developed. Best-corrected visual acuity decreased to 20/70 in the right eye. Repeat magnetic resonance imaging demonstrated a 1.5-cm-sized mass in the right cavernous sinus, suspicious for mycotic aneurysm. Amphotericin B supplementation was begun and was followed by successful transarterial Guglielmi detachable coil embolization. Four months later, extraocular movement was normalized, and visual acuity improved to 20/25 in the right eye.
Mycotic aneurysm is a rare complication of cavernous sinus thrombosis and may be treated with antibiotics, carotid ligation, internal carotid artery balloon occlusion, or Guglielmi detachable coil (GDC) embolization [1]. However, a complete visual recovery from a mycotic aneurysm associated with cavernous sinus thrombophlebitis after endovascular coiling has not been reported in the English literature. We describe a case of mycotic aneurysm complicated by cavernous sinus thrombosis, which was successfully treated with coil embolization and resulted in a complete visual recovery.
A 62-year-old woman presented with diplopia for a period of one day. She had a continuous headache for five days and fever of 38.7℃. She was receiving medication for hypertension but denied any history of trauma, viral infection, or any other systemic disease.
Best corrected visual acuity (BCVA) was 20/25 in the right eye and 20/20 in the left eye. She showed abduction limitation to 20% of the normal range in the right eye. Pupillary light reflex was normal without relative afferent pupillary defect. A blood test showed elevated serum erythrocyte sediment rate (79 mm/hr) and elevated C-reactive protein (14.79 mg/dL). The right cavernous sinus was enhanced in an orbital magnetic resonance imaging test (Fig. 1). A delayed view of four-vessel angiography showed venous engorgement and stasis in the right cavernous sinus, both of which are consistent with thrombophlebitis of the cavernous sinus (Fig. 2A).
Dental examination revealed a limitation of mouth opening (28 mm) and periodontitis in the right lower wisdom tooth. When Gram negative coccobacilli were found in the blood culture, intravenous ceftriaxone, cefuroxime, and metronidazole were started, and heparinization was administered. Fourteen days from the first visit, Fusobacterium was finally isolated. Extraocular movement and general status improved after the systemic antibiotic treatment.
One month from the first visit, right eye proptosis suddenly developed. In the right eye, BCVA decreased to 20/70, and complete third, fourth, and sixth cranial nerve palsies developed. The right eyeball was deviated slightly downward and inward. The pupil was dilated, and no light reflex was demonstrated in the right eye. The superior and temporal visual field was impaired in the right eye. Soft exudates and splinter hemorrhage were noted upon fundus examination of the right eye (Fig. 2B). Four-vessel angiography demonstrated a newly defined 1.5-cm-sized mass in right cavernous sinus, suspicious for mycotic aneurysm (Fig. 2C). The patient was treated with amphotericin B (1 mg/kg).
After systemic status improved, the mycotic aneurysm was completely occluded with transarterial GDC (Boston Scientific Corp., Fremont, CA, USA) embolization without complication. Ten days after the embolization, follow-up angiography showed no evidence of residual aneurysm in the cavernous sinus (Fig. 2D). Four months later, extraocular movement was normalized, and visual acuity improved to 20/25 in the right eye.
The mechanism of mycotic aneurysm formation is thought to be due to hematogenous spread of infectious microemboli to the vasa vasorum, occlusion by an infected embolus of a distal artery lumen, or contiguous spread from an extavascular infection, such as sinusitis, orbital infection, or middle ear infection [2]. However, a case complicated by cavernous sinus thrombophlebitis is much rarer, with about only 20 cases reported.
Mycotic aneurysm in the cavernous sinus may present as ophthalmoplegia, diplopia, orbital swelling, and/or visual disturbance. Quisling et al. [3] have reported a case of blindness which resulted from enlarging mycotic aneurysm after cavernous sinus thrombosis.
Several treatments, such as antibiotic therapy, carotid ligation, internal carotid artery balloon occlusion, and GDC embolization have been adopted to treat mycotic aneurysms in the cavernous sinus [1,4]. The GDC embolization, first used for patients with aneurysm in 1991 [5], prevents blood flow into the aneurysmal sac by filling the aneurysm with coils and thrombus. Although GDC embolization may be complicated by thromboembolism, intra-operative aneurysm rupture, coil migration, bacteremia and vasospasm, our patient showed a complete recovery of vision and motility without complication.
This is the first case of complete visual recovery after mycotic aneurysm embolization complicated by cavernous sinus thrombophlebitis showing a possibility of successful treatment with GDC embolization without any complications.
Figures and Tables
Fig. 1
Gadolinium-enhanced magnetic resonance imaging shows enhancement in the right cavernous sinus in the fat-suppressed T1-weighted axial image (A) and T1-weighted sagittal image (B).
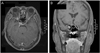
Fig. 2
(A) Four-vessel angiography reveals that the cavernous sinus is not filled in the delayed views, and venous engorgement and stasis are shown (arrow). (B) Soft exudates and splinter hemorrhage are noted upon fundus examination. (C) Mycotic aneurysm is located at the cavernous sinus portion upon digital four-vessel angiography (arrow). (D) Guglielmi detachable coil embolization is performed successfully without the remaining aneurysm (arrow).

Acknowledgements
This work was supported by grant No. R01-2005-000-10875-0 from the Basic Research Program of the Korea Science & Engineering Foundation.
References
1. Hurst RW, Choi IS, Persky M, Kupersmith M. Mycotic aneurysms of the intracavernous carotid artery: a case report and review of the literature. Surg Neurol. 1992. 37:142–146.
2. Wilson WR, Hawrych A, Olan W. Rapid development of bilateral internal carotid artery aneurysm from sphenoid sinus aspergillosis. Skull Base Surg. 1998. 8:211–214.
3. Quisling SV, Mawn LA, Larson TC 3rd. Blindness associated with enlarging mycotic aneurysm after cavernous sinus thrombosis. Ophthalmology. 2003. 110:2036–2039.
4. Koebbe CJ, Veznedaroglu E, Jabbour P, Rosenwasser RH. Endovascular management of intracranial aneurysms: current experience and future advances. Neurosurgery. 2006. 59:5 Suppl 3. S93–S102.
5. Guglielmi G, Vinuela F, Dion J, Duckwiler G. Electrothrombosis of saccular aneurysms via endovascular approach. Part 2: Preliminary clinical experience. J Neurosurg. 1991. 75:8–14.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download